The hip is increasingly recognized as a source of pain owing to heightened awareness of pathologies, recent research, enhanced imaging techniques, and greater popularity of hip arthroscopy as a diagnostic and therapeutic tool.
 Hip arthroscopy first was performed on a cadaver in the 1930s by Burman, but it was not performed regularly until the 1980s, serving mostly as a tool for diagnosis and simple treatments, such as loose body removal, synovial biopsy, and partial labrectomy.
Hip arthroscopy first was performed on a cadaver in the 1930s by Burman, but it was not performed regularly until the 1980s, serving mostly as a tool for diagnosis and simple treatments, such as loose body removal, synovial biopsy, and partial labrectomy.
 With improvements in instrumentation, indications for hip arthroscopy have expanded because surgeons now are able to do more in the hip with decreased risk of iatrogenic injury. Furthermore, enhanced imaging techniques have allowed noninvasive diagnosis, and research has led to increased understanding of hip pathologies, furthering interest in this procedure.
With improvements in instrumentation, indications for hip arthroscopy have expanded because surgeons now are able to do more in the hip with decreased risk of iatrogenic injury. Furthermore, enhanced imaging techniques have allowed noninvasive diagnosis, and research has led to increased understanding of hip pathologies, furthering interest in this procedure.
 Hip arthroscopy can be performed in the central compartment (femoroacetabular joint) and peripheral compartment (along the femoral neck), which also has expanded the indications and success of hip arthroscopy, propagating the popularity of this procedure.
Hip arthroscopy can be performed in the central compartment (femoroacetabular joint) and peripheral compartment (along the femoral neck), which also has expanded the indications and success of hip arthroscopy, propagating the popularity of this procedure.
ANATOMY
 The hip joint is a multiaxial ball-and-socket type of synovial joint in which the head of the femur (ball) articulates with the acetabulum (socket) of the hip.
The hip joint is a multiaxial ball-and-socket type of synovial joint in which the head of the femur (ball) articulates with the acetabulum (socket) of the hip.
 Articular cartilage covers the head of the femur and acetabulum but is not present at the fovea or cotyloid fossa.
Articular cartilage covers the head of the femur and acetabulum but is not present at the fovea or cotyloid fossa.
The articular cartilage of the femoral head and acetabulum is relatively thin compared with that of the knee (FIG 1A).
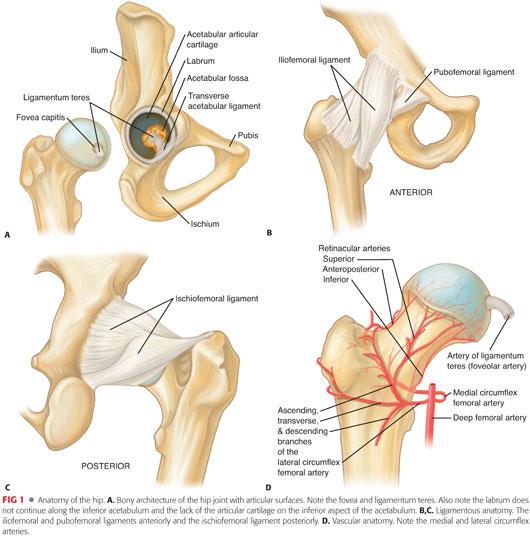
 The acetabular labrum is a triangular fibrocartilage that attaches to the rim of the acetabulum at the articular cartilage edge, except at the inferior most region of the acetabulum, where the transverse acetabular ligament extends the acetabular rim.
The acetabular labrum is a triangular fibrocartilage that attaches to the rim of the acetabulum at the articular cartilage edge, except at the inferior most region of the acetabulum, where the transverse acetabular ligament extends the acetabular rim.
 The hip joint is enclosed by a capsule that is formed by an external fibrous layer and internal synovial membrane and attaches directly to the bony acetabular rim.
The hip joint is enclosed by a capsule that is formed by an external fibrous layer and internal synovial membrane and attaches directly to the bony acetabular rim.
 The fibrous layer consists of the iliofemoral, pubofemoral, and ischiofemoral ligaments, which anchor the head of the femur into the acetabulum (FIG 1B,C).
The fibrous layer consists of the iliofemoral, pubofemoral, and ischiofemoral ligaments, which anchor the head of the femur into the acetabulum (FIG 1B,C).
 The ligamentum teres is extracapsular and travels from the central acetabulum to the foveal portion of the femoral head (FIG 1A).
The ligamentum teres is extracapsular and travels from the central acetabulum to the foveal portion of the femoral head (FIG 1A).
 The major arteries supplying the hip joint include the medial and lateral circumflex femoral arteries, which branch to provide the retinacular arteries that supply the head and neck of the femur (FIG 1D).
The major arteries supplying the hip joint include the medial and lateral circumflex femoral arteries, which branch to provide the retinacular arteries that supply the head and neck of the femur (FIG 1D).
 The artery to the head of the femur also supplies blood and transverses the ligament of the head of the femur (ie, the ligamentum teres).
The artery to the head of the femur also supplies blood and transverses the ligament of the head of the femur (ie, the ligamentum teres).
 The labrum has a relatively low healing potential because vessels penetrate only the outermost layer of the capsular surface.
The labrum has a relatively low healing potential because vessels penetrate only the outermost layer of the capsular surface.
 Pertinent extra-articular neurovascular structures near the hip joint include the lateral femoral cutaneous nerve, femoral nerve, superior gluteal nerve, sciatic nerve, and the ascending branch of the lateral circumflex femoral artery.
Pertinent extra-articular neurovascular structures near the hip joint include the lateral femoral cutaneous nerve, femoral nerve, superior gluteal nerve, sciatic nerve, and the ascending branch of the lateral circumflex femoral artery.
 The lateral femoral cutaneous nerve, formed from the posterior divisions of L2 and L3 nerve roots, supplies the skin sensation of the lateral thigh. It travels from the pelvis just distal and medial to the anterior superior iliac spine (ASIS) and divides into more than three branches distal to the ASIS.
The lateral femoral cutaneous nerve, formed from the posterior divisions of L2 and L3 nerve roots, supplies the skin sensation of the lateral thigh. It travels from the pelvis just distal and medial to the anterior superior iliac spine (ASIS) and divides into more than three branches distal to the ASIS.
 The femoral nerve and artery run together with the femoral vein. They pass under the inguinal ligament midway between the ASIS and the pubic symphysis, with the nerve being most lateral and the vein most medial but being mostly superficial at the level of the hip.
The femoral nerve and artery run together with the femoral vein. They pass under the inguinal ligament midway between the ASIS and the pubic symphysis, with the nerve being most lateral and the vein most medial but being mostly superficial at the level of the hip.
The femoral nerve is 3.2 cm from the anterior hip portal but slightly closer at the level of the capsule.
 The superior gluteal nerve, formed from the posterior divisions of L4, L5, and S1, passes posterior and lateral to the obturator internus and piriformis muscles, then between the gluteus medius and minimus muscles approximately 4 cm proximal to the hip joint.
The superior gluteal nerve, formed from the posterior divisions of L4, L5, and S1, passes posterior and lateral to the obturator internus and piriformis muscles, then between the gluteus medius and minimus muscles approximately 4 cm proximal to the hip joint.
 The sciatic nerve, formed when nerves from L4 to S3 come together, passes anterior and inferior to the piriformis and posterior to the deep hip external rotators to supply the hamstrings and lower leg, foot, and ankle.
The sciatic nerve, formed when nerves from L4 to S3 come together, passes anterior and inferior to the piriformis and posterior to the deep hip external rotators to supply the hamstrings and lower leg, foot, and ankle.
The sciatic nerve is 2.9 cm from the posterior hip arthroscopy portal but is closest at the level of the capsule.
Internally rotating or flexing the hip prior to making the posterior portal brings the nerve dangerously close to the arthroscope.
 The lateral femoral circumflex artery is a branch of the femoral artery that, along with the medial circumflex artery, forms a vascular ring about the neck of the femur, providing arteriole branches to supply the femoral head (FIG 1D).
The lateral femoral circumflex artery is a branch of the femoral artery that, along with the medial circumflex artery, forms a vascular ring about the neck of the femur, providing arteriole branches to supply the femoral head (FIG 1D).
 The lateral femoral circumflex artery is 3.7 cm inferior to the anterior arthroscopy portal; it is much closer at the level of the capsular entry of the arthroscope.
The lateral femoral circumflex artery is 3.7 cm inferior to the anterior arthroscopy portal; it is much closer at the level of the capsular entry of the arthroscope.
PATHOGENESIS
 Loose bodies can be ossified or nonossified and can either appear after traumatic hip injury or be associated with conditions such as osteochondritis dissecans and synovial chondromatosis.8
Loose bodies can be ossified or nonossified and can either appear after traumatic hip injury or be associated with conditions such as osteochondritis dissecans and synovial chondromatosis.8
 Labral tear often results from hyperextension or external rotation of the hip and is more likely with hip dysplasia.
Labral tear often results from hyperextension or external rotation of the hip and is more likely with hip dysplasia.
 Chondral (articular cartilage) damage can result from dislocation or subluxation of the hip or direct impact onto the hip and is associated with labral tears in more than half the cases.9
Chondral (articular cartilage) damage can result from dislocation or subluxation of the hip or direct impact onto the hip and is associated with labral tears in more than half the cases.9
 Femoroacetabular impingement is a major cause of labral tears and chondral damage.
Femoroacetabular impingement is a major cause of labral tears and chondral damage.
It usually occurs when there is loss of femoral head–neck offset (cam impingement), excessive acetabular coverage (eg, osteophytes, retroversion, overcorrection with pelvic osteotomy, protrusio acetabuli, or otto pelvis) (pincer impingement), or both.
The femoral head–neck junction abuts the acetabulum and labrum, resulting in tearing of the labrum, delamination of the articular cartilage, synovitis, and, eventually, arthritis.
 Ligamentum teres pathology may be due to ligament hypertrophy or partial or complete tearing and may be the result of trauma or degenerative joint disease (DJD).
Ligamentum teres pathology may be due to ligament hypertrophy or partial or complete tearing and may be the result of trauma or degenerative joint disease (DJD).
Ligamentum hypertrophy or tearing may result in pain as a result of catching of a thickened or torn edge between the joint surfaces.
 DJD may be associated with loose bodies, labrum tears, chondral damage, ligamentum teres pathology, and synovitis.
DJD may be associated with loose bodies, labrum tears, chondral damage, ligamentum teres pathology, and synovitis.
 Avascular necrosis of the femoral head is primarily idiopathic but can be associated with corticosteroid use, alcohol consumption, fracture, and deep sea diving (caisson disease), among others.
Avascular necrosis of the femoral head is primarily idiopathic but can be associated with corticosteroid use, alcohol consumption, fracture, and deep sea diving (caisson disease), among others.
 Synovial diseases such as pigmented villonodular synovitis, synovial chondromatosis, inflammatory arthritis, and osteochondromatosis can be sources of hip pain and joint damage.
Synovial diseases such as pigmented villonodular synovitis, synovial chondromatosis, inflammatory arthritis, and osteochondromatosis can be sources of hip pain and joint damage.
 Hip instability, either traumatic or atraumatic, may be a cause of labral tears and chondral damage.
Hip instability, either traumatic or atraumatic, may be a cause of labral tears and chondral damage.
Hip instability may be traumatic (eg, acetabular posterior wall fractures) or atraumatic (eg, developmental dysplasia of the hip, connective tissue disorders, benign hypermobility) or as a result of microtrauma (repetitive external rotation).
Pathology exists as a spectrum from hip dislocation to subluxation to microinstability.
NATURAL HISTORY
 The natural history of most pathologies about the hip has not been studied; much of the purported natural history is therefore conjecture.
The natural history of most pathologies about the hip has not been studied; much of the purported natural history is therefore conjecture.
 Removal of loose bodies alleviates mechanical symptoms and reduces articular cartilage damage.
Removal of loose bodies alleviates mechanical symptoms and reduces articular cartilage damage.
 Labral tears and chondral lesions that are débrided may result in degenerative arthritis.
Labral tears and chondral lesions that are débrided may result in degenerative arthritis.
 Untreated femoroacetabular impingement may result in degenerative arthritis.
Untreated femoroacetabular impingement may result in degenerative arthritis.
 It has been proposed, but not proved, that labral repair or surgery for femoroacetabular impingement may lower the risk of developing DJD or slow the rate of degeneration.
It has been proposed, but not proved, that labral repair or surgery for femoroacetabular impingement may lower the risk of developing DJD or slow the rate of degeneration.
PATIENT HISTORY AND PHYSICAL FINDINGS
 The patient history should include an investigation of the quality and location of pain, timing and precipitating cause of symptoms, and any referred pain.
The patient history should include an investigation of the quality and location of pain, timing and precipitating cause of symptoms, and any referred pain.
 Patients with intra-articular pathology may have difficulty with torsional or twisting activities, discomfort with prolonged hip flexion (eg, sitting), pain or catching from flexion to extension (eg, rising from a seated position), and greater difficulty on inclines than on level surfaces.2
Patients with intra-articular pathology may have difficulty with torsional or twisting activities, discomfort with prolonged hip flexion (eg, sitting), pain or catching from flexion to extension (eg, rising from a seated position), and greater difficulty on inclines than on level surfaces.2
 Intra-articular pathology may be associated with groin pain extending to the knee and mechanical symptoms such as popping, locking, or restricted range of motion (ROM).3
Intra-articular pathology may be associated with groin pain extending to the knee and mechanical symptoms such as popping, locking, or restricted range of motion (ROM).3
The source of intra-articular pathology should be investigated in patients with continuous hip pain for longer than 4 weeks.
 Physical examination methods are summarized later.
Physical examination methods are summarized later.
It is important to follow a systemic approach to examination that includes inspection, palpation, ROM, strength, and special tests.11
 Intra-articular pathologies do not have palpable areas of tenderness, although compensation for long-standing intra-articular problems may result in tenderness of muscles or bursae.
Intra-articular pathologies do not have palpable areas of tenderness, although compensation for long-standing intra-articular problems may result in tenderness of muscles or bursae.
 Motor strength and neurovascular examinations must be performed for the entire lower extremity.
Motor strength and neurovascular examinations must be performed for the entire lower extremity.
 It is important to rule out other causes of pain referred to the hip.
It is important to rule out other causes of pain referred to the hip.
Spinal pain usually is localized at the posterior buttock and sacroiliac region and may radiate to the lower extremity.
Injuries to the sacrum and sacroiliac joint are recognized by a positive gapping or transverse anterior stress test.
Abdominal injuries are recognized by basic inspection and palpation of the abdomen for a mass or fascial hernia, which can be evaluated by isometric contraction of the rectus abdominis and obliques.
Abdominal muscle injury is recognized by pain during contraction of the rectus abdominis and obliques.
Herniography may be used to rule out hernias.
• Particularly difficult to diagnose is the sports hernia (Gilmore groin), which is not a true hernia.
Genitourinary tract
• Injuries to the pelvic area, such as pubic symphysis and intrapelvic problems, are recognized by the gapping/transverse anterior stress test.
 Specific tests for the hip include the following:
Specific tests for the hip include the following:
McCarthy test: distinction of internal hip pathology such as torn acetabular labrum or lateral rim impingement
Stinchfield and Fulcrum test: diagnosis of internal derangements, primarily of the anterior portion of the acetabulum
Scour test: associated with microinstability or combined anterior anteversion, acetabular anteversion summation, hyperlaxity, or strain of the iliofemoral ligament
Thomas test: tests for flexion contracture. Extension to 0 degrees (in line with the body) without low back motion is normal. Less than full extension without rotating the pelvis or lifting the lower back is consistent with a flexion contracture.
Ober test: used to evaluate iliotibial band tightness. The test is positive when the upper knee remains in the abducted position after the hip is passively extended and abducted, then adducted, with the knee flexed. If, when the hip and knee are allowed to adduct while the hip is held in neutral rotation, the knee adducts past midline, the hip abductors are not tight; whereas if the knee does not reach to midline, then the hip abductors are tight.
Ely test: if on flexion of the knee the ipsilateral hip also flexes, then the rectus femoris is tight.
Trendelenburg test: indicative of hip abductor weakness and may indicate labrum pathology that affects neuroproprioceptive function. If the pelvis (iliac crest or posterior superior iliac spine) of the ipsilateral hip of the leg that is lifted elevates from the neutral standing position, this is normal. If the pelvis drops below the contralateral pelvis or from the starting position (ie, iliac crest/posterior superior iliac spine), this is considered a positive Trendelenburg sign and indicative of hip abductor weakness of the muscles on the extremity standing on the ground. If the pelvis stays level, then this is indicative of mild weakness and recorded as level.
Patrick test (FABER test): indicative of sacroiliac abnormalities or iliopsoas spasm. Pain may be felt with downward stress on the flexed knee. Pain in the posterior pelvis may be considered a positive finding that indicates the pain is coming from the sacroiliac joint.
Labral stress test: indicative of labral tear. The patient will note groin pain or a click in a consistent position as the hip is being rotated.
Piriformis test: Pain in the lateral hip or buttock reproduced by this maneuver is consistent with pain from the piriformis.
Impingement test: Pain in the groin is a positive test and is consistent with intra-articular hip pain, not just femoroacetabular impingement.
Hip extension and external rotation test: indicative of hip microinstability. The patient will note discomfort or apprehension in the anterior aspect of the hip.
IMAGING AND OTHER DIAGNOSTIC STUDIES
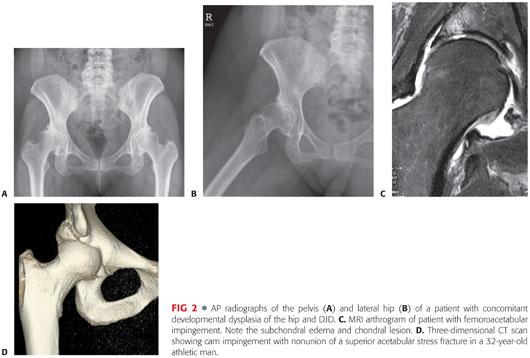
 Routine anteroposterior (AP) and lateral (usually cross-table lateral or Dunn view) radiographs should be obtained in all patients with hip pain to evaluate variations in bony architecture and visualization of areas that may present with hip pain such as the pubic symphysis, sacrum, sacroiliac joints, ilium, and ischium.
Routine anteroposterior (AP) and lateral (usually cross-table lateral or Dunn view) radiographs should be obtained in all patients with hip pain to evaluate variations in bony architecture and visualization of areas that may present with hip pain such as the pubic symphysis, sacrum, sacroiliac joints, ilium, and ischium.
Radiographs help exclude degenerative joint changes, osteonecrosis, loose bodies, stress fractures, or other osseous pathology, and help assess for acetabular dysplasia and femoral neck abnormalities (bump or cam lesion) and femoroacetabular impingement (FIG 2A,B).
 Bone scan or radionuclide imaging is sensitive in detecting fractures, arthritis, neoplasm, infections, and vascular abnormalities but has low specificity and poor anatomic resolution.
Bone scan or radionuclide imaging is sensitive in detecting fractures, arthritis, neoplasm, infections, and vascular abnormalities but has low specificity and poor anatomic resolution.
 Magnetic resonance imaging (MRI) is used to detect stress fractures of the femoral neck and to identify sources of hip pain such as osteonecrosis, pigmented villonodular synovitis, synovial chondromatosis, osteochondromas, and other intra-articular pathology.
Magnetic resonance imaging (MRI) is used to detect stress fractures of the femoral neck and to identify sources of hip pain such as osteonecrosis, pigmented villonodular synovitis, synovial chondromatosis, osteochondromas, and other intra-articular pathology.
MRI arthrography can increase the ability to diagnose and describe labral pathology and articular cartilage loss (FIG 2C).
MRI combined with the use of intra-articular local anesthetic with gadolinium is used to assess pain relief and provide evidence that intra-articular pathology may be causing pain.
Recent studies have demonstrated a very high prevalence of asymptomatic labral tears in young, active people.
 Computed tomography (CT), MRI, and occasionally radioisotope imaging typically are required to help diagnose labral tears, hip instability, iliopsoas tendinitis, inflammatory arthritis, early avascular necrosis, occult fractures, psoas abscess, tumor, upper lumbar radiculopathy, or vascular abnormalities.
Computed tomography (CT), MRI, and occasionally radioisotope imaging typically are required to help diagnose labral tears, hip instability, iliopsoas tendinitis, inflammatory arthritis, early avascular necrosis, occult fractures, psoas abscess, tumor, upper lumbar radiculopathy, or vascular abnormalities.
CT scan can be useful to measure ante- and retroversion of the femoral neck and acetabulum, to show the size and shape of the acetabulum and femoral head and neck, to elucidate bony architecture, to confirm concentric reduction after hip dislocation, and to rule out loose bodies.
CT scan has also been shown to be helpful in assessing the morphology of the AIIS (anterior inferior iliac spine), which has been implicated in subspinous impingement.
 Ultrasound is a nonirradiating way of evaluating intra-articular effusions and soft tissue swelling.
Ultrasound is a nonirradiating way of evaluating intra-articular effusions and soft tissue swelling.
 Iliopsoas bursography is the choice imaging modality to detect iliopsoas bursitis and internal snapping hip.
Iliopsoas bursography is the choice imaging modality to detect iliopsoas bursitis and internal snapping hip.
Iliopsoas bursitis and internal snapping hip may be evaluated with real-time dynamic ultrasound.
Three-dimensional CT is used to assess bony deformities, including osteophytes of the acetabulum and femoral neck bony lesions, which may cause impingement (FIG 2D).
DIFFERENTIAL DIAGNOSIS
 Labral tear
Labral tear
 Chondral delamination or degeneration
Chondral delamination or degeneration
 Dysplasia
Dysplasia
 Femoroacetabular impingement
Femoroacetabular impingement
 Synovitis
Synovitis
 Synovial chondromatosis
Synovial chondromatosis
 Synovial osteochondromatosis
Synovial osteochondromatosis
 Loose bodies
Loose bodies
 Ligamentum teres tear
Ligamentum teres tear
 Ligamentum teres hypertrophy
Ligamentum teres hypertrophy
 Sepsis of the hip
Sepsis of the hip
 Arthritis of the hip
Arthritis of the hip
 Hip dislocation, subluxation, or microinstability
Hip dislocation, subluxation, or microinstability
 Subspinous impingement (AIIS impingement)
Subspinous impingement (AIIS impingement)
 Avascular necrosis of the femoral head
Avascular necrosis of the femoral head
 Sacroiliac joint pathology, including ankylosing spondylitis
Sacroiliac joint pathology, including ankylosing spondylitis
 Trochanteric bursitis
Trochanteric bursitis
 Athletic pubalgia
Athletic pubalgia
 Femur, pelvic, or acetabular fractures or stress fractures
Femur, pelvic, or acetabular fractures or stress fractures
 Myotendinous strains
Myotendinous strains
 Piriformis syndrome
Piriformis syndrome
 Myositis ossification
Myositis ossification
 Neurologic irritation
Neurologic irritation
 Hamstring syndrome
Hamstring syndrome
 Iliotibial band syndrome
Iliotibial band syndrome
 Iliopsoas tendon problems (eg, snapping and tendinitis)
Iliopsoas tendon problems (eg, snapping and tendinitis)
 Tendinitis
Tendinitis
 Tendon injuries (iliopsoas, piriformis, rectus, hamstring, or adductor)
Tendon injuries (iliopsoas, piriformis, rectus, hamstring, or adductor)
 Benign tumors (eg, osteoid osteoma, osteochondroma)
Benign tumors (eg, osteoid osteoma, osteochondroma)
 Occult hernia
Occult hernia
 Lumbar spine (mechanical pain and herniated discs)
Lumbar spine (mechanical pain and herniated discs)
 Abdomen
Abdomen
 Osteitis pubis
Osteitis pubis
NONOPERATIVE MANAGEMENT
 Conservative therapy includes rest, ambulatory support, nonsteroidal anti-inflammatory drugs, and physical therapy.
Conservative therapy includes rest, ambulatory support, nonsteroidal anti-inflammatory drugs, and physical therapy.
 Most pathologies about the hip usually are treated initially with conservative management, including relative rest, nonsteroidal anti-inflammatory drugs, and rehabilitation. Occasionally, protected weight bearing and use of ambulatory assist devices may be needed.
Most pathologies about the hip usually are treated initially with conservative management, including relative rest, nonsteroidal anti-inflammatory drugs, and rehabilitation. Occasionally, protected weight bearing and use of ambulatory assist devices may be needed.
 However, several intra-articular pathologies do not resolve or heal with nonoperative management, including labral tears, loose bodies, articular cartilage lesions, and femoroacetabular impingement.
However, several intra-articular pathologies do not resolve or heal with nonoperative management, including labral tears, loose bodies, articular cartilage lesions, and femoroacetabular impingement.
SURGICAL MANAGEMENT
 Proper patient selection is essential for a successful surgical outcome.
Proper patient selection is essential for a successful surgical outcome.
 Arthroscopy is most successful for patients with recent, symptomatic intra-articular hip joint pathology, particularly those with mechanical symptoms, and minimal arthritic changes.
Arthroscopy is most successful for patients with recent, symptomatic intra-articular hip joint pathology, particularly those with mechanical symptoms, and minimal arthritic changes.
 Arthroscopy should be considered if hip pain is persistent, is reproducible on physical examination, and does not respond to conservative treatment.
Arthroscopy should be considered if hip pain is persistent, is reproducible on physical examination, and does not respond to conservative treatment.
 Pain relief with intra-articular injection of local anesthetic also is a good predictive sign for success.
Pain relief with intra-articular injection of local anesthetic also is a good predictive sign for success.
 Indications for arthroscopy include loose bodies, foreign objects, labral tears, chondral injuries, synovial disease, femoroacetabular impingement, mild degenerative disease with mechanical symptoms, osteonecrosis of femoral head, osteochondritis dissecans, ruptured ligamentum teres, snapping hip syndrome, impinging osteophytes, adhesive capsulitis, iliopsoas tendon release, iliopsoas bursitis, trochanteric bursectomy, iliotibial band resection, crystalline hip arthropathy, hip instability, subspinous impingement, joint sepsis, osteoid osteoma, osteochondroma, and unresolved hip pain.
Indications for arthroscopy include loose bodies, foreign objects, labral tears, chondral injuries, synovial disease, femoroacetabular impingement, mild degenerative disease with mechanical symptoms, osteonecrosis of femoral head, osteochondritis dissecans, ruptured ligamentum teres, snapping hip syndrome, impinging osteophytes, adhesive capsulitis, iliopsoas tendon release, iliopsoas bursitis, trochanteric bursectomy, iliotibial band resection, crystalline hip arthropathy, hip instability, subspinous impingement, joint sepsis, osteoid osteoma, osteochondroma, and unresolved hip pain.
 ROM should be evaluated before arthroscopy to determine the presence of contractures.
ROM should be evaluated before arthroscopy to determine the presence of contractures.
 Arthroscopy can be a means to delay total arthroplasty for DJD.
Arthroscopy can be a means to delay total arthroplasty for DJD.
 Contraindications include systemic illness, open wounds, soft tissue disorders, poor bone quality (ie, unable to withstand traction), nonprogressing avascular necrosis of the femoral head, arthrofibrosis or capsular constriction, and ankylosis of the hip.
Contraindications include systemic illness, open wounds, soft tissue disorders, poor bone quality (ie, unable to withstand traction), nonprogressing avascular necrosis of the femoral head, arthrofibrosis or capsular constriction, and ankylosis of the hip.
 Severe obesity is a relative contraindication that may be circumvented with extra-length instruments.
Severe obesity is a relative contraindication that may be circumvented with extra-length instruments.
 Indications for labrectomy include relief of pain with intra-articular injection of anesthesia, no pain relief with physical therapy or nonsteroidal anti-inflammatory drugs, missed time due to delayed diagnosis, and symptoms for longer than 4 weeks.
Indications for labrectomy include relief of pain with intra-articular injection of anesthesia, no pain relief with physical therapy or nonsteroidal anti-inflammatory drugs, missed time due to delayed diagnosis, and symptoms for longer than 4 weeks.
 Arthroscopy for DJD should be considered for younger patients with mild–moderate disease who present with mechanical symptoms and no deformity.
Arthroscopy for DJD should be considered for younger patients with mild–moderate disease who present with mechanical symptoms and no deformity.
 Microfracture is indicated for grade IV chondral lesions with healthy surrounding articular surface and intact subchondral bone.
Microfracture is indicated for grade IV chondral lesions with healthy surrounding articular surface and intact subchondral bone.
 Treatment of sepsis involves drainage, lavage, débridement, and postoperative antibiotics, and requires early diagnosis.
Treatment of sepsis involves drainage, lavage, débridement, and postoperative antibiotics, and requires early diagnosis.
Sepsis in the setting of joint arthroplasty requires prompt arthroscopic débridement, well-fixed components, a sensitive microorganism, and patient tolerance to and compliance with antibiotic therapy.7
Preoperative Planning
 A physical examination should be completed and radiographs and other imaging reviewed before arthroscopy.
A physical examination should be completed and radiographs and other imaging reviewed before arthroscopy.
 A three-dimensional CT scan may be obtained to further assess bony abnormalities (see FIG 2D).
A three-dimensional CT scan may be obtained to further assess bony abnormalities (see FIG 2D).
 Arthroscopy usually is performed under general anesthesia.
Arthroscopy usually is performed under general anesthesia.
 If epidural anesthesia is used, it also requires adequate motor block to relax muscle tone.
If epidural anesthesia is used, it also requires adequate motor block to relax muscle tone.
 Typical instrumentation includes a marking pen; no. 11 blade scalpel; 6-inch 17-gauge spinal needles; 60-mL syringe of saline with extension tubing; a Nitinol guidewire; 4.5-, 5.0-, and 5.5-mm cannulas with cannulated and solid obturators; a switching stick; a separate inflow adaptor; and a modified probe.
Typical instrumentation includes a marking pen; no. 11 blade scalpel; 6-inch 17-gauge spinal needles; 60-mL syringe of saline with extension tubing; a Nitinol guidewire; 4.5-, 5.0-, and 5.5-mm cannulas with cannulated and solid obturators; a switching stick; a separate inflow adaptor; and a modified probe.
 Fluid used can be introduced by gravity or a pump.
Fluid used can be introduced by gravity or a pump.
 Specialized arthroscopy equipment for the hip is available that is extra-long and extra-strong to withstand the lever arm due to the extra length. These instruments include shavers, burrs, biters, probes, curettes, and loose body retrievers.
Specialized arthroscopy equipment for the hip is available that is extra-long and extra-strong to withstand the lever arm due to the extra length. These instruments include shavers, burrs, biters, probes, curettes, and loose body retrievers.
Positioning
 The patient may be placed in either the supine or lateral decubitus position on a fracture table or attachment that allows for distraction of the hip joint.
The patient may be placed in either the supine or lateral decubitus position on a fracture table or attachment that allows for distraction of the hip joint.
The lateral decubitus position offers the benefit of directing fat away from the operative site.
 The involved hip joint is in neutral rotation, abducted at 10 to 25 degrees, and in neutral flexion–extension (FIG 3A).
The involved hip joint is in neutral rotation, abducted at 10 to 25 degrees, and in neutral flexion–extension (FIG 3A).
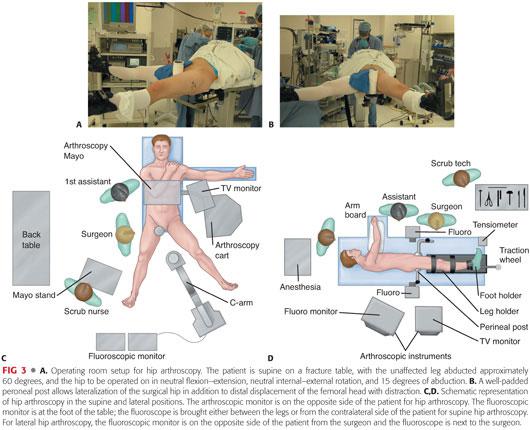
 Flexion of the involved hip during distraction and portal placement increases the risk of injury to the sciatic nerve.
Flexion of the involved hip during distraction and portal placement increases the risk of injury to the sciatic nerve.
 The nonoperative hip also is abducted and is placed under slight traction to stabilize the patient and allow placement of the image intensifier between the legs and directed over the operative hip.
The nonoperative hip also is abducted and is placed under slight traction to stabilize the patient and allow placement of the image intensifier between the legs and directed over the operative hip.
 A heavily padded perineal post is placed against the pubic ramus and ischial tuberosity, but lateralized against the medial thigh of the operative hip, with care taken to protect perineal structures (FIG 3B).
A heavily padded perineal post is placed against the pubic ramus and ischial tuberosity, but lateralized against the medial thigh of the operative hip, with care taken to protect perineal structures (FIG 3B).
 It is important to lateralize the traction vector such that it is parallel to the femoral neck to minimize risk of pressure neurapraxia to the pudendal nerve and to optimize distraction of the joint.
It is important to lateralize the traction vector such that it is parallel to the femoral neck to minimize risk of pressure neurapraxia to the pudendal nerve and to optimize distraction of the joint.
 The surgeon, assistant, and scrub nurse stand on the operative side, facing the arthroscopic monitor on the opposite side of the patient (FIG 3C,D).
The surgeon, assistant, and scrub nurse stand on the operative side, facing the arthroscopic monitor on the opposite side of the patient (FIG 3C,D).
 The fluoroscopy monitor is placed at the foot of the fracture table.
The fluoroscopy monitor is placed at the foot of the fracture table.
Approach
 Portal placement and arthroscopic technique do not differ between the supine and lateral decubitus positions.
Portal placement and arthroscopic technique do not differ between the supine and lateral decubitus positions.
 Hip arthroscopy usually is performed through three portals: anterolateral, anterior, and posterolateral.
Hip arthroscopy usually is performed through three portals: anterolateral, anterior, and posterolateral.
 A shortened bridge can accommodate the use of 4.5-, 5.0-, and 5.5-mm cannulas.
A shortened bridge can accommodate the use of 4.5-, 5.0-, and 5.5-mm cannulas.
Although a 5.0-mm cannula is used for initial entry of the arthroscope, a 4.5-mm cannula permits interchange of the inflow, arthroscope, and instruments, and a 5.5-mm cannula allows entry of larger instruments (eg, shaver blades).
 A 30-degree videoarticulated arthroscope provides best visualization of the central portion of the acetabulum, the femoral head, and the superior aspect of the acetabular fossa.
A 30-degree videoarticulated arthroscope provides best visualization of the central portion of the acetabulum, the femoral head, and the superior aspect of the acetabular fossa.
A 70-degree video arthroscope provides optimal visualization of the periphery of the joint, the acetabular labrum, and the inferior aspect of the acetabular fossa.
 The radiofrequency device are used to ablate tissue and can offer increased maneuverability over shavers.
The radiofrequency device are used to ablate tissue and can offer increased maneuverability over shavers.
 Extra-length convex and concave curved shaver blades are used to remove tissue around the femoral head.
Extra-length convex and concave curved shaver blades are used to remove tissue around the femoral head.
 Fragile, extra-length instruments designed for other arthroscopic procedures should be avoided because these have a greater tendency to break.
Fragile, extra-length instruments designed for other arthroscopic procedures should be avoided because these have a greater tendency to break.
TECHNIQUES
 Hip Distraction
Hip Distraction
The patient is prepared with chlorhexidine (Hibiclens) or povidone-iodine (Betadine).
Traction is applied to distract the joint 7 to 10 mm.
A tensiometer may be used to monitor traction force (typically 25 to 50 pounds).
Traction time should be monitored. It is important to limit the time to less than 2 hours to prevent complications such as compression of the pudendal nerve or injury to other nerves.
The spinal needle is introduced under fluoroscopy at the anterolateral position into the joint capsule to equilibrate the space with the ambient pressure (TECH FIG 1A,B).
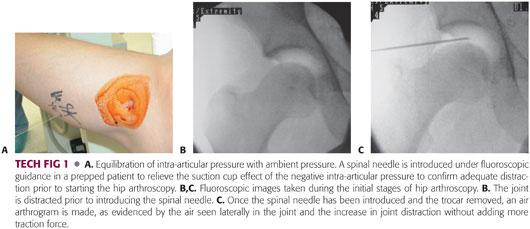
Pressure in the joint may be equilibrated with air or saline (TECH FIG 1C).
Care should be taken to avoid penetrating the labrum and articular surfaces with the spinal needle.
 Making the Portals
Making the Portals
Portals are established by penetrating the skin with a 6-inch 17-gauge spinal needle and positioning the needle into the respective joint space.
The trocar of the spinal needle is removed and a Nitinol guidewire (Smith & Nephew Endoscopy, Andover, MA) is run through the needle into the joint space (TECH FIG 2A,B).
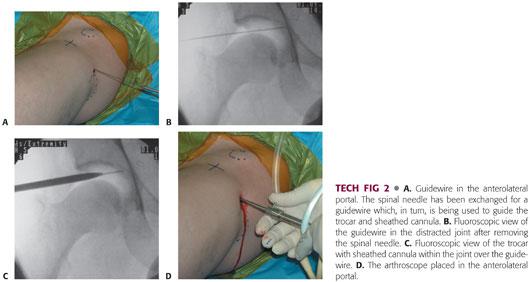
The needle is removed.
A skin incision is made at the entry site, large enough to facilitate entry of a 5.0-mm cannula.
A long cannula sheath with cannulated trocar is advanced over the guidewire into the joint space (TECH FIG 2C,D).
The cannulated obturator should be kept off the femoral head to avoid articular damage.
It is important to avoid cannula removal and reintroduction because this may damage cartilage.
It may be necessary to release the capsule with an arthroscopic knife.
The weight-bearing portion of the femoral head is visualized by using the arthroscope in all three central compartment portals with the 70- and 30-degree lenses or by internally and externally rotating the hip intraoperatively.
The fossa and ligamentum teres typically are visualized from all three portals, particularly using the 30-degree lens.
 Anterolateral Portal
Anterolateral Portal
The anterolateral portal is created first because it is the safest, being the most distant from and posing least risk of injury to the femoral and sciatic neurovascular structures.
The portal penetrates the gluteus medius muscle and is positioned directly over the superior aspect of the greater trochanter at its anterior margin to enter the lateral capsule at its anterior margin (TECH FIG 3).
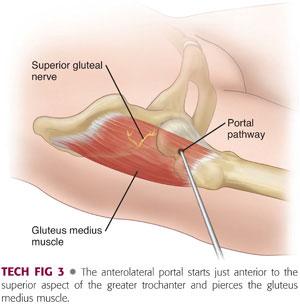
When creating the anterolateral portal, it is important to introduce the spinal needle in the coronal plane by keeping it parallel to the floor (see TECH FIG 2A).
As the cannula is positioned into the intra-articular space, care should be taken to avoid damage to the labrum or articular surfaces.
The portal provides visualization of most of the acetabular cartilage, labrum, and weight-bearing femoral head within the central compartment, as well as visualization of the peripheral compartment, such as the non–weight-bearing femoral head, the anterior neck, the anterior intrinsic capsular folds, and the synovial tissues beneath the zona orbicularis and the anterior labrum.
The superior gluteal nerve is the closest neurovascular structure and runs 4.4 cm posterior to the portal.
 Anterior Portal
Anterior Portal
The senior author prefers to establish the anterior portal after the anterolateral portal, although some prefer to establish the anterior portal first.
Arthroscopic visualization from the anterolateral portal and fluoroscopy facilitate correct portal placement, helping to avoid damage to the labrum or articular surfaces.
Several different anterior portals have been described.
One popular anterior portal enters at the junction of a line drawn distally from the ASIS and a transverse line across the superior margin of the greater trochanter (TECH FIG 4A).
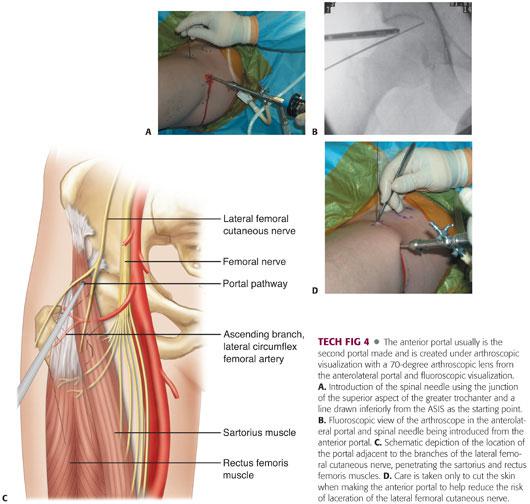
The portal penetrates the sartorius and rectus femoris muscles as it is directed 45 degrees cephalad and 30 degrees medially to enter the anterior capsule (TECH FIG 4B,C).
As the cannulated obturator enters the joint space, it should be kept off the articular surface and directed underneath the acetabular labrum.
The portal allows visualization of the anterior femoral neck, the anterior aspect of the joint, the superior retinacular fold, the ligamentum teres, and the lateral labrum.
Care should be taken to minimize injury to branches of the lateral femoral cutaneous nerve by directing movement medially, avoiding deep cuts at the entry site, not using vigorous instrumentation, and using a 70-degree arthroscope at the anterolateral portal to guide entry (TECH FIG 4D).
The femoral nerve is 3.2 cm medial and runs tangential to the portal.
The ascending branch of the lateral femoral circumflex artery is 3.7 cm inferior to the portal, but terminal branches may be within millimeters of the portal at the capsular level.
More recently, the anterior portal is made more distal (approximately 7 cm) and slightly lateral (1 to 3 cm) to the aforementioned anterior portal.
This position allows for easier access under the anterior acetabular rim in pincer impingement and provides a better approach for labral repair drilling and anchor placement.
 Posterolateral Portal
Posterolateral Portal
The posterolateral portal is established after the anterior portal (TECH FIG 5A).
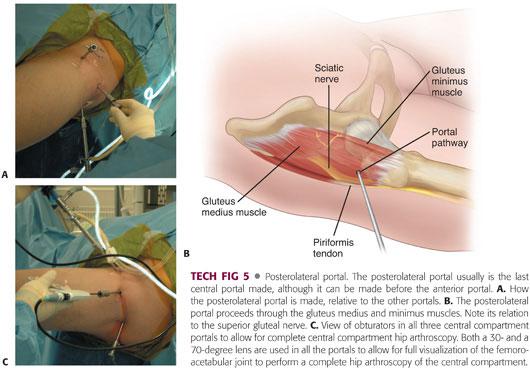
This portal is just posterior to the greater trochanter, at the same level as the anterolateral portal.
Arthroscopic visualization and fluoroscopy are used to guide portal placement.
The portal penetrates the gluteus medius and minimus muscles and is directed over the superior aspect of the greater trochanter at its posterior border to enter the lateral capsule at its posterior margin (TECH FIG 5B).
The portal is superior and anterior to the piriformis.
The portal allows visualization of the posterior aspect of the femoral head, the posterior labrum, the posterior capsule, and the inferior edge of the ischiofemoral ligament (TECH FIG 5C).
The sciatic nerve is 2.9 cm posterior to the portal at the level of the capsule.
It is important to maintain the leg in neutral rotation and extension and to introduce the spinal needle horizontally to avoid injury to the sciatic nerve.
 Distal Anterolateral Portal
Distal Anterolateral Portal
To access the peripheral compartment–femoral neck region, two portals are used after traction is removed from the extremity.
Peripheral compartment arthroscopy can be done in hip flexion to relax the anterior capsule or in neutral flexion extension.
The anterolateral portal is used as one portal.
A distal anterolateral portal is established 3 to 5 cm distal to the anterolateral portal, just anterior to the lateral aspect of the proximal femoral shaft and neck (TECH FIG 6).
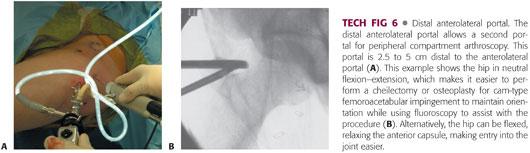
Fluoroscopy is used to guide portal placement.
The portal penetrates the gluteus medius muscle and upper vastus lateralis.
The spinal needle should enter the peripheral compartment laterally. The guidewire is brought through the spinal needle and can be gently advanced to the medial capsule—the easy passage until the medial capsule is reached helps confirm that one is in the peripheral compartment.
The skin incision is made, and the trocar and the sheath are passed over the guidewire.
The sheath and guidewire are exchanged for the arthroscope or instrumentation.
Arthroscopy and fluoroscopy can be used together to perform surgery in the peripheral compartment.
PEARLS AND PITFALLS | |
Patient selection |
|
| |
| |
Hip distraction |
|
| |
| |
| |
Patient positioning |
|
| |
Portal placement |
|
| |
| |
| |
| |
| |
| |
POSTOPERATIVE CARE
 Traction is released.
Traction is released.
 Long-acting local anesthetic is injected into the joint.
Long-acting local anesthetic is injected into the joint.
 The portals are sutured, and a sterile dressing is applied to the wounds.
The portals are sutured, and a sterile dressing is applied to the wounds.
 Arthroscopy is an outpatient procedure and the patient typically leaves recovery room after 1 to 3 hours.
Arthroscopy is an outpatient procedure and the patient typically leaves recovery room after 1 to 3 hours.
 If arthroscopy does not involve bony recontouring of the femoral neck, labral repair, or microfracture of the articular surfaces, then the patient is allowed to walk immediately, although weight bearing should be assisted with crutches for 3 to 7 days or until gait pattern is normalized.
If arthroscopy does not involve bony recontouring of the femoral neck, labral repair, or microfracture of the articular surfaces, then the patient is allowed to walk immediately, although weight bearing should be assisted with crutches for 3 to 7 days or until gait pattern is normalized.
 Rehabilitation should take into consideration soft tissue healing constraints, control of swelling and pain, early ROM, limitations on weight bearing, early initiation of muscle activity and neuromuscular control, progressive lower extremity strengthening and proprioceptive retraining, cardiovascular training, and sport-specific training.
Rehabilitation should take into consideration soft tissue healing constraints, control of swelling and pain, early ROM, limitations on weight bearing, early initiation of muscle activity and neuromuscular control, progressive lower extremity strengthening and proprioceptive retraining, cardiovascular training, and sport-specific training.
 Swelling and pain are controlled by ice and nonaspirin, nonsteroidal anti-inflammatory drugs.
Swelling and pain are controlled by ice and nonaspirin, nonsteroidal anti-inflammatory drugs.
 The dressing is removed on the first or second postoperative day, and the wound is covered with adhesive bandages.
The dressing is removed on the first or second postoperative day, and the wound is covered with adhesive bandages.
 Portal sutures are removed a few days after surgery.
Portal sutures are removed a few days after surgery.
 Patients who undergo labrum repairs on the anterior superior region and capsulorraphy should follow specific ROM and weight-bearing guidelines.
Patients who undergo labrum repairs on the anterior superior region and capsulorraphy should follow specific ROM and weight-bearing guidelines.
 Patients who undergo osteoplasty should limit impact activities that increase the risk of femoral neck fracture during the initial several weeks.
Patients who undergo osteoplasty should limit impact activities that increase the risk of femoral neck fracture during the initial several weeks.
 Patients who undergo microfracture should adhere to 8 weeks of protected weight bearing on crutches.
Patients who undergo microfracture should adhere to 8 weeks of protected weight bearing on crutches.
OUTCOMES
 Record functional and prosthetic survivorship data, as applicable.
Record functional and prosthetic survivorship data, as applicable.
 Loose bodies are the clearest indication for arthroscopy, resulting in less morbidity and faster recovery than open surgery.4
Loose bodies are the clearest indication for arthroscopy, resulting in less morbidity and faster recovery than open surgery.4
 Labral débridement has been shown to result in successful outcomes in 68% to 82% of cases, with positive outcomes associated with isolated tears and poorer prognosis associated with arthritis.2,5,12
Labral débridement has been shown to result in successful outcomes in 68% to 82% of cases, with positive outcomes associated with isolated tears and poorer prognosis associated with arthritis.2,5,12
 Débridement of ligamentum teres, such as labral débridement, has shown best results when lesions are isolated and without associated acetabular fracture or significant osteochondral defect of either the acetabulum or femoral head.
Débridement of ligamentum teres, such as labral débridement, has shown best results when lesions are isolated and without associated acetabular fracture or significant osteochondral defect of either the acetabulum or femoral head.
 Treatment of hip DJD by arthroscopy has shown unpredictable results, with a range of 34% to 60% of patients reporting improvement of symptoms after arthroscopic débridement for DJD.6,13
Treatment of hip DJD by arthroscopy has shown unpredictable results, with a range of 34% to 60% of patients reporting improvement of symptoms after arthroscopic débridement for DJD.6,13
 One study reported that 86% of patients treated for chondral lesions by microfracture showed a successful response at 2-year follow-up.1
One study reported that 86% of patients treated for chondral lesions by microfracture showed a successful response at 2-year follow-up.1
 Arthroscopic synovectomy is palliative, and success is based on the integrity of the articular cartilage.
Arthroscopic synovectomy is palliative, and success is based on the integrity of the articular cartilage.
 Treatment of femoroacetabular impingement has shown better outcomes when there is less DJD.
Treatment of femoroacetabular impingement has shown better outcomes when there is less DJD.
 Treatment of avascular necrosis is controversial—the results are better when the articular surface is not disrupted or when treating mechanical symptoms.
Treatment of avascular necrosis is controversial—the results are better when the articular surface is not disrupted or when treating mechanical symptoms.
O’Leary10 reported 40% of patients improved at 30-month follow-up.
 More specifics are provided in the chapters describing specific techniques for the different processes treated about the hip.
More specifics are provided in the chapters describing specific techniques for the different processes treated about the hip.
COMPLICATIONS
 Traction neurapraxia
Traction neurapraxia
 Direct trauma to pudendal, lateral femoral cutaneous, femoral, and sciatic nerves
Direct trauma to pudendal, lateral femoral cutaneous, femoral, and sciatic nerves
 Iatrogenic labral and chondral damage
Iatrogenic labral and chondral damage
 Fluid extravasation
Fluid extravasation
 Vaginal tear
Vaginal tear
 Pressure necrosis to scrotum, labia and perineum, and foot
Pressure necrosis to scrotum, labia and perineum, and foot
 Labia and perineum hematoma
Labia and perineum hematoma
 Knee ligament injury
Knee ligament injury
 Ankle fracture
Ankle fracture
 Femoral head avascular necrosis
Femoral head avascular necrosis
 Fracture of femoral neck
Fracture of femoral neck
 Instrument breakage
Instrument breakage
 Portal hematoma and bleeding
Portal hematoma and bleeding
REFERENCES
1. Byrd JWT, Jones KS. Microfracture for grade IV chondral lesions of the hip. Arthroscopy 2004;20:89.
2. Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy 2000;16:578–587.
3. Carreira D, Bush-Joseph CA. Hip arthroscopy. Orthopedics 2006;29:517–523.
4. Epstein H. Posterior fracture-dislocations of the hip: comparison of open and closed methods of treatment in certain types. J Bone Joint Surg Am 1961;43A:1079–1098.
5. Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labrum tears. Arthroscopy 1999;15:132–137.
6. Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for degenerative joint disease. Arthroscopy 1998;14:435.
7. Hyman JL, Salvati EA, Laurencin CT, et al. The arthroscopic drainage, irrigation, and débridement of late, acute total hip arthroplasty infections: average 6-year follow-up. J Arthroplasty 1999;14:903–910.
8. Kelly BT, Williams RJ III, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med 2003;31(6):1020–1037.
9. McCarthy JC, Noble PC, Schuck MR, et al. The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res 2001;393:25–37.
10. O’Leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy 2001;17:181–188.
11. Safran MR. Evaluation of the hip: history, physical examination, and imaging. Oper Tech Sports Med 2005;13:2–12.
12. Santori N, Villar RN. Acetabular labral tears: results of arthroscopic partial limbectomy. Arthroscopy 2000;16:11–15.
13. Villar RN. Arthroscopic debridement of the hip: a minimally invasive approach to osteoarthritis. J Bone Joint Surg Br 1991;73B:170–171.
< div class='tao-gold-member'>



















