Breast Surgery after Radioactive Seed Localization
Richard J. Gray
Barbara A. Pockaj
The goal of breast conserving therapy is to remove the lesion with the minimum tissue volume necessary to ensure negative margins, a low recurrence risk, and a good cosmetic result. More than two-thirds of breast cancers are nonpalpable, as are an even greater proportion of undiagnosed breast lesions. These nonpalpable lesions require radiologic localization for surgical treatment or biopsy. The standard procedure for excision of nonpalpable breast lesions is wire localization (WL). There are several disadvantages with the standard WL technique that include the following:
Wire skin entry site may be far away from the tumor resulting in more difficulty planning the incision site and excess normal tissue being excised.
Margins of excision have been reported to be positive, requiring a second operation for reexcision up to 50% of the time (1,2).
Wire can be displaced during postlocalization mammogram and transfer to the operating room.
Wire must be placed on the same day of surgery, resulting in logistical challenges for radiology and operative suites that may result in more inpatient stays due to operations occurring late in the day.
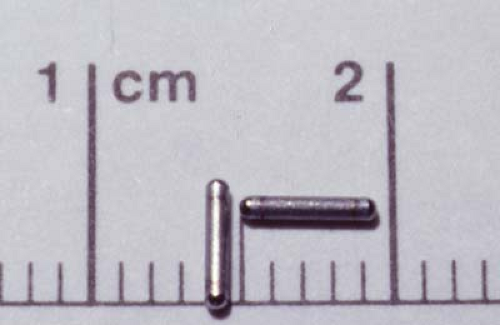
Radioactive seed localization (RSL) overcomes many of these disadvantages. The technique utilizes a 4.5 mm by 0.8 mm titanium seed labeled with 125I (usual dose 0.100–0.150 mCi) (Fig. 9.1). The same radioactive seed is used for prostate brachytherapy. The radioactive seed is placed percutaneously, using radiologic guidance in a manner similar to that used for wire placement. Intraoperative localization is performed using a gamma counter set to detect 125I. Several studies have demonstrated the safety, feasibility, and effectiveness of RSL, including a demonstration of virtually no radiation exposure to staff. Patients also benefit by as much as a 52% reduction in the rate of positive margins (3).
The first step in preoperative planning for RSL is ensuring an appropriate program is in place. RSL requires that the institution have a medical license issued by the Nuclear Regulatory Commission or an agreement state, as is the case for any institution using radioactive materials for any purpose. In addition, an authorized nuclear medicine physician or radiation oncologist must agree to oversee the safe use of radioactive seeds and develop systems for ensuring each seed is safely handled and returned to nuclear storage for decay after use. One must also clarify billing issues: the same Current Procedural Terminology (CPT) code is used for the operative procedure, but the CPT code for the radiologic placement of the radioactive seed must be clarified with payers. Current CPT codes to be considered include 19499, 19290, A4641, 77032, and 76942.
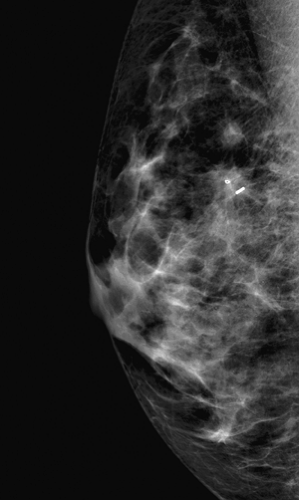
Radiologic placement of radioactive seeds is done with largely the same techniques as for WL. Seeds may be inserted up to 5 days before the operation, although 1 day prior to the operation is most common to allow concurrent injection of radiocolloid for sentinel lymph node (SLN) mapping. After assembling the necessary items (Fig. 9.2), the target(s) is confirmed with ultrasound or mammography and the approach determined. Unlike WL, in RSL, the radiologist may use the best available approach for accurate seed placement without concern for the skin entry site complicating the operative approach for the surgeon. Using reverse-spring tweezers, a sterile seed is loaded into an 18-G spinal needle, the tip of which has been occluded with bone wax. After providing adequate local anesthesia, the needle is advanced to the target under imaging
guidance and the seed deployed by advancing a stylet through the needle. A postlocalization mammogram confirms positioning of the seed (Fig. 9.3).
guidance and the seed deployed by advancing a stylet through the needle. A postlocalization mammogram confirms positioning of the seed (Fig. 9.3).
 Figure 9.2 Equipment for radiologic placement of radioactive seed. (Photo courtesy of Michelle McDonough, MD.) |
There are several potential RSL pitfalls of which the radiologist must be aware of.
The stylet must be placed part way into the spinal needle or additional bone wax placed into the needle hub during the localization to ensure the seed does not slide back out through the hub as the angle of the needle is manipulated.
The diameters of 18-G spinal needles and of the radioactive seeds can slightly vary, so one must ensure the seed passes through the needle adequately before beginning localization.
One must ensure the stylet passes through the bone wax for the seed to deploy, so note how far into the spinal needle the stylet fits before beginning each localization procedure.
Multiple radioactive seeds can be placed to localize multiple lesions or bracket a large lesion. Orienting these seeds to separate on a radial plane rather than in the anterior-to-posterior dimension allows the surgeon to more easily detect the seeds as separate gamma sources at the skin level. Having the ability to separately detect these signals allows surgeon to more precisely plan incision and dissection.
No patient or staff shielding is necessary, nor are patient warnings or precautions necessary when the patient leaves the radiology suite. A single 125I seed provides little radiation exposure. The radiation dose at 15 cm from each low-dose seed is less than one-tenth the radiation exposure from a plane flight.
Steps of the Procedure
Excision of a nonpalpable breast lesion by using RSL requires only a gamma probe such as those used for SLN biopsy. The 125I seed can be detected as a separate source from the 99Tc colloid used for SLN mapping. The steps for the RSL surgical excision are as follows:
Set the gamma counter to detect 125I. The setting for a SLN biopsy procedure is 99Tc. It is critical that the gamma counter is changed for the RSL as the surgeon can be misled to think the 99
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree