Substantial bone loss and bone defects are among the most challenging problems faced by surgeons performing revision knee arthroplasty. Tibial bone loss in failed total knee arthroplasty (TKA) is a complex and difficult problem.
 Awareness and proper management of bone loss through cement fill, metal augments, or bone grafting are crucial for achieving stability and longevity of the newly implanted revision components.
Awareness and proper management of bone loss through cement fill, metal augments, or bone grafting are crucial for achieving stability and longevity of the newly implanted revision components.
ANATOMY
 Tibial bone loss during revision TKA is common. The most common areas of deficiency involve the posterolateral and medial tibial plateau.
Tibial bone loss during revision TKA is common. The most common areas of deficiency involve the posterolateral and medial tibial plateau.
 Bone loss is typically inconsequential and contained; even after component removal, bone loss can be restricted to discrete cancellous defects.
Bone loss is typically inconsequential and contained; even after component removal, bone loss can be restricted to discrete cancellous defects.
 Smaller, contained defects can often be addressed with morcellized autografts from bone cuts (or allograft if unavailable) or with bone cement alone. Larger, uncontained defects may require the use of metallic wedges or structural allografts.
Smaller, contained defects can often be addressed with morcellized autografts from bone cuts (or allograft if unavailable) or with bone cement alone. Larger, uncontained defects may require the use of metallic wedges or structural allografts.
PATHOGENESIS
 The etiology of bone loss after TKA is usually multifactorial. Bone stock deficiency may result from any of the following causes:
The etiology of bone loss after TKA is usually multifactorial. Bone stock deficiency may result from any of the following causes:
Aseptic loosening. Secondary to component malposition or ligament imbalance, aseptic loosening can cause collapse of the tibia plateau on the compression side as well as lift-off on the tension side.
Periprosthetic osteolysis. Wear debris following TKA is frequently due to high-contact stresses secondary to poor implant design or poor component alignment or ligament balance12 and can result in lysis of the bone.
Infection
Removal of well-fixed implants. Even using proper technique, implant removal can result in some degree of bone loss, particularly from the implant-adherent region.7
NATURAL HISTORY
 Regardless of the mechanism of bone loss, it is likely that continuing progression, leading to eventual failure of the TKA, will occur once significant bony destruction is visible on plain radiographs.
Regardless of the mechanism of bone loss, it is likely that continuing progression, leading to eventual failure of the TKA, will occur once significant bony destruction is visible on plain radiographs.
 In this spiral toward implant failure, patients may be asymptomatic initially. However, pain, swelling, and instability, including hyperextension due to loss of tibial height, can be expected and are likely sequelae of a failing TKA with significant tibial bone loss.
In this spiral toward implant failure, patients may be asymptomatic initially. However, pain, swelling, and instability, including hyperextension due to loss of tibial height, can be expected and are likely sequelae of a failing TKA with significant tibial bone loss.
PATIENT HISTORY AND PHYSICAL FINDINGS
 Preoperative evaluation begins with a detailed history and clinical examination.
Preoperative evaluation begins with a detailed history and clinical examination.
 It is paramount that the cause of failure is determined in the preoperative assessment to reduce the risk of repeating mistakes that may have led to failure of the initial TKA.
It is paramount that the cause of failure is determined in the preoperative assessment to reduce the risk of repeating mistakes that may have led to failure of the initial TKA.
 Other causes of pain, such as spinal or hip pathology, should be ruled out.
Other causes of pain, such as spinal or hip pathology, should be ruled out.
 Contraindications for surgery, such as infection, poor general condition, Charcot arthropathy, or neuromuscular disorders, must be ruled out.
Contraindications for surgery, such as infection, poor general condition, Charcot arthropathy, or neuromuscular disorders, must be ruled out.
 Reports of previous surgeries must be obtained to gather information on prior soft tissue releases performed as well as the type and size of the current prosthetic components.
Reports of previous surgeries must be obtained to gather information on prior soft tissue releases performed as well as the type and size of the current prosthetic components.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 A thorough clinical and radiographic evaluation is a prerequisite for revision TKA. The extent and location of bone loss, the quality of the remaining bone, the degree of cortical continuity, and the absence of infection must be determined.
A thorough clinical and radiographic evaluation is a prerequisite for revision TKA. The extent and location of bone loss, the quality of the remaining bone, the degree of cortical continuity, and the absence of infection must be determined.
 Full-length standing anteroposterior radiographs should be taken to assess coronal limb alignment and the presence of diaphyseal deformities or hardware.
Full-length standing anteroposterior radiographs should be taken to assess coronal limb alignment and the presence of diaphyseal deformities or hardware.
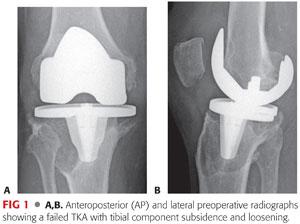
 Weight-bearing anteroposterior, lateral, and Merchant patellar views allow the femoral and tibial implant size to be evaluated and current bone stock, implant position and fixation, and patellar height and coronal position to be assessed (FIG 1).
Weight-bearing anteroposterior, lateral, and Merchant patellar views allow the femoral and tibial implant size to be evaluated and current bone stock, implant position and fixation, and patellar height and coronal position to be assessed (FIG 1).
 The true magnitude of bone loss is often underestimated on radiographs. Computed tomography (CT) scans may estimate the degree of bone loss more accurately, particularly when there is massive bone loss or abnormal anatomy, as well as help in identifying malrotation of the femoral or tibial component.14
The true magnitude of bone loss is often underestimated on radiographs. Computed tomography (CT) scans may estimate the degree of bone loss more accurately, particularly when there is massive bone loss or abnormal anatomy, as well as help in identifying malrotation of the femoral or tibial component.14
 All patients should have the appropriate infection laboratory studies (ie, complete blood count, C-reactive protein, erythrocyte sedimentation rate). Knee aspiration should be considered in order to obtain culture specimens as well as a cell count with differential. Synovial fluid aspirates with leukocyte counts greater than or equal to 2500 per mm3 in conjunction with a neutrophil percentage of 60% are indicative of infection.11
All patients should have the appropriate infection laboratory studies (ie, complete blood count, C-reactive protein, erythrocyte sedimentation rate). Knee aspiration should be considered in order to obtain culture specimens as well as a cell count with differential. Synovial fluid aspirates with leukocyte counts greater than or equal to 2500 per mm3 in conjunction with a neutrophil percentage of 60% are indicative of infection.11
DIFFERENTIAL DIAGNOSIS
 Extremity pain in a patient with a TKA can have several possible nonsurgical diagnoses, including the following:
Extremity pain in a patient with a TKA can have several possible nonsurgical diagnoses, including the following:
Referred pain from the hip, thigh, or calf
Complex regional pain syndrome
Pes anserine bursitis
Patellar or hamstring tendinitis
Crystal deposition disease (ie, gout or pseudogout)
Neurovascular problems: neuropathy, radiculopathy, spinal stenosis
Tumor (should eventually be considered)
Vascular claudication
Thrombophlebitis or deep vein thrombosis
Fibromyalgia
NONOPERATIVE MANAGEMENT
 Nonoperative management of a painful TKA with tibial bone loss is often not indicated. However, if revision is not deemed safe for medical, psychosocial, or other reasons, management is similar to that for a patient with end-stage knee arthritis.
Nonoperative management of a painful TKA with tibial bone loss is often not indicated. However, if revision is not deemed safe for medical, psychosocial, or other reasons, management is similar to that for a patient with end-stage knee arthritis.
 Treatment options are symptom-based and can include activity modification, walking aids, nonsteroidal pain medications, and bracing.
Treatment options are symptom-based and can include activity modification, walking aids, nonsteroidal pain medications, and bracing.
SURGICAL MANAGEMENT
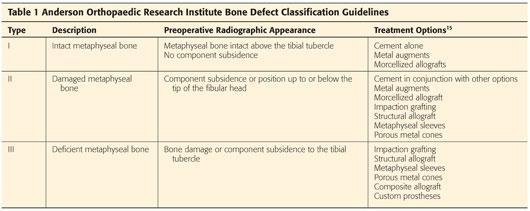
 Various joint reconstruction techniques have been described for dealing with bone loss. The choice of reconstruction depends largely on the type of bone loss (ie, contained or uncontained) and the location and size of the defect (Table 1).
Various joint reconstruction techniques have been described for dealing with bone loss. The choice of reconstruction depends largely on the type of bone loss (ie, contained or uncontained) and the location and size of the defect (Table 1).
Cement and screw reconstruction
Morcellized autograft or allograft with impaction grafting16
Prosthetic augments
Modular hinged prosthesis
Metaphyseal sleeves or cones
Structural allograft
 A contained defect is surrounded by intact bone and has an intact peripheral cortical rim that allows treatment with morcellized bone graft or cement and screws.2,12
A contained defect is surrounded by intact bone and has an intact peripheral cortical rim that allows treatment with morcellized bone graft or cement and screws.2,12
 An uncontained defect has no peripheral cortical rim and typically requires modular block augments, bulk allograft, or metal metaphyseal sleeves or cones for reconstruction.2
An uncontained defect has no peripheral cortical rim and typically requires modular block augments, bulk allograft, or metal metaphyseal sleeves or cones for reconstruction.2
Preoperative Planning
 Bone loss around a knee implant should be assessed systematically and include both femoral condyles, both tibial plateaus, and the patellofemoral joint.
Bone loss around a knee implant should be assessed systematically and include both femoral condyles, both tibial plateaus, and the patellofemoral joint.
 Location of the joint line is marked. Reference points include the fibular head and the epicondyles of the femur. The joint line typically sits 20 to 25 mm distal of the lateral epicondyle.4
Location of the joint line is marked. Reference points include the fibular head and the epicondyles of the femur. The joint line typically sits 20 to 25 mm distal of the lateral epicondyle.4
 The magnitude of bone loss has significant implications for decisions regarding the use of bone graft or prosthesis augmentation, choice of prosthesis sizing, selection of articular constraint, and need for supplemental stem fixation.5
The magnitude of bone loss has significant implications for decisions regarding the use of bone graft or prosthesis augmentation, choice of prosthesis sizing, selection of articular constraint, and need for supplemental stem fixation.5
Positioning
 Revision TKA is usually performed with the patient in the supine position.
Revision TKA is usually performed with the patient in the supine position.
Approach
 Sufficient surgical exposure is of critical importance in revision TKA. With revision surgery, the soft tissue planes are often blurred by extensive scar tissue. The incision should therefore be lengthened as necessary to allow adequate exposure and visualization and the surgeon should work from normal tissue to recreate the tissue planes.
Sufficient surgical exposure is of critical importance in revision TKA. With revision surgery, the soft tissue planes are often blurred by extensive scar tissue. The incision should therefore be lengthened as necessary to allow adequate exposure and visualization and the surgeon should work from normal tissue to recreate the tissue planes.
 A standard medial parapatellar arthrotomy of the knee is routinely performed; however, for some cases, the subvastus approach could still be used.
A standard medial parapatellar arthrotomy of the knee is routinely performed; however, for some cases, the subvastus approach could still be used.
 Next, a thorough intra-articular synovectomy is performed to expose the implants and recreate the lateral gutters.
Next, a thorough intra-articular synovectomy is performed to expose the implants and recreate the lateral gutters.
 Additional exposure is often required if a metal wire mesh is needed for unconstrained defects. The proximal portion of the tibia must be well exposed to ensure fixation of the wire mesh onto the bone. External rotation of the tibia and elevation of the medial sleeve often help with exposure of the cortical margins.
Additional exposure is often required if a metal wire mesh is needed for unconstrained defects. The proximal portion of the tibia must be well exposed to ensure fixation of the wire mesh onto the bone. External rotation of the tibia and elevation of the medial sleeve often help with exposure of the cortical margins.
 The surgeon should assess the stability of the collateral ligaments prior to removal of the implants.
The surgeon should assess the stability of the collateral ligaments prior to removal of the implants.
 Following medial release, the knee is dislocated and the polyethylene insert removed. The patella is sublimated rather than everted to minimize tension on the extensor mechanism. A quadriceps snip can be performed if needed, which reduces the risk of iatrogenic disruption to the extensor mechanism without exacerbating postoperative restrictions for the patient.3
Following medial release, the knee is dislocated and the polyethylene insert removed. The patella is sublimated rather than everted to minimize tension on the extensor mechanism. A quadriceps snip can be performed if needed, which reduces the risk of iatrogenic disruption to the extensor mechanism without exacerbating postoperative restrictions for the patient.3
 Once the components are adequately exposed, they are evaluated and implant removal is initiated. The implant–bone or cement–bone interface should be disrupted with a combination of flexible osteotomes and thin saw blades on an oscillating saw.
Once the components are adequately exposed, they are evaluated and implant removal is initiated. The implant–bone or cement–bone interface should be disrupted with a combination of flexible osteotomes and thin saw blades on an oscillating saw.
 Cavitary defects need to be contoured. In case of multiloculated defects, they need to be cleaned from the cavitary defects. In addition, sclerotic areas need to be decorticated. This is best accomplished with a high-speed burr.
Cavitary defects need to be contoured. In case of multiloculated defects, they need to be cleaned from the cavitary defects. In addition, sclerotic areas need to be decorticated. This is best accomplished with a high-speed burr.
 When removing the components, the degree of iatrogenic bone loss can be minimized with a careful and methodologic surgical technique.
When removing the components, the degree of iatrogenic bone loss can be minimized with a careful and methodologic surgical technique.
TECHNIQUES
 Morcellized Allograft
Morcellized Allograft
Morcellized grafting is indicated in Anderson Orthopaedic Research Institute (AORI) type 1 and type 2 defects, in which the metaphyseal rim is intact.15
The primary advantage is a restoration of bone stock without the need for donor bone. This is of particular importance in young patients in whom further revision procedures can be expected.
As a part of the débridement process, a high-speed burr/reamer or a curette is typically used to remove sclerotic bone down to the underlying bleeding bed.
After thorough débridement, allograft bone is placed within the contained defect before placement of the final components.
 Impaction Grafting
Impaction Grafting
Indications for impaction grafting are AORI type 2 and type 3 defects.9
Impaction grafting is an attempt to reconstitute bone stock and avoid problems associated with excessively large or long uncemented stems.
It is particularly indicated in younger patients.
Unlike augments, impaction grafting can use irregular-shaped areas of bone loss. It is typically employed in contained defects, although the addition of a wire mesh to enclose any metaphyseal defects extends its application to uncontained defects.
The impaction of the different layers of graft is time-consuming.
Impaction grafting is associated with an increased risk of iatrogenic intraoperative fracture or perforation of metaphyseal or diaphyseal bone.
Contained Defects
A trial stem is inserted into the tibial canal to determine the proper size and stem length. The stem could be larger than the anticipated stem. Care should be taken to align the stem properly.
Contained defects require impaction of bone directly into the defect (TECH FIG 1).
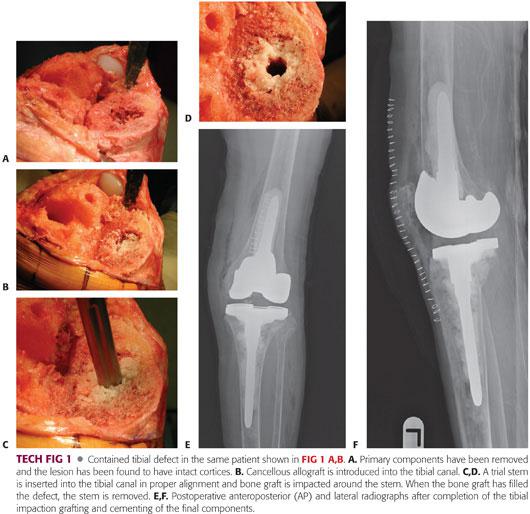
Morcellized bone graft is progressively impacted in layers around the stem until the metaphysis has been filled.
The surgeon should be prepared to fix or bypass, as appropriate, iatrogenic fractures or perforations of the metaphyseal or diaphyseal bone.
Once the impaction process is complete, the trial stem is carefully removed. The final components are cemented into place and excess cement removed.
Uncontained Defects
Uncontained defects call for a wire mesh to reproduce the cortical anatomy (TECH FIG 2).
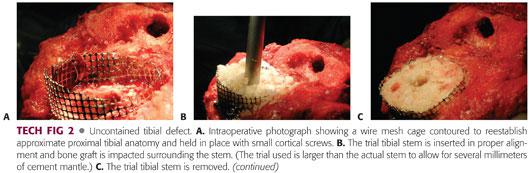
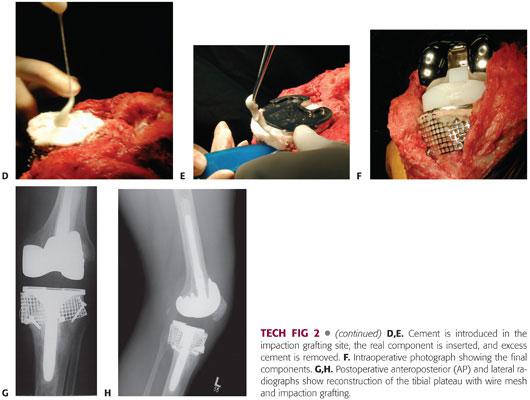
The wire mesh is molded to estimate the normal contours of the proximal tibia and is held in place with small cortical screws.
A central intramedullary guide rod with cement restrictor is inserted to allow a gap of 2 cm from the anticipated end of the final tibial stem component.
A trial tibial stem is inserted into the tibial canal in neutral alignment. The final chosen stem should be smaller to allow for a 2-mm circumferential cement mantle.
Thawed fresh frozen morcellized cancellous allograft is introduced into the tibial canal and impacted tightly around the stem using either cannulated or standard tamps and a mallet.
The trial stem is removed, leaving a restored mantle of cancellous bone.
The stemmed tibial prosthesis is cemented in standard fashion.
 Structural Femoral Head Allograft
Structural Femoral Head Allograft
Indications for structural, or bulk, allograft are AORI type 2 and type 3 defects.5
Structural allograft is typically used for defects larger than the metal augments available for use in revision TKA.
Structural allograft is an attempt to reconstitute bone stock. It is therefore particularly indicated in younger patients.
Preoperatively, estimate the size of the defect and order appropriate-sized femoral head allografts. The size of the graft should match as closely as possible with the size of the defect.
Following débridement, the metaphyseal bone is hemispherically reamed. Reaming through the thin metaphyseal cortical bone, with the creation of an uncontained defect, must be avoided.
Once the recipient bed is prepared, the femoral head allograft is prepared on the back table using a female reamer (TECH FIG 3A). The graft should be irrigated using a pulsatile irrigator and, depending on the size of the graft, 2 or more liters of saline.
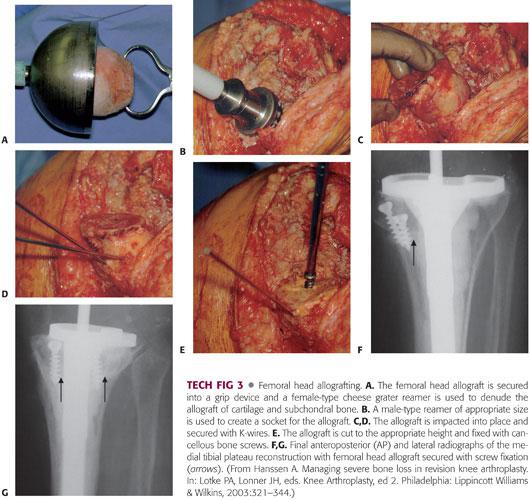
The allograft is usually reamed to one size larger than the male reamer used to prepare the metaphyseal bone (TECH FIG 3B). The host bone is reamed to expose healthy, bleeding cancellous bone, with removal of all fibrous tissue and cement.
Sclerotic bone may cause the reamer to wander. In these cases, a high-speed burr may be used to remove sclerotic bone.
The allograft is prepared to maximize the contact surface area across the allograft–host junction, optimize the mechanical interlock between the graft and host, allow rigid implant fixation, and restore anatomy.
The allograft is placed into the defect and provisionally secured with Kirschner (K) wires or Steinmann pins. These should be placed so that they do not interfere with the stemmed prosthesis insertion (TECH FIG 3C,D).
Revision cutting guides are used to trim the allograft for component implantation. Tibial component preparation should follow standard revision principles.
Finally, the K-wires are removed. They can be replaced with partially threaded 4.0- or 4.5-mm cancellous screws, and the tibial component is press-fitted or cemented in the standard fashion (TECH FIG 3E–G).
 Massive Tibial Allograft
Massive Tibial Allograft
The indication for massive tibial allograft is AORI type 3 defects with or without extensor mechanism failures (TECH FIG 4).8
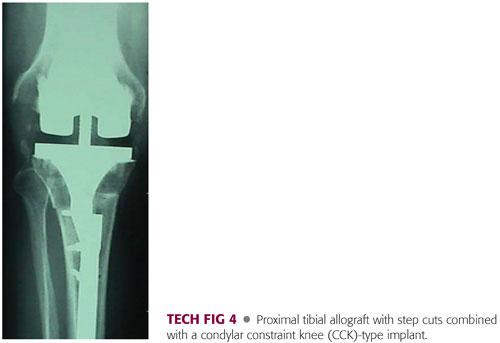
Implantation of an allograft prosthetic component (APC) is a challenging salvage procedure in the presence of uncontained circumferential defects that involve a large part of the proximal tibia and cannot be treated with cement, augments, or structural allograft alone.
It can be considered as an alternative to a tumor prosthesis.
The APC of the tibia is fashioned to the correct size based on careful measurements of the host tibia after thorough débridement.
After careful measurement (and following débridement) of the host tibia, the graft should be slightly oversized in length. If necessary, it should be trimmed down to size.
The allograft–host junction should be bypassed by a press-fit stem by approximately 5 cm.
To optimize rotational stability of the implant, the host bone and graft bone should be shaped with oblique or step cuts.
Positioning of the graft should be carried out with the trial implants already in place to verify that anatomic positioning and good patella height and tracking has been obtained.
The final position should be marked with a cautery or marking pen to assist appropriate overall orientation in final implantation of the APC.
If the extensor mechanism is deficient secondary to bone loss, or in the presence of tendon rupture or erosion of the extensor mechanism, the procedure can be performed in conjunction with reconstruction of the extensor mechanism.
PEARLS AND PITFALLS | |
Preoperative planning |
|
| |
| |
Débridement |
|
Mechanical contouring |
|
| |
Impaction grafting |
|
| |
Morcellized allograft |
|
Impaction grafting |
|
| |
| |
Structural allograft |
|
| |
| |
Massive tibial allograft |
|
| |
POSTOPERATIVE CARE
 Postoperative management should be tailored to the individual patient and depends on the degree of bone loss, the primary stability of the implant and graft, soft tissue quality, and extensor mechanism compromise.
Postoperative management should be tailored to the individual patient and depends on the degree of bone loss, the primary stability of the implant and graft, soft tissue quality, and extensor mechanism compromise.
 The priority should be wound healing and incorporation of the graft. With large allograft techniques, weight bearing is restricted until graft incorporation has occurred. Partial weight bearing is typically recommended for a minimum of 6 to 8 weeks and continued until radiographic signs of union at the graft–host interface are present.1
The priority should be wound healing and incorporation of the graft. With large allograft techniques, weight bearing is restricted until graft incorporation has occurred. Partial weight bearing is typically recommended for a minimum of 6 to 8 weeks and continued until radiographic signs of union at the graft–host interface are present.1
OUTCOMES
 Lotke et al10 reported prospectively on 48 consecutive patients treated with impaction allograft for substantial bone loss in revision TKA. They found no mechanical failures and all radiographs showed incorporation and remodeling of the bone graft. Six complications (14%) were reported, including two infections and two periprosthetic fractures.
Lotke et al10 reported prospectively on 48 consecutive patients treated with impaction allograft for substantial bone loss in revision TKA. They found no mechanical failures and all radiographs showed incorporation and remodeling of the bone graft. Six complications (14%) were reported, including two infections and two periprosthetic fractures.
 Engh and Ammeen6 reported outcomes at a mean of 7.9 years postoperatively in 49 knees with severe tibial bone defects requiring revision arthroplasty. Three patients could not be assessed. Four revision procedures had failed and required reoperation. No instance of graft collapse or aseptic loosening associated with the structural graft were found.
Engh and Ammeen6 reported outcomes at a mean of 7.9 years postoperatively in 49 knees with severe tibial bone defects requiring revision arthroplasty. Three patients could not be assessed. Four revision procedures had failed and required reoperation. No instance of graft collapse or aseptic loosening associated with the structural graft were found.
 Naim and Toms13 published prospective findings on 11 patients with large tibial defects treated with knee impaction bone grafting and a short cemented stem. Over a minimum follow-up of 2 years, there were no mechanical failures, all radiographs showed incorporation and remodeling of the graft, and none of the patients required secondary procedures or further revisions. One complication—superficial dysesthesia around the operative scar—was recorded.
Naim and Toms13 published prospective findings on 11 patients with large tibial defects treated with knee impaction bone grafting and a short cemented stem. Over a minimum follow-up of 2 years, there were no mechanical failures, all radiographs showed incorporation and remodeling of the graft, and none of the patients required secondary procedures or further revisions. One complication—superficial dysesthesia around the operative scar—was recorded.
COMPLICATIONS
 Bone graft resorption
Bone graft resorption
 Graft collapse
Graft collapse
 Infection
Infection
 Instability
Instability
 Joint line elevation
Joint line elevation
 Stiffness
Stiffness
 Periprosthetic fracture
Periprosthetic fracture
 End-of-stem pain1
End-of-stem pain1
 Allograft nonunion2
Allograft nonunion2
REFERENCES
1. Barrack RL, Rorabeck C, Burt M, et al. Pain at the end of the stem after revision total knee arthroplasty. Clin Orthop Relat Res 1999;(367):216–225.
2. Daines BK, Dennis DA. Management of bone defects in revision total knee arthroplasty. Instr Course Lect 2013;62:341–348.
3. Della Valle CJ, Berger RA, Rosenberg AG. Surgical exposures in revision total knee arthroplasty. Clin Orthop Relat Res 2006;446:59–68.
4. Dennis DA. A stepwise approach to revision total knee arthroplasty. J Arthroplasty 2007;22:32–38.
5. Elia EA, Lotke PA. Results of revision total knee arthroplasty associated with significant bone loss. Clin Orthop Relat Res 1991;(271):114–121.
6. Engh GA, Ammeen DJ. Use of structural allograft in revision total knee arthroplasty in knees with severe tibial bone loss. J Bone Joint Surg Am 2007;89:2640–2647.
7. Engh GA, Parks NL. The management of bone defects in revision total knee arthroplasty. Instr Course Lect 1997;46:227–236.
8. Kuchinad RA, Garbedian S, Rogers BA, et al. The use of structural allograft in primary and revision knee arthroplasty with bone loss. Adv Orthop 2011;2011:578952.
9. Lonner JH, Lotke PA, Kim J, et al. Impaction grafting and wire mesh for uncontained defects in revision knee arthroplasty. Clin Orthop Relat Res 2002;(404):145–151.
10. Lotke PA, Carolan GF, Puri N. Impaction grafting for bone defects in revision total knee arthroplasty. Clin Orthop Relat Res 2006;446:99–103.
11. Mason JB, Fehring TK, Odum SM, et al. The value of white blood cell counts before revision total knee arthroplasty. J Arthroplasty 2003;18:1038–1043.
12. Morrison JC, Reilly DT. Allograft in revision total knee arthroplasty. In: Bono JV, Scott RD, eds. Revision Total Knee Arthroplasty. New York: Springer Science+Business Media, Inc, 2005:81–96.
13. Naim S, Toms AD. Impaction bone grafting for tibial defects in knee replacement surgery. Results at two years. Acta Orthop Belg 2013;79:205–210.
14. Nicoll D, Rowley DI. Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 2010;92:1238–1244.
15. Stock GH, Austin MS, Meneghini RM. Management of bone loss in revision total knee arthroplasty. In: Parvizi J, ed. Principles and Techniques in Revision Total Knee Arthroplasty. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2012:49–60.
16. Stulberg SD. Bone loss in revision total knee arthroplasty: graft options and adjuncts. J Arthroplasty 2003;18:48–50.
< div class='tao-gold-member'>




















