Autologous Reconstruction: Gluteal Flap Breast Reconstruction
Michael R. Zenn
Indications
Autogenous tissue reconstruction of the breast by utilizing gluteal tissues is indicated in any woman with a partial or complete deformity of the breast. There must be adequate tissue in the gluteal area to match the requirements for breast reconstruction. Gluteal tissues are a solid second or third choice for autologous breast reconstruction after abdominal-based tissue reconstructions (transverse rectus abdominis myocutaneous (TRAM), deep inferior epigastric perforator (DIEP), superficial inferior epigastric artery (SIEA)) or possibly back tissues (latissimus flaps). Although abdominal-based flaps are usually more popular for donor site cosmetic reasons, patients without sufficient abdominal tissue or previous abdominal surgery are often ideally suited for gluteal reconstruction. This often includes patients requiring bilateral reconstruction such as prophylactic mastectomy patients who do not have adequate tissue in the abdomen for two reconstructions. Patients seeking gluteal flap reconstruction as a general rule wish to avoid the use of synthetic implants. They are willing to accept a scar in a location that is well hidden and not easily visible to themselves.
Advantages
Faster recovery than with abdominal flaps (TRAM, DIEP).
No risk of abdominal hernias or bulges.
Good projection of the reconstruction.
There is less postoperative discomfort than with abdominal-based flaps.
Contraindications
Patients who are in poor health who would be at risk for a prolonged surgical procedure under a general anesthesia.
Extreme obesity where the blood supply to the buttock tissues may be hard to localize and capture in the flap (body mass index > 30).
Lack of recipient site inflow vessels (internal mammary artery, thoracodorsal artery).
Relative Contraindications
Smokers, because of the vasoconstrictive effects of nicotine, who have higher incidence of wound healing problems, especially at the donor site.
Inadequate tissue for reconstruction.
Previous surgery in the area of the gluteus.
Large breast reconstructions (larger than a C cup).
Unwillingness to have scar or deformity of the gluteal area.
Patients who will be having postoperative radiation therapy as part of their cancer care. In this case, reconstruction will be delayed until after radiation to avoid radiation damage to the reconstructed breast.
Workup for gluteal flap surgery for breast reconstruction starts with a thorough history and physical examination taking into account potential for local, regional, and metastatic disease. Areas of previous surgery or injury at the donor or recipient sites should be closely examined. From the general medical standpoint, patients should be screened for poorly controlled diabetes, cardiac disease, pulmonary disease, and renal disease. These procedures are major undertakings and do not warrant unnecessary morbidity. Remember, patients can always forego a lengthy and possibly risky surgery and use an external prosthesis. A history of smoking is not an absolute contraindication but does say something about the patient’s ability and willingness to take an active role in her care and do something to ensure success. Although smoking does not cause gluteal flap failures, the vasoconstrictive effects of nicotine have been shown to cause necrosis of mastectomy flaps and buttock wound healing problems. Chronologic age is probably less important that physiologic age. As a general rule, these procedures are not offered to patients in their 70s or older.
The issue of radiation therapy as part of the patient’s adjuvant therapy deserves special mention. It has been shown convincingly that radiation of a soft tissue reconstructive flap can potentially cause adverse effects on that tissue that include firmness, distortion, pain, and even failure of the reconstruction. It is for this reason that patients who require radiation for their cancer care should have their gluteal flaps delayed, preferably 6 months or more after their radiation treatment. Reconstruction in the irradiated chest wall field has the same success rate as in a nonirradiated case but has the advantage of placing soft, supple, nonirradiated tissue on the chest for a more durable reconstruction. It should be noted that once a patient has been irradiated, contracture and induration of the chest wall skin may increase skin requirements for reconstruction, making the gluteal flap less useful or limiting its ultimate size.
Finally, preoperative evaluation should include evaluation of the contralateral breast in cases of unilateral reconstruction. Ultimately, the goal of reconstruction is to enable a patient to achieve symmetry in clothes. Absolute symmetry out of clothes is unrealistic and, if present, will not stand the test of time as each breast mound will respond differently to physiologic and physical changes over time. For patients with large or ptotic breasts, there should be a willingness for contralateral surgery for symmetry to best match the configuration of the gluteal flap reconstruction. This would include mastopexy or breast reduction. In a bilateral reconstruction, it is somewhat easier to match sides since the composition of the breast reconstructions will be similar. With that said, matching in clothes remains the standard.
No studies need to be performed preoperatively to evaluate the recipient site or the donor site vessels. Because of the extensive nature of this procedure, bilateral cases are performed only if two microsurgeons are available. Most surgeons will do one side at a time, separated by 4 to 6 months.
Relevant Anatomy
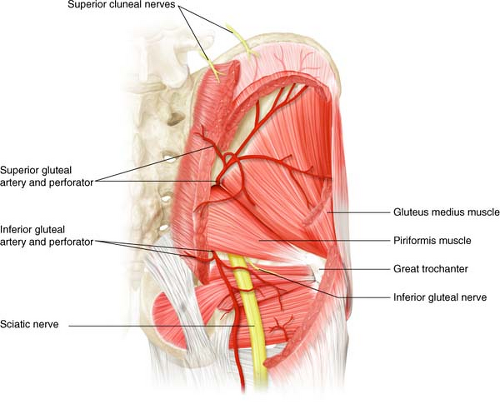
Gluteal tissues can be carried on one of two vascular supplies: the superior gluteal artery or the inferior gluteal artery (Fig. 31.1). Gluteal-based flaps were first described as myocutaneous flaps where a block of tissue from the buttock was carried with underlying gluteus maximus muscle and the gluteal blood vessels. This is no longer practiced as the muscle is unnecessary for vascular supply of the buttock skin and fat. These flaps are based on the perforating vessels of the inferior and superior gluteal arteries, so-called perforator flaps. The SGAP (superior gluteal artery perforator) and IGAP (inferior gluteal artery perforator) flaps are the current standard for gluteal-based flaps. Which flap is used is determined by the distribution of excess fat and skin in that particular patient. Both flaps have the advantage of a longer pedicle length than their muscle-bound relative since the dissection of the intramuscular course adds to the ultimate length of the pedicle, facilitating microsurgery. By not harvesting muscle with the flap, the SGAP and IGAP flaps also minimize morbidity by maintaining muscle strength and integrity.
SGAP flaps are much more commonly performed than IGAP flaps for the following reasons:
Improved donor site aesthetic. The incision and tissue removal is similar to a buttock lift and leaves the buttock with good contour.
Adequate pedicle length. Since gluteal muscle is not taken, the ultimate length of the perforating blood vessels off the superior gluteal artery are more than adequate for reanastomoses and placement of the flap in the proper position. This was the limiting factor to using superiorly based gluteal flaps when muscle was included.
The inferior gluteal artery is intimately associated with the posterior femoral cutaneous nerve supplying sensation to the posterior thigh and the motor nerve to the
entire gluteus muscle (inferior gluteal nerve). By avoiding these completely, one limits the potential morbidities caused by their injury.
With all that said, the IGAP should be entertained in those patients whose fat and skin distribution is mainly in the lower buttock area.
Relevant muscles in this area are as follows:
The gluteus maximus muscle. The gluteus maximus is quadrangular in shape. It originates from the bony pelvis and inserts into the gluteal tuberosity of the femur. It is a powerful extensor and is important in activities such as standing from a squatting position, heel walking, and climbing stairs. Perforating vessels of the superior and inferior gluteal artery perforate this muscle, supplying the overlying skin and fatty tissue.
The piriformis muscle lies beneath the gluteus muscle. It arises from the sacrum and inserts into the greater trochanter. The superior gluteal vessels emerge superior to it and the inferior gluteal vessels inferior to it.
There are multiple perforators from each vessel through the muscle but only one perforator is required to ensure vascularization of the flap. Cutaneous nerve supply to the buttock is via the nervi clunii superioris, which are branches of the lumbar nerves. They can be identified at the superior margin of the gluteal artery perforator flap and, if found large enough, can be raised with the flap to innervate the gluteal flap and give sensation to reconstruction.
Surgical Marking
Markings for the gluteal flap are made in the standing position and then confirmed intraoperatively. Marking of the superior gluteal flap employs the rule of “thirds” (Fig. 31.2). The posterior superior iliac spine and the prominence of the greater trochanter of the femur are palpated and marked. A line drawn between these points and divided into thirds will
denote the expected location of the superior gluteal artery at the junction between the upper and middle third. The location of the piriformis muscle can be found by drawing a line from the posterior superior iliac spine to the coccyx. A new line drawn from the midpoint of this line to the trochanter will show the position of the piriformis muscle, helping to differentiate between the superior and inferior gluteal perforating vessels.
denote the expected location of the superior gluteal artery at the junction between the upper and middle third. The location of the piriformis muscle can be found by drawing a line from the posterior superior iliac spine to the coccyx. A new line drawn from the midpoint of this line to the trochanter will show the position of the piriformis muscle, helping to differentiate between the superior and inferior gluteal perforating vessels.
 Figure 31.3 Clinical case with the markings utilizing the rule of thirds. This patient is 4 months after the contralateral side, and the scar location and quality can be seen. |
When the patient is positioned in the operating room, a handheld Doppler probe can be used to search for and confirm perforators in these areas. The skin design can then be marked on the buttock, including within it the identified perforators (Fig. 31.3). The skin design can be up to 30 cm in length and 10 to 12 cm in width and still allow closure of the buttock without tension. The axis of the flap is made slightly oblique or horizontal in position to best hide the ultimate scar and to effectively lift the buttock area, improving its aesthetic.
For immediate breast reconstruction, a lateral position can be employed and a two-team approach can be used. The oncologic team can perform the mastectomy while the reconstructive team harvests the ipsilateral gluteal flap. In delayed cases, a supine–prone strategy is employed in which the recipient site is first prepared supine. Once adequate vessels are found for reconstruction, the wound is temporarily closed and the patient is changed to a prone position for harvest of the flap. Once harvested, the flap is placed on the back table and the donor site is quickly closed. The patient is returned to the supine position for the microscopic anastomosis and insetting of the flap.
Since these cases are long and in unnatural positions, exquisite care must be taken to pad the patient appropriately to prevent pressure-related problems.
Recipient Site
Prior to the final flap dissection, the recipient site is prepared. In the case of immediate reconstruction, the thoracodorsal system is evaluated first as it is normally exposed already from any axillary lymph node dissection (Fig. 31.4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree