Severe deformity is a congenital (acquired or iatrogenic) abnormality in the size and shape of the native acetabulum or proximal femur, and special techniques or implants must be employed by the surgeon to perform a primary total hip arthroplasty (THA).
ANATOMY
 Severe deformities around the hip typically result from pediatric hip disease, skeletal dysplasia, infection, metabolic bone disease, or trauma; or are the consequences of the treatment.
Severe deformities around the hip typically result from pediatric hip disease, skeletal dysplasia, infection, metabolic bone disease, or trauma; or are the consequences of the treatment.
 The American Academy of Orthopaedic Surgeons’ classification can be used to describe both acetabular-sided11 and femoral-sided12 deformity:
The American Academy of Orthopaedic Surgeons’ classification can be used to describe both acetabular-sided11 and femoral-sided12 deformity:
Acetabular deficiencies in deformity are frequently segmental (type I), cavitary (type II), or combined (type III).
Femoral abnormalities are typically malalignment (type IV) or stenosis (type V). The Paprosky classification does not include these deformities. However, occasionally, the proximal femur is completely absent.
 Although we focus on bony abnormality because of technical problems with fit and fix, deformed anatomy around the hip also alters local hip biomechanics with subsequent overloading and secondary osteoarthritis (OA) because of changes in the insertion and lever arm of muscles around the hip, particularly the abductors.
Although we focus on bony abnormality because of technical problems with fit and fix, deformed anatomy around the hip also alters local hip biomechanics with subsequent overloading and secondary osteoarthritis (OA) because of changes in the insertion and lever arm of muscles around the hip, particularly the abductors.
 Deformed anatomy at the hip affects the mechanical alignment of the entire lower limb and alters the biomechanics of the knee, ankle, and foot, and can lead to degenerative joint disease at these locations.
Deformed anatomy at the hip affects the mechanical alignment of the entire lower limb and alters the biomechanics of the knee, ankle, and foot, and can lead to degenerative joint disease at these locations.
 Abnormal anatomy creates difficulties in approach (identifying true anatomy), implant selection (because of problems with endosteal anatomy), size, and the challenges of restoring lower limb biomechanics.
Abnormal anatomy creates difficulties in approach (identifying true anatomy), implant selection (because of problems with endosteal anatomy), size, and the challenges of restoring lower limb biomechanics.
 The most common cause of hip deformity in adults is developmental dysplasia of the hip (DDH), where a small dysplastic acetabulum is coupled with an anteverted femur with a narrow canal which may have been treated with previous proximal femoral osteotomy, further complicating the deformity. DDH itself can be caused by congenital dysplasia (most commonly dislocation), the consequences of infantile infection, neuromuscular disease, or inflammatory joint disease.
The most common cause of hip deformity in adults is developmental dysplasia of the hip (DDH), where a small dysplastic acetabulum is coupled with an anteverted femur with a narrow canal which may have been treated with previous proximal femoral osteotomy, further complicating the deformity. DDH itself can be caused by congenital dysplasia (most commonly dislocation), the consequences of infantile infection, neuromuscular disease, or inflammatory joint disease.
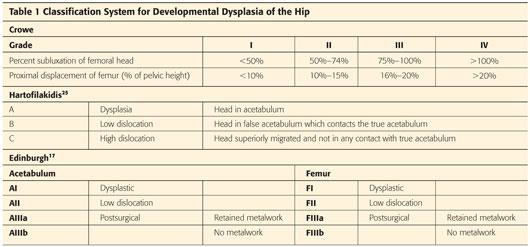
 There are several classifications of deformity severity in DDH: Crowe and Hartofilakidis25 are widely used classification systems and are composite for both sides of the hip. The Edinburgh system17 uses similar criteria but divides the problems into femur and acetabulum to allow a detailed plan for each bone to be formulated (Table 1).
There are several classifications of deformity severity in DDH: Crowe and Hartofilakidis25 are widely used classification systems and are composite for both sides of the hip. The Edinburgh system17 uses similar criteria but divides the problems into femur and acetabulum to allow a detailed plan for each bone to be formulated (Table 1).
PATHOGENESIS
 Specific conditions and their treatment cause specific deformities and ultimately specific patterns of secondary OA and symptomatology.
Specific conditions and their treatment cause specific deformities and ultimately specific patterns of secondary OA and symptomatology.
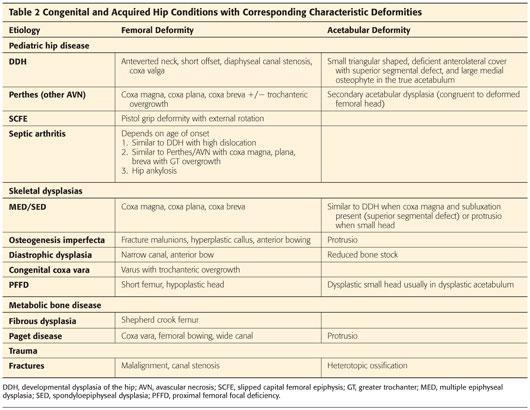
 Congenital and acquired causes of deformity around the hip joint are listed in Table 2.
Congenital and acquired causes of deformity around the hip joint are listed in Table 2.
 Osteotomies performed as realignment or conservative joint-sparing procedures to treat these conditions create new iatrogenic deformities and technical difficulties when hip reconstruction is considered:
Osteotomies performed as realignment or conservative joint-sparing procedures to treat these conditions create new iatrogenic deformities and technical difficulties when hip reconstruction is considered:
Perthes—valgising proximal femoral osteotomy +/− trochanteric advancement
DDH—varising proximal femoral osteotomy, +/− derotation, +/− extension
Slipped capital femoral epiphysis (SCFE)—valgising proximal femoral osteotomy, +/− derotation, +/− flexion
Coxa vara—valgising proximal femoral osteotomy, +/− derotation
 Retained metalwork may be overgrown, broken, or obsolete. Careful planning is required to decide whether metalwork should be removed or retained and consideration given to the consequences of its removal.
Retained metalwork may be overgrown, broken, or obsolete. Careful planning is required to decide whether metalwork should be removed or retained and consideration given to the consequences of its removal.
 Deformity of the acetabulum and proximal femur disrupts hip kinematics and generates pain via the following:
Deformity of the acetabulum and proximal femur disrupts hip kinematics and generates pain via the following:
Increased joint reaction force—secondary to abductor dysfunction and coupled with reduced joint contact area leads to high load per unit area and early failure with secondary OA.
Impingement of the following:
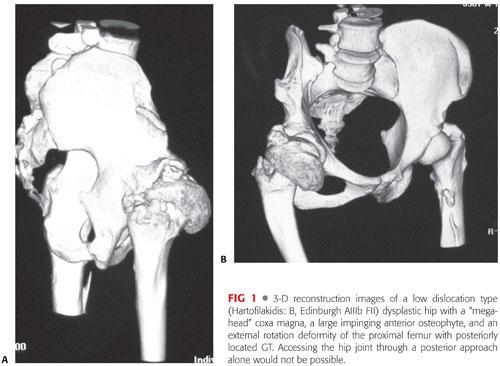
• Large, abnormal nonconcentric femoral head on the acetabulum (FIG 1)
• Overgrown greater trochanter (GT) on the ilium during hinged abduction
• Highly dislocated femoral head with the false acetabulum or ilium
Leg length discrepancy (LLD) and altered gait kinematics, causing abnormal loading of the lumbar spine and lower limbs.
Lower limb mechanical axis disruption with overloading and subsequent OA of the knee and lumbar spine
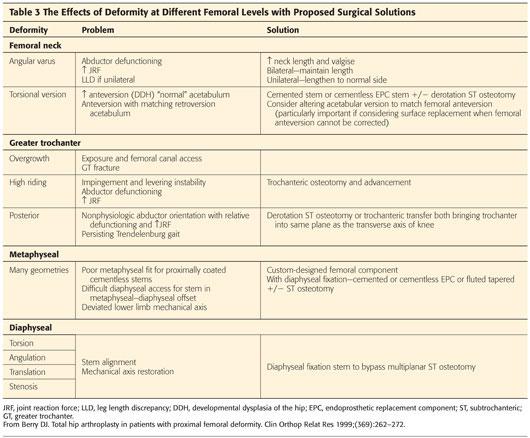
 Deformities at different levels create different problems as outlined in Table 3.
Deformities at different levels create different problems as outlined in Table 3.
NATURAL HISTORY
 Patients with deformity develop OA at an earlier age than those without deformity. The mean age at the time THA is performed in patients with deformity is 45 to 50 years old.7,20,23
Patients with deformity develop OA at an earlier age than those without deformity. The mean age at the time THA is performed in patients with deformity is 45 to 50 years old.7,20,23
PATIENT HISTORY AND PHYSICAL FINDINGS
 Patients with degenerative joint disease resulting from deformity around the hip present with exertional groin pain, knee pain (either referred or secondary long-leg arthritis), or lower back pain in addition to what may be a long-standing deformity, with or without LLD.
Patients with degenerative joint disease resulting from deformity around the hip present with exertional groin pain, knee pain (either referred or secondary long-leg arthritis), or lower back pain in addition to what may be a long-standing deformity, with or without LLD.
 Symptoms may have been present chronically with recent progression of functional limitations.
Symptoms may have been present chronically with recent progression of functional limitations.
 Patients with underlying DDH may present with iliopsoas tendon snapping over an anteverted, uncovered, sometimes large, femoral head or secondary acetabular osteophyte (see FIG 1).
Patients with underlying DDH may present with iliopsoas tendon snapping over an anteverted, uncovered, sometimes large, femoral head or secondary acetabular osteophyte (see FIG 1).
 Patients with congenital deformities may have associated conditions which must be considered; for example, fixed scoliosis (congenital, idiopathic, or acquired) or complex medical problems.
Patients with congenital deformities may have associated conditions which must be considered; for example, fixed scoliosis (congenital, idiopathic, or acquired) or complex medical problems.
 Short stature/dwarfism will affect implant sizes.
Short stature/dwarfism will affect implant sizes.
 LLD may not be obvious in bilateral disease.
LLD may not be obvious in bilateral disease.
 Following fracture with or without fixation, degenerative joint disease with pain, stiffness, and functional limitation may have developed rapidly following the acute development of deformity and mechanical malalignment.
Following fracture with or without fixation, degenerative joint disease with pain, stiffness, and functional limitation may have developed rapidly following the acute development of deformity and mechanical malalignment.
 Examination must include the following:
Examination must include the following:
Observation of gait and Trendelenburg test with Medical Research Council (MRC) Scale for Muscle Strength grading of hip abductor power
Observation of surgical scars to indicate previous hip approaches
Hip range of motion—increased internal rotation and decreased external rotation is indicative of excessive femoral anteversion prior to the stiffness of advanced OA.
Anterior impingement test
Accurate documentation of true and apparent leg lengths
Neurologic assessment and documentation of lower limb vascular status
Examination of ipsilateral knee, lumbar spine, and contralateral hip
Examination of the spine and sitting posture to determine if any spinal curvature secondary to leg length problems is correctable. This is important in older patients in whom correcting an LLD may create an unstable spinal deformity.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Sufficient imaging should be performed to gain an understanding of the three-dimensional (3-D) anatomy of the deformity and facilitate planning of its correction and the implantation of THA components.
Sufficient imaging should be performed to gain an understanding of the three-dimensional (3-D) anatomy of the deformity and facilitate planning of its correction and the implantation of THA components.
 In many cases for the experienced surgeon, this requires plain radiographs only:
In many cases for the experienced surgeon, this requires plain radiographs only:
Weight-bearing anteroposterior (AP) pelvis plus lateral of hip
Full-length femur AP and lateral to assess femoral deformity and anterior femoral bow
Judet views to assess anterior and posterior columns in acetabular deformity
Standing hip-knee-ankle x-rays to assess leg lengths and knee joint level. Some patients who have undergone surgery around the hip in childhood may experience overgrowth distally.
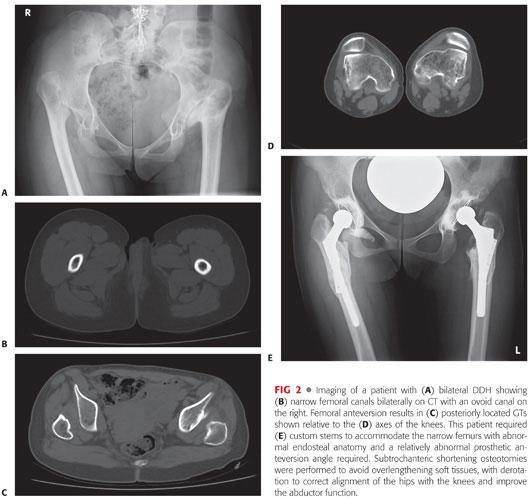
 Computed tomography (CT) scan with or without 3-D reconstruction (see FIG 1) enables visualization of multiplanar deformities in addition to assessment of acetabular bone stock, femoral canal diameter, GT position, and femoral neck version relative to the condylar axis of the knee (FIG 2). This allows detailed planning to be carried out.
Computed tomography (CT) scan with or without 3-D reconstruction (see FIG 1) enables visualization of multiplanar deformities in addition to assessment of acetabular bone stock, femoral canal diameter, GT position, and femoral neck version relative to the condylar axis of the knee (FIG 2). This allows detailed planning to be carried out.
DIFFERENTIAL DIAGNOSIS
 See Pathogenesis section.
See Pathogenesis section.
NONOPERATIVE MANAGEMENT
 As for primary hip OA, nonoperative management consists of simple analgesia, weight loss, activity modification, physical therapy, and orthotics to address LLD.
As for primary hip OA, nonoperative management consists of simple analgesia, weight loss, activity modification, physical therapy, and orthotics to address LLD.
SURGICAL MANAGEMENT
 Surgical management is indicated when conservative management has failed. The goals of surgical management are as follows:
Surgical management is indicated when conservative management has failed. The goals of surgical management are as follows:
Restoration of hip kinetics and kinematics, including hip center, acetabular and femoral version, abductor length, and GT position
Correction of lower limb mechanical alignment
Reconstruction of femoral and acetabular integrity to provide prosthesis containment
Joint stability
 Achieving these goals may require adding acetabular bone stock and correcting deformities with multiplanar osteotomies.
Achieving these goals may require adding acetabular bone stock and correcting deformities with multiplanar osteotomies.
 Subtrochanteric osteotomy should be performed if
Subtrochanteric osteotomy should be performed if
Restoring the hip center will lengthen the limb by greater than 4 cm, producing sciatic nerve traction
Significant angular/rotational/translational deformity prohibits stem access down the diaphysis or disrupts the mechanical axis of the lower limb.
Removal of awkward metalwork under direct vision
 Use implants with which you are familiar for these difficult cases, make the hip look normal, and conduct the procedure as usual. Both cemented23 and cementless stems with diaphyseal engagement31 have been used successfully in deformity cases in combination with subtrochanteric osteotomy. Our practice is to use a cemented, collarless, polished tapered stem routinely or a cementless, modular, fluted tapered stem if required. Custom-made implants may be necessary in rare cases, particularly if the endosteal anatomy is abnormal.
Use implants with which you are familiar for these difficult cases, make the hip look normal, and conduct the procedure as usual. Both cemented23 and cementless stems with diaphyseal engagement31 have been used successfully in deformity cases in combination with subtrochanteric osteotomy. Our practice is to use a cemented, collarless, polished tapered stem routinely or a cementless, modular, fluted tapered stem if required. Custom-made implants may be necessary in rare cases, particularly if the endosteal anatomy is abnormal.
 Cemented stems provide immediate stability in osteopenic bone with a narrow canal. They also provided proximal metaphyseal stability if osteotomy is required. Cemented stems do not depend on metaphyseal fit and fill to obtain stability, as proximally coated cementless stems do, and can be difficult in these cases.
Cemented stems provide immediate stability in osteopenic bone with a narrow canal. They also provided proximal metaphyseal stability if osteotomy is required. Cemented stems do not depend on metaphyseal fit and fill to obtain stability, as proximally coated cementless stems do, and can be difficult in these cases.
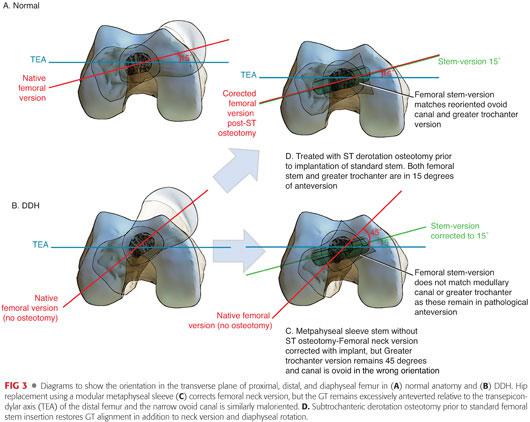
 Modular cementless femoral reconstruction systems with metaphyseal sleeves and long stems can correct femoral version independently of metaphyseal fit and fill,3,41 but they do not alter the position of the GT relative to the distal femoral condyles and thus do not restore physiologic abductor orientation or the mechanical alignment of the lower limb unless coupled with a trochanteric or subtrochanteric osteotomy (FIG 3). The diaphyseal stem provides relative stability in comparison to an osteotomy, but rotational stability depends on the diaphyseal cortical engagement of polished flutes only, with no ongrowth/ingrowth potential. Metaphyseal capture following a subtrochanteric osteotomy can be difficult with an incidence of nonunion that can be reduced by plating the osteotomy.
Modular cementless femoral reconstruction systems with metaphyseal sleeves and long stems can correct femoral version independently of metaphyseal fit and fill,3,41 but they do not alter the position of the GT relative to the distal femoral condyles and thus do not restore physiologic abductor orientation or the mechanical alignment of the lower limb unless coupled with a trochanteric or subtrochanteric osteotomy (FIG 3). The diaphyseal stem provides relative stability in comparison to an osteotomy, but rotational stability depends on the diaphyseal cortical engagement of polished flutes only, with no ongrowth/ingrowth potential. Metaphyseal capture following a subtrochanteric osteotomy can be difficult with an incidence of nonunion that can be reduced by plating the osteotomy.
 Short-stem cementless components require a long, intact neck for rotational support and good-quality metaphyseal bone stock.38 This is often absent in femoral deformity. These implants cannot correct for version or leg length and are not recommended when femoral deformity is present, although their short stem may seem attractive.
Short-stem cementless components require a long, intact neck for rotational support and good-quality metaphyseal bone stock.38 This is often absent in femoral deformity. These implants cannot correct for version or leg length and are not recommended when femoral deformity is present, although their short stem may seem attractive.
 Custom-made stems accommodate rather than correct deformity. They can be essential in very narrow femoral canals (see FIG 2) but are often also used in metaphyseal level deformity. When they are used to accommodate rather than correct metaphyseal level deformity, they do not restore mechanical alignment and are therefore exposed to high-bending moments with associated risks of aseptic loosening and cantilever bending. Failure to restore the mechanical axis of the lower limb can hasten ipsilateral knee OA development.
Custom-made stems accommodate rather than correct deformity. They can be essential in very narrow femoral canals (see FIG 2) but are often also used in metaphyseal level deformity. When they are used to accommodate rather than correct metaphyseal level deformity, they do not restore mechanical alignment and are therefore exposed to high-bending moments with associated risks of aseptic loosening and cantilever bending. Failure to restore the mechanical axis of the lower limb can hasten ipsilateral knee OA development.
 Resurfacing does not correct deformity, particularly the often extreme femoral anteversion in DDH. In less severe cases, the acetabular version can be altered to accommodate excessive version of the femoral neck, but this must be planned if the acetabulum is inserted before the femoral head.
Resurfacing does not correct deformity, particularly the often extreme femoral anteversion in DDH. In less severe cases, the acetabular version can be altered to accommodate excessive version of the femoral neck, but this must be planned if the acetabulum is inserted before the femoral head.
 Scarring from previous surgery can compromise ideal skin incision location and make exposure difficult with increased need for trochanteric osteotomy to obtain access to the diaphysis and difficulty reaming the femoral canal in up to 35% of cases.6,16
Scarring from previous surgery can compromise ideal skin incision location and make exposure difficult with increased need for trochanteric osteotomy to obtain access to the diaphysis and difficulty reaming the femoral canal in up to 35% of cases.6,16
 Removal of retained metalwork adds to surgical time. Fresh screw holes act as stress risers and allow cement extrusion. They also act as stress risers for uncemented prosthesis, which rely on high initial hoop stresses. Although consideration should be given on removing metalwork as a separate earlier procedure, the implants are often overgrown with bone, and any defect created by removal rarely heals (FIG 4). Plate removal in particular can leave a gutter in the cortex, which is difficult to manage. Leaving the plate but removing the screws either in the usual manner or cutting endosteally under direct vision at the time of THA is recommended. Overdrilling leaves large defects in what is usually a small femur.
Removal of retained metalwork adds to surgical time. Fresh screw holes act as stress risers and allow cement extrusion. They also act as stress risers for uncemented prosthesis, which rely on high initial hoop stresses. Although consideration should be given on removing metalwork as a separate earlier procedure, the implants are often overgrown with bone, and any defect created by removal rarely heals (FIG 4). Plate removal in particular can leave a gutter in the cortex, which is difficult to manage. Leaving the plate but removing the screws either in the usual manner or cutting endosteally under direct vision at the time of THA is recommended. Overdrilling leaves large defects in what is usually a small femur.

Approach Planning
 Previous surgery may determine skin incision.
Previous surgery may determine skin incision.
 Trochanteric osteotomy (standard, extended, or subtrochanteric) may be required for access to the femur.
Trochanteric osteotomy (standard, extended, or subtrochanteric) may be required for access to the femur.
 Excessive anteversion and severe arthritis leading to stiffness or a megahead can lead to difficulties on dislocation of the hip (see FIG 1). A combined anterior and posterior approach should be used to release tight structures and identify bone anatomy before cutting bone.
Excessive anteversion and severe arthritis leading to stiffness or a megahead can lead to difficulties on dislocation of the hip (see FIG 1). A combined anterior and posterior approach should be used to release tight structures and identify bone anatomy before cutting bone.
Bone Quantity and Quality
 Acetabular defects may require bone stock restoration—is adequate autograft available or will trabecular metal or allograft be required?
Acetabular defects may require bone stock restoration—is adequate autograft available or will trabecular metal or allograft be required?
 Medialization of the acetabulum is well reported with good results.18
Medialization of the acetabulum is well reported with good results.18
 Cemented implants may be more appropriate in osteopenic bone.
Cemented implants may be more appropriate in osteopenic bone.
Implant Type
 Templating is essential to decide whether standard, revision, or custom-made implants are necessary. A knowledge of the range of implants available is essential (eg, implants for the Asia Pacific market are often much smaller than for Western implants).
Templating is essential to decide whether standard, revision, or custom-made implants are necessary. A knowledge of the range of implants available is essential (eg, implants for the Asia Pacific market are often much smaller than for Western implants).
 Nonprimary implants have been required in up to 40% of femoral deformity cases31; however, this is not our experience with cemented prostheses.
Nonprimary implants have been required in up to 40% of femoral deformity cases31; however, this is not our experience with cemented prostheses.
Implant Size
 The acetabulum is often small anteroposteriorly and the femoral canal is narrow.
The acetabulum is often small anteroposteriorly and the femoral canal is narrow.
Acetabulum
 Measure acetabular diameter on preoperative radiographs.
Measure acetabular diameter on preoperative radiographs.
 Ensure that small enough implants are available.
Ensure that small enough implants are available.
 This will also determine head size and may affect bearing selection.
This will also determine head size and may affect bearing selection.
 Use cemented for extremely small acetabula, and remove polyethylene from the anterior and posterior surface with a knife to fit.
Use cemented for extremely small acetabula, and remove polyethylene from the anterior and posterior surface with a knife to fit.
Femur
 Measure canal diameter on preoperative radiographs/CT.
Measure canal diameter on preoperative radiographs/CT.
 Organize custom stems if endosteum is very narrow or abnormally shaped.
Organize custom stems if endosteum is very narrow or abnormally shaped.
 Ensure that smaller stems are available to accommodate small, narrow femurs.
Ensure that smaller stems are available to accommodate small, narrow femurs.
 Longer stems should be available if subtrochanteric osteotomy is planned, fracture/perforation is a significant risk, or screw holes will be present in removed metalwork.
Longer stems should be available if subtrochanteric osteotomy is planned, fracture/perforation is a significant risk, or screw holes will be present in removed metalwork.
 Long stems must be slim to accommodate narrow femurs but long enough to bypass the osteotomy site, screw holes, and fracture site by two cortical diameters.
Long stems must be slim to accommodate narrow femurs but long enough to bypass the osteotomy site, screw holes, and fracture site by two cortical diameters.
 Usually, there is considerable anterior femoral bowing and stem entry, and length must be planned to avoid anterior perforation.
Usually, there is considerable anterior femoral bowing and stem entry, and length must be planned to avoid anterior perforation.
Other Hardware
 Retained metalwork
Retained metalwork
Metalwork is often still in situ from previous realignment, joint-sparing procedures, or fracture fixation.
Identify manufacturers and ensure that appropriate removal instrumentation is present.
Ensure that metal cutting equipment is available.
If plates are overgrown, consider retaining the plate but removing screws (see FIG 4).
Consider subtrochanteric femoral osteotomy to remove retained screws under direct vision.
 Wiring systems
Wiring systems
Required for diaphyseal fracture prophylaxis if using cementless stem
Need to be available due to the high rate of intraoperative fracture (particularly when using cementless stems)
 Osteotomy stabilization
Osteotomy stabilization
Plate and unicortical screws for subtrochanteric osteotomy stabilization
Temporary double plating to allow insertion may be necessary
Heterotopic Ossification Prophylaxis
 Consider if previous heterotropic ossification (HO), previous fracture surgery, or if trochanteric osteotomy is planned.
Consider if previous heterotropic ossification (HO), previous fracture surgery, or if trochanteric osteotomy is planned.
Consent
 Consent is to discuss with the patient the increased risk of complications (leg length, neurovascular complication, implant loosening, and fracture) and patient expectations need to be managed accordingly.
Consent is to discuss with the patient the increased risk of complications (leg length, neurovascular complication, implant loosening, and fracture) and patient expectations need to be managed accordingly.
Bilateral Deformity
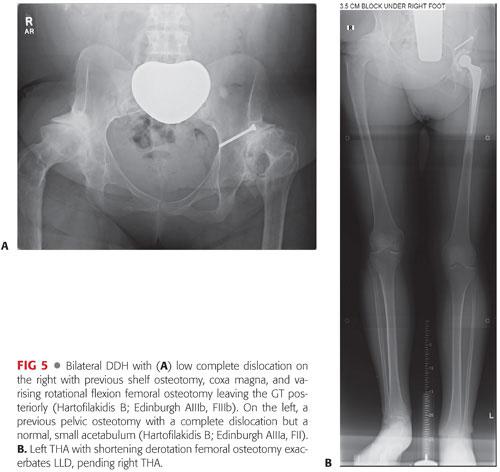
 In many cases, bilateral deformity exists, especially in DDH. Performing one THA may worsen LLD, and plans to schedule the second THA should be made early (see FIG 4) or acceptance of a shoe raise agreed (FIG 5).
In many cases, bilateral deformity exists, especially in DDH. Performing one THA may worsen LLD, and plans to schedule the second THA should be made early (see FIG 4) or acceptance of a shoe raise agreed (FIG 5).
Positioning
 The patient is placed in the lateral position with a posterior lumbosacral support and an anterior support placed on to the anterior superior iliac spine to stabilize the pelvis.
The patient is placed in the lateral position with a posterior lumbosacral support and an anterior support placed on to the anterior superior iliac spine to stabilize the pelvis.
Approach
 Skin incisions from previous surgery are used with scar excision where possible to improve cosmesis.
Skin incisions from previous surgery are used with scar excision where possible to improve cosmesis.
 A posterior approach maintains abductor integrity, provides a circumferential view of the acetabulum, and is extensile to facilitate femoral osteotomy. Performing trochanteric osteotomy may defunction abductors in these extreme cases (reattachment is difficult), and subtrochanteric osteotomy, although sometimes necessary prior to dislocation, creates multiple fragments which can be difficult to manage while preparing the acetabulum.
A posterior approach maintains abductor integrity, provides a circumferential view of the acetabulum, and is extensile to facilitate femoral osteotomy. Performing trochanteric osteotomy may defunction abductors in these extreme cases (reattachment is difficult), and subtrochanteric osteotomy, although sometimes necessary prior to dislocation, creates multiple fragments which can be difficult to manage while preparing the acetabulum.
TECHNIQUES
 Exposure
Exposure
A posterior approach, with the option of a direct anterior through the same incision, gives a circumferential view of the true acetabulum, preserves the abductors facilitating the soft tissue tension method for judging resection length in femoral osteotomy, and is extensile.
Combining the posterior and true anterior approaches allows accurate neck resection in situ (or debulking of the often anteriorly subluxed femoral head) under direct vision prior to dislocation. This is particularly important in the stiff, fixed, externally rotated hip, which cannot be accessed from the back alone (see FIG 1).
Occasionally, the head can be almost subcutaneous and removal of the anterior acetabular osteophyte is necessary to avoid impingement in flexion.
Iliopsoas release from lesser trochanter allows proximal femoral descent.
Total capsulectomy allows the proximal femur to be brought distally for hip center restoration.
The sciatic nerve is usually found running over the ischium and can be traced back to the sciatic notch. It need not be mobilized unless a previous pelvic osteotomy has caused scarring and adhesions.
The femoral bundle is rarely identified even when a direct anterior approach is added.
 Acetabular Reconstruction—Identifying the True Acetabulum in Severe DDH
Acetabular Reconstruction—Identifying the True Acetabulum in Severe DDH
Indication: DDH or proximal femoral focal deficiency (PFFD) is where the femoral head does not articulate with the true acetabulum (TECH FIG 1).
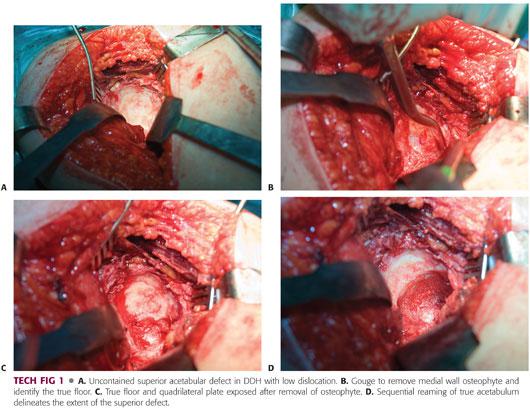
The femoral head may be articulating with a false acetabulum or may even be trapped in the abductor musculature in high dislocations.
In these circumstances, the true acetabulum is often small and triangular with a narrow entry. Overhanging osteophytes close down the entry, but the transverse ligament is a constant indicator of the true acetabulum location.
Medial osteophyte must be removed to identify the true floor.
 Acetabular Reconstruction—Femoral Head Autograft
Acetabular Reconstruction—Femoral Head Autograft
Indication: Recreating an anatomic hip center when the resulting position is associated with anterosuperior roof deficiency of greater than 20%.
The true acetabulum is prepared as for a standard cemented acetabular component (see TECH FIG 1). The final acetabular reamings are kept as graft for the procedure later.
The superior segmental defect is delineated by inserting a trial cup (TECH FIG 2A,B). The defect is prepared using gouges to remove fibrocartilage. The femoral head is similarly prepared by removing fibrocartilage.
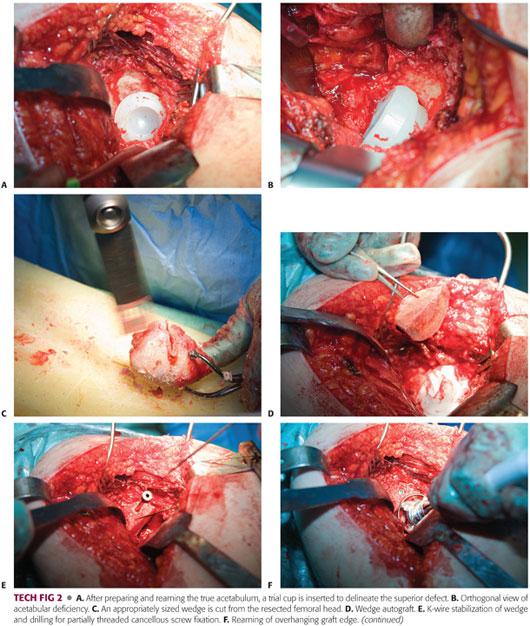
A generous wedge of the resected femoral head, which came from the defect, is cut (TECH FIG 2C,D) and placed with its sclerotic convexity against the prepared concave defect with the reamings from the true acetabulum placed in the bed to improve contact. This is held temporarily with a K-wire (TECH FIG 2E) and fixed with two superiorly placed partially threaded cancellous screws.
Any autograft overhanging the true acetabulum is then reamed away (TECH FIG 2F), leaving an acetabular bulk autograft supported by host bone and a contained socket into which a standard acetabular component can be cemented using third-generation cementing techniques (TECH FIG 2G,H).
 Femoral Reconstruction—Subtrochanteric Shortening Osteotomy
Femoral Reconstruction—Subtrochanteric Shortening Osteotomy
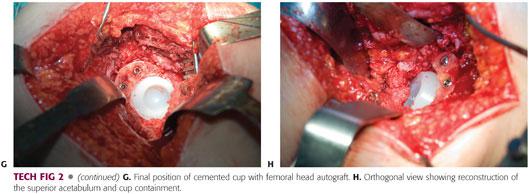
Indication: When recreating an anatomic hip center, subtrochanteric shortening osteotomy will lengthen the lower limb by greater than 3 cm with risk of sciatic nerve palsy.
Femoral length, angulation, and GT position can be addressed concurrently using this technique.
It reduces the need for custom implants (although small sizes may be required) and restores lower limb mechanical alignment.
Single-plane osteotomy is easier for correction of complex deformity than a stepped osteotomy and requires a shorter stem to bypass it by a minimum of two shaft diameters.
Perform acetabular implantation first.
Identify the level for osteotomy distal to the lesser trochanter.
Create a transverse osteotomy perpendicular to the shaft (TECH FIG 3A).
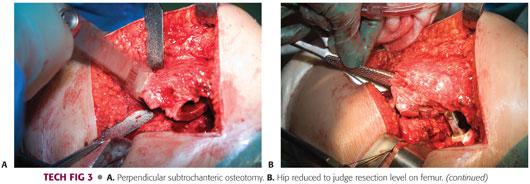
The proximal femoral fragment is prepared with serial rasps to accept the femoral component which best fits with the largest offset. A burr can be used in a retrograde manner at the osteotomy site to aid this.
The proximal fragment with rasp and trial head in situ is reduced into the acetabulum (TECH FIG 3B).
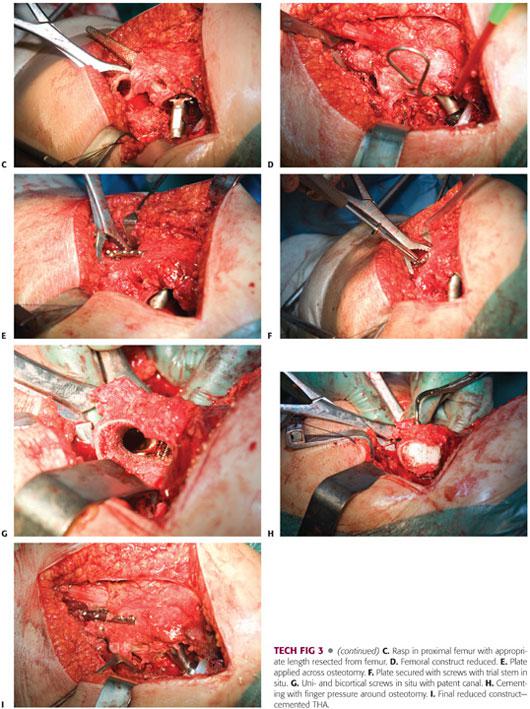
Longitudinal traction is applied to the distal fragment and the amount of overlap of proximal and distal fragments is noted and marked. This length is resected perpendicular to the diaphysis (TECH FIG 3C). The burr can then be used in an antegrade fashion on the distal fragment if needed to remove any sclerotic or stenotic bone under direct vision.
The resultant bone ends are opposed, and any rotational correction is made to align the GT 15 degrees from orthogonal to the transepicondylar axis of the knee. This restores the anatomic alignment of the direction of pull of the abductors with the transepicondylar knee axis.
The appropriate femoral trial is then inserted and passed across the osteotomy and the osteotomy compressed with fracture reduction forceps (TECH FIG 3D).
A 5- or 6-hole, one-third tubular plate or dynamic compression plate (DCP) is applied posteriorly with a combination of unicortical and bicortical screws as the in situ femoral trial allows (TECH FIG 3E–G). If the osteotomy is unstable, a temporary 2-hole plate can be applied at right angles to stabilize the construct temporarily.
The stem is then cemented using third-generation techniques while the assistant’s fingers wrap around the femur anteriorly at the osteotomy site to prevent cement extrusion and provide tension against the plate and thus anterior compression at the osteotomy (TECH FIG 3H,I).
After curing, morselized autologous graft is packed around the osteotomy site and the plate is left in situ.
 Femoral Reconstruction—Subtrochanteric Osteotomy with Derotation and angulation
Femoral Reconstruction—Subtrochanteric Osteotomy with Derotation and angulation
Indication: Angular deformity of femur requiring correction in order to implant stem and correct mechanical axis
It is similar to shortening osteotomy, except the osteotomy made in the distal fragment should be oblique to correct angulation (TECH FIG 4B).
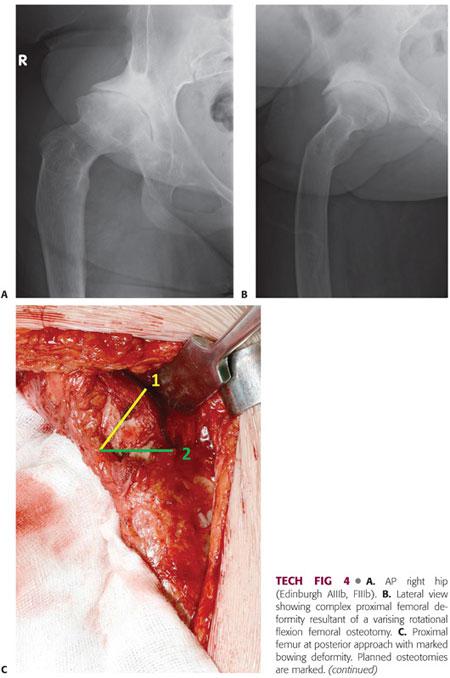
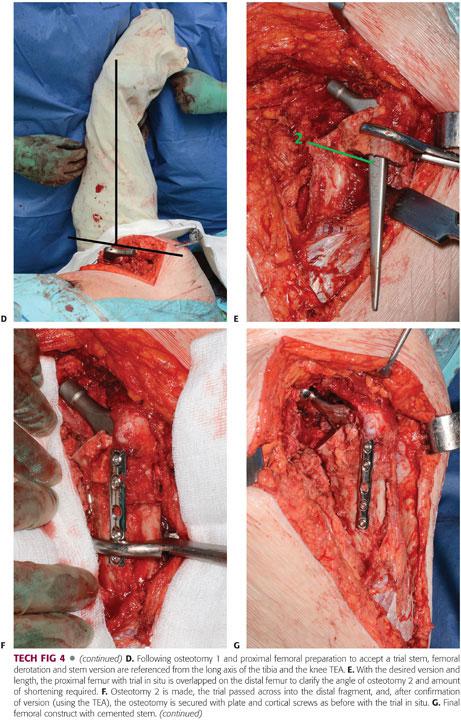

The distal part has longitudinal traction applied, and the GT proximally is placed in the transepicondylar plane as before (TECH FIG 4C). The obliquity of the required osteotomy is determined by the overlap of the proximal osteotomy with the distal fragment (TECH FIG 4D). This is marked and the bone is resected accordingly.
The distal fragment is prepared as before and the osteotomy is stabilized with a plate as before (TECH FIG 4E–G).
PEARLS AND PITFALLS | |
| |
| |
| |
| |
| |
POSTOPERATIVE CARE
 Where structural autograft or femoral osteotomy has been used, patients should be partial weight bearing for 6 weeks with standard posterior approach dislocation precautions.
Where structural autograft or femoral osteotomy has been used, patients should be partial weight bearing for 6 weeks with standard posterior approach dislocation precautions.
OUTCOMES
 In addition to being technically difficult cases, patients with deformity are young and active and often have multiple operations. As such, THA performed for severe deformity is associated with more complications and worse survivorship when compared to standard primary THA.
In addition to being technically difficult cases, patients with deformity are young and active and often have multiple operations. As such, THA performed for severe deformity is associated with more complications and worse survivorship when compared to standard primary THA.
 Arthroplasty register data have suggested that after adjusting for age, there is no significant difference in revision risk for THA performed for sequelae of pediatric hip disease compared to THA performed for OA, with a 10-year survival rate of 93.6% compared to 93.8%.14 However, more revisions were performed within 6 months in the pediatric hip disease group, with significantly more revisions for dislocation.14 These data do not consider the severity of deformity, which individual series have shown to be a key determinant of outcome.
Arthroplasty register data have suggested that after adjusting for age, there is no significant difference in revision risk for THA performed for sequelae of pediatric hip disease compared to THA performed for OA, with a 10-year survival rate of 93.6% compared to 93.8%.14 However, more revisions were performed within 6 months in the pediatric hip disease group, with significantly more revisions for dislocation.14 These data do not consider the severity of deformity, which individual series have shown to be a key determinant of outcome.
 In DDH, mild deformity (eg, dysplasia without dislocation) rarely requires special techniques for deformity correction and is associated with THA survival comparable to that without deformity, with a 90% 15-year survival rate.19 Worse deformity with dislocation (low or high) is associated with higher rates of failure and the 15-year survival rate reduces to 75%.21
In DDH, mild deformity (eg, dysplasia without dislocation) rarely requires special techniques for deformity correction and is associated with THA survival comparable to that without deformity, with a 90% 15-year survival rate.19 Worse deformity with dislocation (low or high) is associated with higher rates of failure and the 15-year survival rate reduces to 75%.21
 Using the technique of structural roof allograft to treat severe acetabular dysplasia, 10-year survivorship for aseptic loosening is reported as 80% to 100% when combined with cemented cups5,23,32,40 and 91% to 100% with cementless.22,26,39 Longer term, 12- to 15-year survival of 65% to 96% is reported with cemented cups.1,13,24,29,37
Using the technique of structural roof allograft to treat severe acetabular dysplasia, 10-year survivorship for aseptic loosening is reported as 80% to 100% when combined with cemented cups5,23,32,40 and 91% to 100% with cementless.22,26,39 Longer term, 12- to 15-year survival of 65% to 96% is reported with cemented cups.1,13,24,29,37
 When a subtrochanteric osteotomy is used, studies with mean follow-up of greater than 5 years have shown femoral stem survival of 90% to 100% when a cementless stem is used8,15,30,33,35 and 80% to 91% with a cemented stem.9,23,30 Osteotomy union of 93% to 100% is reported with cementless stems8,15,30,33,35 and 90% to 97% with cemented stems.23,30
When a subtrochanteric osteotomy is used, studies with mean follow-up of greater than 5 years have shown femoral stem survival of 90% to 100% when a cementless stem is used8,15,30,33,35 and 80% to 91% with a cemented stem.9,23,30 Osteotomy union of 93% to 100% is reported with cementless stems8,15,30,33,35 and 90% to 97% with cemented stems.23,30
 Registry data have confirmed that there is no difference in the revision rate of short, cemented, collarless tapered stems (n = 1898; 7-year survival rate of 96.6%) compared to that of standard length stems (n = 39,956; 7-year survival of 96.5%) despite their use in a greater proportion of difficult DDH cases.10 Concerns regarding the biomechanical strength and stability of these slighter stems have not been confirmed, with no documented cases of stem fracture and no increase in aseptic loosening.
Registry data have confirmed that there is no difference in the revision rate of short, cemented, collarless tapered stems (n = 1898; 7-year survival rate of 96.6%) compared to that of standard length stems (n = 39,956; 7-year survival of 96.5%) despite their use in a greater proportion of difficult DDH cases.10 Concerns regarding the biomechanical strength and stability of these slighter stems have not been confirmed, with no documented cases of stem fracture and no increase in aseptic loosening.
 Using a variety of cementless stems in the management of proximal femoral deformity, Mortazavi et al31 reported a mechanical failure rate (loose or revised) of 9% at 4 years. Twenty-one out of 58 (36%) required an osteotomy for exposure or deformity correction.
Using a variety of cementless stems in the management of proximal femoral deformity, Mortazavi et al31 reported a mechanical failure rate (loose or revised) of 9% at 4 years. Twenty-one out of 58 (36%) required an osteotomy for exposure or deformity correction.
 Failure to restore the true hip center by positioning the acetabular component proximally and laterally increases the joint reaction force4 and shearing forces on the cup25 and does not restore the abductor moment arm. Cups placed 15 mm superiorly have significantly higher rates of aseptic loosening and revision of both acetabular and femoral components when compared to implants where the center of rotation has been anatomically restored.36
Failure to restore the true hip center by positioning the acetabular component proximally and laterally increases the joint reaction force4 and shearing forces on the cup25 and does not restore the abductor moment arm. Cups placed 15 mm superiorly have significantly higher rates of aseptic loosening and revision of both acetabular and femoral components when compared to implants where the center of rotation has been anatomically restored.36
 Data on custom-made implants are difficult to interpret and long-term data are lacking. Medium-term follow-up of 48 cementless custom stems showed a survival rate of 96% at 4 years with failures due to early aseptic loosening.27 Follow-up of 70 different custom-made cementless stems reports a 99% (95% confidence interval, 90 to 100) 12-year survival rate with no femoral loosening up to 16 years.
Data on custom-made implants are difficult to interpret and long-term data are lacking. Medium-term follow-up of 48 cementless custom stems showed a survival rate of 96% at 4 years with failures due to early aseptic loosening.27 Follow-up of 70 different custom-made cementless stems reports a 99% (95% confidence interval, 90 to 100) 12-year survival rate with no femoral loosening up to 16 years.
 Previous proximal femoral osteotomy adversely affects THA outcomes with an intraoperative complication rate of 11% to 23%,6,16 increased risk of infection and septic THA failure rate of 8% at 5 to 10 years,14 and an overall failure rate of 21% at 10 years in 215 patients.16
Previous proximal femoral osteotomy adversely affects THA outcomes with an intraoperative complication rate of 11% to 23%,6,16 increased risk of infection and septic THA failure rate of 8% at 5 to 10 years,14 and an overall failure rate of 21% at 10 years in 215 patients.16
COMPLICATIONS
 Compared to THA for primary OA, there is a greater risk of complications when THA is performed in the presence of deformity:
Compared to THA for primary OA, there is a greater risk of complications when THA is performed in the presence of deformity:
The intraoperative fracture or femoral perforation rate is 5% to 22%.
The dislocation rate is 6% to 7%.23,28
The osteotomy nonunion rate is 3% to 7%.9,23,28
The nerve palsy rate is 1% to 5%.3,6,16,23,27,36
Residual LLD may still be present.34
REFERENCES
1. Akiyama H, Kawanabe K, Iida H, et al. Long-term results of cemented total hip arthroplasty in developmental dysplasia with acetabular bulk bone grafts after improving operative techniques. J Arthroplasty 2010;25(5):716–720.
2. Berry DJ. Total hip arthroplasty in patients with proximal femoral deformity. Clin Orthop Relat Res 1999;(369):262–272.
3. Biant LC, Bruce WJ, Assini JB, et al. The anatomically difficult primary total hip replacement: medium- to long-term results using a cementless odular stem. J Bone Joint Surg Br 2008;90(4):430–435.
4. Bicanic G, Delimar D, Delimar M, et al. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop 2009;33(2):397–402.
5. Bobak P, Wroblewski BM, Siney PD, et al. Charnley low-friction arthroplasty with an autograft of the femoral head for developmental dysplasia of the hip. The 10- to 15-year results. J Bone Joint Surg Br 2000;82(4):508–511.
6. Boos N, Krushell R, Ganz R, et al. Total hip arthroplasty after previous proximal femoral osteotomy. J Bone Joint Surg Br 1997;79(2): 247–253.
7. Busch VJ, Clement ND, Mayer PF, et al. High survivorship of cemented sockets with roof graft for severe acetabular dysplasia. Clin Orthop Relat Res 2012;470(11)3032–3040.
8. Chareancholvanich K, Becker DA, Gustilo RB. Treatment of congenital dislocated hip by arthroplasty with femoral shortening. Clin Orthop Relat Res 1999;(360):127–135.
9. Charity JA, Tsiridis E, Sheeraz A, et al. Treatment of Crowe IV high hip dysplasia with total hip replacement using the Exeter stem and shortening derotational subtrochanteric osteotomy. J Bone Joint Surg Br 2011;93:34–38.
10. Choy GG, Roe JA, Whitehouse SL, et al. Exeter short stems compared with standard length Exeter stems: experience from the Australian Orthopaedic Association National Joint Replacement Registry. J Arthroplasty 2013;28:103–109.
11. D’Antonio JA, Capello WN, Borden LS, et al. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res 1989;(243):126–137.
12. D’Antonio J, McCarthy JC, Bargar WL, et al. Classification of femoral abnormalities in total hip arthroplasty. Clin Orthop Relat Res 1993;(296):133–139.
13. de Jong PT, Haverkamp D, van der Vis HM, et al. Total hip replacement with a superolateral bone graft for osteoarthritis secondary to dysplasia: a long-term follow-up. J Bone Joint Surg Br 2006;88(2):173–178.
14. Engesaeter LB, Engesaeter IO, Fenstad AM, et al. Low revision rate after total hip arthroplasty in patients with pediatric hip diseases. Acta Orthop 2012;83(5):436–441.
15. Eskelinen A, Helenius I, Remes V, et al. Cementless total hip arthroplasty in patients with high congenital hip dislocation. J Bone Joint Surg Am 2006;88:80–91.
16. Ferguson GM, Cabanela ME, Ilstrup DM. Total hip arthroplasty after failed intertrochanteric osteotomy. J Bone Joint Surg Br 1994; 76(2):252–257.
17. Gaston MS, Gaston P, Donaldson P, et al. A new classification system for the adult dysplastic hip requiring total hip arthroplasty: a reliability study. Hip Int 2009;19(2):96–101.
18. Hartofilakidis G, Babis GC, Lampropoulou-Adamidou K, et al. Results of total hip arthroplasty differ in subtypes of high dislocation. Clin Orthop Relat Res 2013;471(9):2972–2979.
19. Hartofilakidis G, Karachalios T. Total hip arthroplasty for congenital hip disease. J Bone Joint Surg Am 2004:86(2):242–250.
20. Hartofilakidis G, Karachalios T, Georgiades G. Total hip arthroplasty in patients with high dislocation: a concise follow-up, at a minimum of fifteen years, of previous reports. J Bone Joint Surg Am 2011;93(17):1614–1618.
21. Hartofilakidis G, Stamos K, Karachalios T. Treatment of high dislocation of the hip in adults with total hip arthroplasty. Operative technique and long-term clinical results. J Bone Joint Surg Am 1998;80(4):510–517.
22. Hendrich C, Mehling I, Sauer U, et al. Cementless acetabular reconstruction and structural bone-grafting in dysplastic hips. J Bone Joint Surg Am 2006;88(2):387–394.
23. Howie CR, Ohly NE, Miller B. Cemented total hip arthroplasty with subtrochanteric osteotomy in dysplastic hips. Clin Orthop Relat Res 2010;468(12):3240–3247.
24. Iida H, Matsusue Y, Kawanabe K, et al. Cemented total hip arthroplasty with acetabular bone graft for developmental dysplasia. Long-term results and survivorship analysis. J Bone Joint Surg Br 2000;82(2):176–184.
25. Karachalios T, Hartofilakidis G. Congenital hip disease in adults: terminology, classification, pre-operative planning and management. J Bone Joint Surg Br 2010;92(7):914–921.
26. Kim M, Kadowaki T. High long-term survival of bulk femoral head autograft for acetabular reconstruction in cementless THA for developmental hip dysplasia. Clin Orthop Relat Res 2010;468(6):1611–1620.
27. Koulouvaris P, Stafylas K, Sculco T, et al. Custom-design implants for severe distorted proximal anatomy of the femur in young adults followed for 4-8 years. Acta Orthop 2008;79(2):203–210.
28. Krych AJ, Howard JL, Trousdale RT, et al. Total hip arthroplasty with shortening subtrochanteric osteotomy in Crowe type-IV developmental dysplasia: surgical technique. J Bone Joint Surg Am 2010;92 (suppl 1):176–187.
29. Lee BP, Cabanela ME, Wallrichs SL, et al. Bone-graft augmentation for acetabular deficiencies in total hip arthroplasty. Results of long-term follow-up evaluation. J Arthroplasty 1997;12(5):503–510.
30. Masonis JL, Patel JV, Miu A, et al. Subtrochanteric shortening and derotational osteotomy in primary total hip arthroplasty for patients with severe hip dysplasia: 5-year follow-up. J Arthroplasty 2003;18 (3 suppl 1):68–73.
31. Mortazavi SM, Restrepo C, Kim PJ, et al. Cementless femoral reconstruction in patients with proximal femoral deformity. J Arthroplasty 2011;26(3):354–359.
32. Mulroy RD Jr, Harris WH. Failure of acetabular autogenous grafts in total hip arthroplasty. Increasing incidence: a follow-up note. J Bone Joint Surg Am 1990;72(10):1536–1540.
33. Nagoya S, Kaya M, Sasaki M, et al. Cementless total hip replacement with subtrochanteric femoral shortening for severe developmental dysplasia of the hip. J Bone Joint Surg Br 2009;91(9):1142–1147.
34. Oe K, Iida H, Nakamura T, et al. Subtrochanteric shortening osteotomy combined with cemented total hip arthroplasty for Crowe group IV hips. Arch Orthop Trauma Surg 2013;133(12):1763–1770.
35. Onodera S, Majima T, Ito H, et al. Cementless total hip arthroplasty using the modular S-ROM prosthesis combined with corrective proximal femoral osteotomy. J Arthroplasty 2006;21(5):664–669.
36. Pagnano W, Hanssen AD, Lewallen DG, et al. The effect of superior placement of the acetabular component on the rate of loosening after total hip arthroplasty. J Bone Joint Surg Am 1996;78(7); 1004–1014.
37. Rodriguez JA, Huk OL, Pellicci PM, et al. Autogenous bone grafts from the femoral head for the treatment of acetabular deficiency in primary total hip arthroplasty with cement. Long-term results. J Bone Joint Surg Am 1995;77(8):1227–1233.
38. Schmidutz F, Bierer M, Weber P, et al. Biomechanical reconstruction of the hip: comparison between modular short-stem hip arthroplasty and conventional total hip arthroplasty. Int Orthop 2012;36(7):1341–1347.
39. Shetty AA, Sharma P, Singh S, et al. Bulk femoral-head autografting in uncemented total hip arthroplasty for acetabular dysplasia: results at 8 to 11 years follow-up. J Arthroplasty 2004;19(6):706–713.
40. Stringa G, Pitto RP, Di Muria GV, et al. Total hip replacement with bone grafting using the removed femoral head in severe acetabular dysplasia. Int Orthop 1995;19(2):72–76.
41. Tamegai H, Otani T, Fujii H, et al. A modified S-ROM stem in primary total hip arthroplasty for developmental dysplasia of the hip. J Arthroplasty 2013;28(10):1741–1745.
< div class='tao-gold-member'>








