The loss of acetabular bone stock remains a major challenge in revision hip surgery.
 The three main causes of acetabular bone loss encountered in revision hip surgery are aseptic loosening due to osteolysis, bone loss due to infection, and iatrogenic loss encountered during implant removal.
The three main causes of acetabular bone loss encountered in revision hip surgery are aseptic loosening due to osteolysis, bone loss due to infection, and iatrogenic loss encountered during implant removal.
 The use of large amounts of bone cement in isolation for the reconstruction of acetabular defects in revision hip surgery has poor results, with high rates of early loosening.
The use of large amounts of bone cement in isolation for the reconstruction of acetabular defects in revision hip surgery has poor results, with high rates of early loosening.
 Impaction grafting has the ability to restore anatomy and bone stock with histologic incorporation of graft.
Impaction grafting has the ability to restore anatomy and bone stock with histologic incorporation of graft.
 Acetabular impaction grafting (AIG) is defined as vigorous forceful impaction of cancellous bone chips using specially designed instruments to achieve a solid bed of bone into which polymer bone cement can be pressurized prior to insertion of a polyethylene acetabular component.
Acetabular impaction grafting (AIG) is defined as vigorous forceful impaction of cancellous bone chips using specially designed instruments to achieve a solid bed of bone into which polymer bone cement can be pressurized prior to insertion of a polyethylene acetabular component.
 True AIG requires the use of a cemented polyethylene acetabular component. Graft used in combination with uncemented shells serves only as a void filler and cannot be loaded in the same physiologic manner.
True AIG requires the use of a cemented polyethylene acetabular component. Graft used in combination with uncemented shells serves only as a void filler and cannot be loaded in the same physiologic manner.
 Impaction bone grafting is ideal for cavitary defects and can be used in extensive segmental defects, providing that stable containment of the graft can be achieved.
Impaction bone grafting is ideal for cavitary defects and can be used in extensive segmental defects, providing that stable containment of the graft can be achieved.
 Stainless steel mesh fixed with small fragment screws can be used to convert segmental defects (medial wall or peripheral) into contained cavitary defects suitable for impaction grafting. Alternatively, porous metal wedges may be used to create a contained defect.6
Stainless steel mesh fixed with small fragment screws can be used to convert segmental defects (medial wall or peripheral) into contained cavitary defects suitable for impaction grafting. Alternatively, porous metal wedges may be used to create a contained defect.6
 Adequate pressurization of cement into impacted bone graft creates a composite with immediate mechanical stability, promoting bone remodeling, and restoration of bone stock.
Adequate pressurization of cement into impacted bone graft creates a composite with immediate mechanical stability, promoting bone remodeling, and restoration of bone stock.
 AIG has shown good long-term results.5,12–15,18
AIG has shown good long-term results.5,12–15,18
 Standard implants and modern cementing techniques are used.
Standard implants and modern cementing techniques are used.
ANATOMY
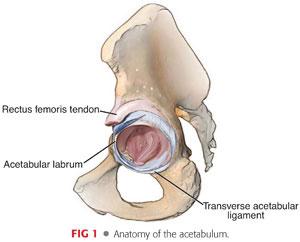
 The acetabulum is a complex three-dimensional structure with two thick columns of bone, one anteriorly and one posteriorly, and thinner walls superiorly and medially, which contain the socket.
The acetabulum is a complex three-dimensional structure with two thick columns of bone, one anteriorly and one posteriorly, and thinner walls superiorly and medially, which contain the socket.
 It is important to identify relevant landmarks intraoperatively, such as the transverse acetabular ligament, the true floor (medial wall), anterior and posterior walls and columns, and superior dome (FIG 1).
It is important to identify relevant landmarks intraoperatively, such as the transverse acetabular ligament, the true floor (medial wall), anterior and posterior walls and columns, and superior dome (FIG 1).
 AIG combined with a cemented polyethylene cup allows for the restoration of the hip center and normal hip biomechanics.
AIG combined with a cemented polyethylene cup allows for the restoration of the hip center and normal hip biomechanics.
PATHOGENESIS
 Although autograft is the ideal material for AIG, a limited natural supply necessitates the use of allograft.
Although autograft is the ideal material for AIG, a limited natural supply necessitates the use of allograft.
 Animal studies show that impacted, morselized fresh frozen allograft bone incorporates into new bone.11
Animal studies show that impacted, morselized fresh frozen allograft bone incorporates into new bone.11
 Twenty-four acetabular bone biopsy specimens were obtained from 20 patients who had undergone acetabular reconstruction with impaction bone grafting.16
Twenty-four acetabular bone biopsy specimens were obtained from 20 patients who had undergone acetabular reconstruction with impaction bone grafting.16
Biopsy specimens were obtained at 3 months to 15 years.
Histology showed rapid revascularization of the graft followed by osteoclastic resorption and woven bone formation on the graft remnants.
A mixture of graft, new bone, and fibrin remodeled completely into a new trabecular structure, with normal lamellar bone and only scarce remnants of graft material.
Localized areas of nonincorporated bone graft surrounded by fibrous tissue remained despite the follow-up period.
Large nonincorporated fragments of cartilage were also found in cases in which femoral head bone chips were produced by a bone mill.
 Allograft is an osteoconductive material, acting as a scaffold for new bone formation. However, histologic studies have shown that new bone forms within the stromal tissue, indicating that osteoinduction may also play a role, although the exact mechanism by which this occurs is unclear.
Allograft is an osteoconductive material, acting as a scaffold for new bone formation. However, histologic studies have shown that new bone forms within the stromal tissue, indicating that osteoinduction may also play a role, although the exact mechanism by which this occurs is unclear.
 Despite the contact between bone graft and cement, the bone graft retains its biologic and mechanical viability and healing potential.9
Despite the contact between bone graft and cement, the bone graft retains its biologic and mechanical viability and healing potential.9
 Reports on AIG show promising intermediate and long-term results.5,8,12–15,18
Reports on AIG show promising intermediate and long-term results.5,8,12–15,18
PATIENT HISTORY AND PHYSICAL FINDINGS
 As usual, a thorough history and examination is essential, including a clear understanding of the previous hip surgery and the reasons behind failure.
As usual, a thorough history and examination is essential, including a clear understanding of the previous hip surgery and the reasons behind failure.
 Infection is considered a relative contraindication and any suspicion of this should be thoroughly investigated in the usual fashion. Rudelli et al10 reported their series of the use of impaction bone grafting in one-stage revisions. They reported the following:
Infection is considered a relative contraindication and any suspicion of this should be thoroughly investigated in the usual fashion. Rudelli et al10 reported their series of the use of impaction bone grafting in one-stage revisions. They reported the following:
A 6.2% recurrence of infection at 8.6 years in 32 patients
Of these patients, 25 underwent impaction grafting of both the femur and acetabulum, and half required the use of mesh to contain the graft.
These results are similar to those reported using a two-stage procedure.
 Physical examination should include examination for previous incisions, sinus tracts, range of motion, contractures, leg length discrepancy, and neurovascular status.
Physical examination should include examination for previous incisions, sinus tracts, range of motion, contractures, leg length discrepancy, and neurovascular status.
 Records of previous surgeries should be obtained, including details of previous implants.
Records of previous surgeries should be obtained, including details of previous implants.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 The initial diagnostic imaging examination should begin with standard anteroposterior (AP) pelvis and AP and lateral radiographs of the affected hip.
The initial diagnostic imaging examination should begin with standard anteroposterior (AP) pelvis and AP and lateral radiographs of the affected hip.
 Oblique Judet views can be extremely useful to assess column and wall defects.
Oblique Judet views can be extremely useful to assess column and wall defects.
 A computed tomography (CT) scan may be helpful in identifying bone loss and structural defects, although metal artifacts can make interpretation difficult.
A computed tomography (CT) scan may be helpful in identifying bone loss and structural defects, although metal artifacts can make interpretation difficult.
 The actual bone defects or bone loss may be more severe than preoperative radiographic studies reveal.17
The actual bone defects or bone loss may be more severe than preoperative radiographic studies reveal.17
 A preoperative workup for infection should be performed, including aspiration or biopsy as required.
A preoperative workup for infection should be performed, including aspiration or biopsy as required.
NONOPERATIVE MANAGEMENT
 Nonoperative management is only considered for patients who are not able to tolerate a revision operation or able to comply with the postoperative instructions. In these cases, excision arthroplasty with removal of any loose components may be a reasonable option as a pain-relieving procedure.
Nonoperative management is only considered for patients who are not able to tolerate a revision operation or able to comply with the postoperative instructions. In these cases, excision arthroplasty with removal of any loose components may be a reasonable option as a pain-relieving procedure.
 Alternative methods of fixation include cemented acetabular revision, revision with structural allograft, uncemented acetabular components with structural allograft, uncemented components with metal augments, jumbo acetabular components, and trabecular metal acetabular components.
Alternative methods of fixation include cemented acetabular revision, revision with structural allograft, uncemented acetabular components with structural allograft, uncemented components with metal augments, jumbo acetabular components, and trabecular metal acetabular components.
 In cases of pelvic discontinuity or severe anterior or posterior column defects, alternative techniques of reconstruction such as cages, plates and screws, or trabecular metal implants may be necessary.
In cases of pelvic discontinuity or severe anterior or posterior column defects, alternative techniques of reconstruction such as cages, plates and screws, or trabecular metal implants may be necessary.
SURGICAL MANAGEMENT
Preoperative Planning
 One of the benefits of AIG is the ability to recreate anatomy by restoring the center of rotation to the correct level.
One of the benefits of AIG is the ability to recreate anatomy by restoring the center of rotation to the correct level.
 Precise preoperative templating is necessary to plan the requirement for reconstruction of segmental defects and to assess cavitary defects in order to ensure anatomic positioning of the acetabular component.
Precise preoperative templating is necessary to plan the requirement for reconstruction of segmental defects and to assess cavitary defects in order to ensure anatomic positioning of the acetabular component.
Positioning
 The patient is positioned according to the surgeon’s preference and planned surgical approach. This technique is applicable to most patient positions and surgical techniques.
The patient is positioned according to the surgeon’s preference and planned surgical approach. This technique is applicable to most patient positions and surgical techniques.
Approach
 Any surgical approach that allows full acetabular exposure can be used. It is important that the surgeon uses an approach that is both familiar and extensile.
Any surgical approach that allows full acetabular exposure can be used. It is important that the surgeon uses an approach that is both familiar and extensile.
 Extensile approaches that allow good visualization of the posterior column are favored, as this facilitates the reconstruction of segmental defects.
Extensile approaches that allow good visualization of the posterior column are favored, as this facilitates the reconstruction of segmental defects.
TECHNIQUES
 Acetabular Exposure
Acetabular Exposure
Circumferential exposure of the acetabulum for the assessment of bony deficiencies is essential.
Releases that may facilitate acetabular exposure include release of gluteus maximus tendon from the femur, release of the iliofemoral ligament and reflected head of rectus from the superoanterior acetabulum, and release of iliopsoas tendon.
Removal of the femoral stem can also facilitate exposure. Cemented taper slip femoral stem can be tapped out of the intact mantle and replaced following reconstruction using a cement-in-cement technique.3
The previous acetabular components are removed using traditional implant removal techniques. Particular attention must be taken to avoid additional bone loss.
All residual cement and fibrous tissue must be removed using small burrs and curettes, taking care to preserve the thin acetabular walls (TECH FIG 1).

In the cases of medial defects, the membrane here can be left intact as removal may risk damaging intrapelvic structures.
Identification of the transverse acetabular ligament, if present, can be a useful landmark for positioning of the revised component.
Following exposure, the bony anatomy is assessed and acetabular defects are identified.
As soon as the defect has been assessed and its suitability for AIG is confirmed, it is advisable to remove the autograft femoral heads from the freezer and allow these to defrost in warm saline.
 Acetabular Preparation
Acetabular Preparation
The use of acetabular reamers should be kept to a minimum to avoid removing host bone and damaging thin acetabular walls. Areas of sclerotic bone that are not bleeding can be burred gently or drilled with a 2-mm drill bit to encourage bleeding, which may improve graft incorporation.
In order to assess acetabular defects and to determine whether containment is required, it is useful to hold a trial component in the intended inclination and anteversion at the level of the transverse acetabular ligament (TECH FIG 2A).

For purely cavitary defects, no further reconstruction with mesh is required and impaction can begin.
Peripheral segmental defects require containment using stainless steel rim meshes (X-change Revision Instrument System, Stryker Orthopaedics, Mahwah, NJ) that can be cut to size, ensuring sharp edges are not placed posteriorly where they might risk injury to the sciatic nerve, and secured to the acetabular rim using multiple small fragment screws placed at 1-cm intervals along the acetabular wall. It is useful to secure the mesh at the apex initially and, after rotating the mesh to the correct anteversion, screws can be placed at the anterior and posterior corners and then in the intervals (TECH FIG 2B).
Porous metal wedges may be used in peripheral defects to create a contained defect for impaction grafting.
When securing peripheral meshes, it is useful to place an appropriately sized impactor in the acetabulum to ensure the mesh or wedge is appropriately oriented and the defect is adequately contained.
Medial segmental defects are common and require reinforcement prior to impaction. Specific medial meshes can be cut to size and gently impacted medially. The placement of a thin wafer of femoral head or cancellous bone chips can be placed medially to stabilize the mesh. If required, additional stability can be achieved using two or three small fragment screws.
Anterior wall defects can also be contained with a small mesh, although in these circumstances, the mesh is secured to the inner surface of the acetabulum.
Large defects that require use of the large rim mesh should be carefully assessed, as results have shown higher failure rates with larger rim meshes, probably due to the difficulty in achieving stable containment.5,18 Alternative methods of reconstruction may be required in these cases.
 Preparation of Bone Graft
Preparation of Bone Graft
In revision cases, sufficient autograft is rarely available. In these cases, fresh frozen femoral heads are the preferred choice.
The graft can be prepared either by hand, using large rongeurs, or using a commercially available bone mill as long as appropriate size chips can be produced.
Better stability has been shown with larger bone chips and a 7- to 10-mm bone chip is recommended,1 in contrast to the smaller bone graft size used with femoral impaction grafting.
Most commercially available bone mills are not capable of producing bone chips of this larger size; therefore, we recommend handmade bone chips.
In addition to larger chip size, pulsatile lavage can be used to clean the graft after morselization and this has also been shown to improve stability of the impacted graft.1,4
 Acetabular Bone Reconstruction
Acetabular Bone Reconstruction
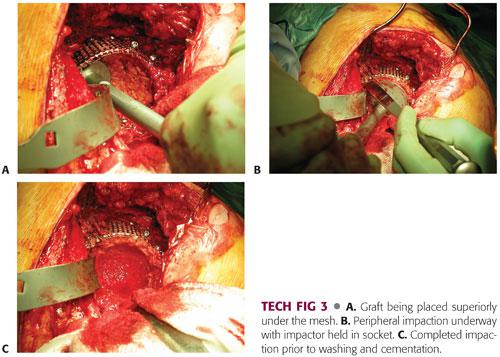
Bone chips are introduced into the acetabulum and impacted in layers.
It is important to fill superior defects first (TECH FIG 3A) using small impactors to fill small cavitary defects and work around any screws that may be passing across the defect.
It is a technical mistake to place too much graft medially, resulting in lateralization of the final acetabular component.
Reverse reaming with an acetabular reamer should not be used. This technique has demonstrated inferior results with less graft stability.2
Impaction using hemispherical acetabular impactors needs to be vigorous—forceful enough to ensure a stable bed of graft but not so forceful as to fracture the acetabulum.
Once the main defect has been filled, more chips should be placed at the periphery and impacted. Impaction in the periphery should continue until it is no longer possible to insert more bone chips (TECH FIG 3B). In order to facilitate this, the final impactor can be backed off by 1 or 2 mm. Once peripheral impaction is complete, hammer the impactor back into place.
The final impactor should be 4 to 6 mm larger than the outer diameter of the planned acetabular component to allow for an adequate cement mantle.
Following final impaction, the bone bed should have the consistency of cortical bone (TECH FIG 3C).
Pulse lavage can be used to clean the graft bed, but the graft should be protected using a mesh or slotted spoon.
 Cemented Cup Insertion
Cemented Cup Insertion
Hydrogen peroxide–soaked gauzes can be placed in the acetabulum to clean the graft surface while the polymethylmethacrylate (PMMA) bone cement is mixed.
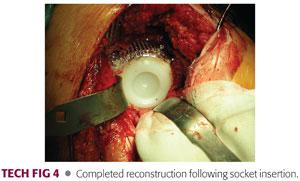
The PMMA cement is inserted into the acetabulum once it has reached the correct consistency and is pressurized for a minute prior to cup insertion.
The authors prefer a flanged all-polyethylene acetabular component.
Following insertion, pressure is maintained on the acetabular component until the PMMA cement has polymerized (TECH FIG 4).
PEARLS AND PITFALLS | |
Acetabular exposure |
|
Acetabular preparation |
|
| |
| |
Bone graft preparation |
|
| |
| |
| |
Acetabular bone reconstruction |
|
| |
| |
| |
Cemented cup insertion |
|
POSTOPERATIVE CARE
 Postoperative protocols are according to the surgeon’s preference. Perioperative antibiotics are recommended.
Postoperative protocols are according to the surgeon’s preference. Perioperative antibiotics are recommended.
 Prophylaxis for heterotopic ossification should be considered.
Prophylaxis for heterotopic ossification should be considered.
 Patients are toe-touch weight bearing for 6 weeks, followed by partial weight bearing with crutches or a walker for another 6 weeks.
Patients are toe-touch weight bearing for 6 weeks, followed by partial weight bearing with crutches or a walker for another 6 weeks.
 Interval-appropriate radiographs are recommended.
Interval-appropriate radiographs are recommended.
OUTCOMES
 Schreurs et al12 reported on 62 consecutive acetabular revisions in 58 patients with acetabular impaction bone grafting and a cemented cup at an average follow-up of 16.5 years and found an overall survival rate of 79% and an 84% survival rate when aseptic loosening was used as an end point.
Schreurs et al12 reported on 62 consecutive acetabular revisions in 58 patients with acetabular impaction bone grafting and a cemented cup at an average follow-up of 16.5 years and found an overall survival rate of 79% and an 84% survival rate when aseptic loosening was used as an end point.
 Schreurs et al13 reported a 20-year survival rate of 91% with aseptic loosening as an end point in patients younger than 50 years of age. The overall survival in this patient population was 80% when acetabular revision for any reason was evaluated.
Schreurs et al13 reported a 20-year survival rate of 91% with aseptic loosening as an end point in patients younger than 50 years of age. The overall survival in this patient population was 80% when acetabular revision for any reason was evaluated.
 Schreurs et al,15 using a similar technique in 35 hips in patients with rheumatoid arthritis, demonstrated a prosthetic survival rate of 90% at 8 years, with aseptic loosening as the end point.
Schreurs et al,15 using a similar technique in 35 hips in patients with rheumatoid arthritis, demonstrated a prosthetic survival rate of 90% at 8 years, with aseptic loosening as the end point.
 Pitto et al8 reported on 81 patients treated with impaction bone grafting and reinforcement rings. At an average of 6.5 years, only one patient had a revision because of dislocation. All grafts demonstrated graft incorporation at 3 months.
Pitto et al8 reported on 81 patients treated with impaction bone grafting and reinforcement rings. At an average of 6.5 years, only one patient had a revision because of dislocation. All grafts demonstrated graft incorporation at 3 months.
 Gilbody et al5 reported on a minimum 10-year follow-up of 304 hips revised using AIG. The mean follow-up was 12.4 years and the survival rate with revision for aseptic loosening as the end point was 85.9%.
Gilbody et al5 reported on a minimum 10-year follow-up of 304 hips revised using AIG. The mean follow-up was 12.4 years and the survival rate with revision for aseptic loosening as the end point was 85.9%.
COMPLICATIONS
 Complications generally related to revision hip arthroplasty, such as infection, instability, hematoma, and neurovascular injury are risks of surgery.
Complications generally related to revision hip arthroplasty, such as infection, instability, hematoma, and neurovascular injury are risks of surgery.
 Wide acetabular exposure puts neurovascular structures such as the superior gluteal nerve and vessels at risk.
Wide acetabular exposure puts neurovascular structures such as the superior gluteal nerve and vessels at risk.
 Intraoperative fractures may occur with vigorous packing of the bone graft. If this occurs, the fracture should be stabilized prior to completion of the impaction procedure.
Intraoperative fractures may occur with vigorous packing of the bone graft. If this occurs, the fracture should be stabilized prior to completion of the impaction procedure.
 Socket migration can occur, but radiostereometric analysis (RSA) studies have shown that this reduces in the first postoperative year.7 The mechanism of failure in large defects is usually shear within the graft substrate; shear is less likely to occur if large bone chips are used. Significant migration in defects reconstructed using large rim meshes may result in fatigue failure of the mesh.
Socket migration can occur, but radiostereometric analysis (RSA) studies have shown that this reduces in the first postoperative year.7 The mechanism of failure in large defects is usually shear within the graft substrate; shear is less likely to occur if large bone chips are used. Significant migration in defects reconstructed using large rim meshes may result in fatigue failure of the mesh.
ACKNOWLEDGMENT
All images reproduced with the kind permission of The Exeter Hip Unit publishers.
REFERENCES
1. Arts JJ, Verdonschot N, Buma P, et al. Larger bone graft size and washing of bone grafts prior to impaction enhances the initial stability of cemented cups: experiments using a synthetic acetabular model. Acta Orthop 2006;77:227–233.
2. Bolder SB, Schreurs BW, Verdonschot N, et al. Particle size of bone graft and method of impaction affect initial stability of cemented cups: human cadaveric and synthetic pelvic specimen studies. Acta Orthop Scand 2003;74:652–657.
3. Duncan WW, Hubble MJ, Howell JR, et al. Revision of the cemented femoral stem using a cement-in-cement technique. J Bone Joint Surg Br 2009;91(5):577–582.
4. Dunlop DG, Brewster NT, Madabhushi SP, et al. Techniques to improve the shear strength of impacted bone graft: the effect of particle size and washing of the graft. J Bone Joint Surg Am 2003;85A:639–646.
5. Gilbody J, Taylor C, Bartlett GE, et al. Clinical and radiographic outcomes of acetabular impaction grafting without cage reinforcement for revision hip arthroplasty: a minimum 10 year follow-up study. Bone Joint J 2014;96-B(2):188–194.
6. Gill K, Wilson MJ, Whitehouse SL, et al. Results using Trabecular Metal™ augments in combination with acetabular impaction bone grafting in deficient acetabular. Hip Int 2013;23(6):522–528.
7. Ornstein E, Franzen H, Johnsson R, et al. Five-year follow-up of socket movements and loosening after revision with impacted morselized allograft bone and cement: a radiostereometric and radiographic analysis. J Arthroplasty 2006;21(7):975–984.
8. Pitto RP, Di Muria GV, Hohmann D. Impaction grafting and acetabular reinforcement in revision hip replacement. Int Orthop 1998;22:161–164.
9. Roffman M, Silbermann M, Mendes DG. Viability and osteogenicity of bone graft coated with methylmethacrylate cement. Acta Orthop Scand 1982;53:513–519.
10. Rudelli S, Uip D, Honda E, et al. One-stage revision of infected total hip arthroplasty with bone graft. J Arthroplasty 2008;23(8):1165–1177.
11. Schimmel JW, Buma P, Versleyen D, et al. Acetabular reconstruction with impacted morselized cancellous allografts in cemented hip arthroplasty: a histological and biomechanical study on the goat. J Arthroplasty 1998;13:438–448.
12. Schreurs BW, Bolder SB, Gardeniers JW, et al. Acetabular revision with impacted morsellised cancellous bone grafting and a cemented cup: a 15- to 20-year follow-up. J Bone Joint Surg Br 2004;86B:492–497.
13. Schreurs BW, Busch VJ, Welten ML, et al. Acetabular reconstruction with impaction bone-grafting and a cemented cup in patients younger than fifty years old. J Bone Joint Surg Am 2004;86A:2385–2392.
14. Schreurs BW, Slooff TJ, Buma P, et al. Acetabular reconstruction with impacted morsellised cancellous bone graft and cement: a 10- to 15-year follow-up of 60 revision arthroplasties. J Bone Joint Surg Br 1998;80B:391–395.
15. Schreurs BW, Thien TM, de Waal Malefijt MC, et al. Acetabular revision with impacted morselized cancellous bone graft and a cemented cup in patients with rheumatoid arthritis: three to fourteen-year follow-up. J Bone Joint Surg Am 2003;85A:647–652.
16. van der Donk S, Buma P, Slooff TJ, et al. Incorporation of morselized bone grafts: a study of 24 acetabular biopsy specimens. Clin Orthop Rel Res 2002:131–141.
17. Walde TA, Weiland DE, Leung SB, et al. Comparison of CT, MRI, and radiographs in assessing pelvic osteolysis: a cadaveric study. Clin Orthop Relat Res 2005;(437):138–144.
18. Wilson MJ, Whitehouse SL, Howell JR, et al. The results of acetabular impaction grafting in 129 cemented total hip replacements. J Arthroplasty 2013;28(8):1394–1400.
< div class='tao-gold-member'>
















