Although the term sports hernia is commonly used in the media, athletic pubalgia is a more appropriate term to describe the constellation of injuries causing chronic groin pain in athletes.
Diagnosis of the cause of groin pain is difficult due to the complex anatomy of the groin and the fact that two or more injuries may coexist.
Intra-abdominal pathology, genitourinary abnormalities, referred lumbosacral pain, and hip joint disorders must first be excluded.
 Adductor strains are the most common cause of groin pain in athletes.
Adductor strains are the most common cause of groin pain in athletes.
The adductors are usually strained during eccentric contraction of the muscles. The injury often occurs at the myotendinous junction, but the strain also can occur in the tendon itself or its bony insertion.
Other muscles in and around the groin region also can be strained, including the rectus femoris, the sartorius, abdominal muscles, and the conjoint tendon.
 Sports hernia is a condition of chronic groin pain that is caused by a tear in the inguinal floor without a clinically obvious hernia.7,11
Sports hernia is a condition of chronic groin pain that is caused by a tear in the inguinal floor without a clinically obvious hernia.7,11
Sports hernias result in an occult injury that usually is not identified by most examiners. However, with increasing experience, the examiner can feel an abnormal inguinal floor and appreciate abnormal tenderness inside the external ring.
In contrast, indirect and direct hernias involve easily palpable defects in the inguinal canal or through the anterior abdominal musculature, respectively.
Duration of symptoms typically is months, and pain is resistant to conservative measures.
 Osteitis pubis is characterized by symphysis pain and joint disruption and occurs commonly in distance runners and soccer players.
Osteitis pubis is characterized by symphysis pain and joint disruption and occurs commonly in distance runners and soccer players.
It may be difficult to distinguish from adductor strains, and the two conditions may coincide.
 Stress fractures are rare injuries that result from repetitive cyclic loading of the bone.
Stress fractures are rare injuries that result from repetitive cyclic loading of the bone.
The pubic rami are the most common location for stress fractures in the pelvis. These fractures are most common in long-distance runners.
ANATOMY
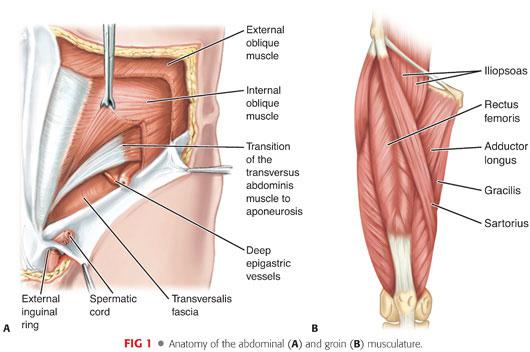
 The anatomy in and around the groin is complex (FIG 1), and a thorough understanding of it is crucial in diagnosing the various groin injuries.
The anatomy in and around the groin is complex (FIG 1), and a thorough understanding of it is crucial in diagnosing the various groin injuries.
 In terms of athletic pubalgia, the pelvis is considered to contain two joints: the commonly known ball-and-socket of the hip joint and the second, less well known “pubic bone joint.”
In terms of athletic pubalgia, the pelvis is considered to contain two joints: the commonly known ball-and-socket of the hip joint and the second, less well known “pubic bone joint.”
The pubic bone joint consists of a large, complex rotational joint that involves both pubic bones and all the soft tissue attachments on either side of the pubis (FIG 2).
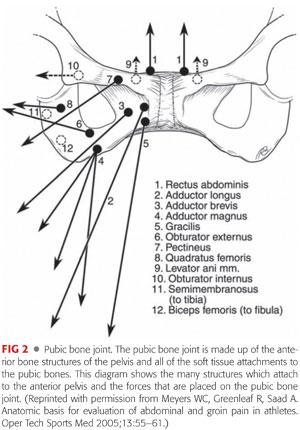
The pubic symphysis is the center point of the pubic bone joint and is the site of numerous musculotendinous attachments that act to dynamically stabilize the position of the anterior pelvis.
The abdominal muscles attaching to the pubic symphysis consist of the external and internal oblique muscles, transversus abdominis, and rectus abdominis. The thigh adductors attaching to the pelvis include the pectineus, gracilis, adductor longus, brevis, and magnus.
 The posterior inguinal wall consists primarily of the transversalis fascia, along with the conjoint tendon, made up of the internal abdominal oblique and transversus abdominis aponeuroses.7
The posterior inguinal wall consists primarily of the transversalis fascia, along with the conjoint tendon, made up of the internal abdominal oblique and transversus abdominis aponeuroses.7
 The conjoint tendon inserts onto the pubic tubercle and along the iliopubic tract.
The conjoint tendon inserts onto the pubic tubercle and along the iliopubic tract.
PATHOGENESIS
 The most robust and important muscles for maintaining stability of the anterior pelvis are the rectus abdominis and the adductor longus muscles.
The most robust and important muscles for maintaining stability of the anterior pelvis are the rectus abdominis and the adductor longus muscles.
These muscle groups pull the pelvis with opposite vectors and function as antagonists to one another during flexion, extension, and rotation of the pelvis (FIG 3).
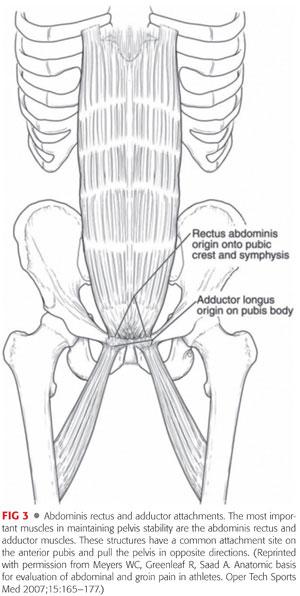
A tremendous amount of torque is created at the level of the pelvis in athletes participating in sports requiring twisting and cutting. The cutting and twisting activities require the use of the abdominal and pelvic muscles, which creates significant force through the pelvis and stress on the tendinous insertions.
 Overuse injuries due to repetitive hip hyperextension and truncal rotational movements lead to wear and tear of the tendon insertions culminating in partial or full tearing of these structures. When one muscle weakens or its associated tendon torn, the result is an unequal distribution of pelvic forces and overpulling of one of the muscles leading to more anterior or posterior pelvic tilt, depending on which muscle or tendon is injured.
Overuse injuries due to repetitive hip hyperextension and truncal rotational movements lead to wear and tear of the tendon insertions culminating in partial or full tearing of these structures. When one muscle weakens or its associated tendon torn, the result is an unequal distribution of pelvic forces and overpulling of one of the muscles leading to more anterior or posterior pelvic tilt, depending on which muscle or tendon is injured.
NATURAL HISTORY
 A majority of acute adductor strains will improve with appropriate conservative treatment over a course of 2 to 6 weeks. However, if not properly rehabilitated, an adductor injury may progress to chronic strains or tendinopathy.
A majority of acute adductor strains will improve with appropriate conservative treatment over a course of 2 to 6 weeks. However, if not properly rehabilitated, an adductor injury may progress to chronic strains or tendinopathy.
 Recovery from athletic pubalgia varies greatly from athlete to athlete. Although many athletes will get improvement with rest and conservative treatment, recurrent symptoms are common after returning to play. A small subset of patients will improve with nonoperative treatment; however, most patients who have been accurately diagnosed with athletic pubalgia will eventually require surgical repair.7,13 A hallmark of sports hernias is that patients have less pain when they are inactive and more pain when active.
Recovery from athletic pubalgia varies greatly from athlete to athlete. Although many athletes will get improvement with rest and conservative treatment, recurrent symptoms are common after returning to play. A small subset of patients will improve with nonoperative treatment; however, most patients who have been accurately diagnosed with athletic pubalgia will eventually require surgical repair.7,13 A hallmark of sports hernias is that patients have less pain when they are inactive and more pain when active.
 Osteitis pubis is self-limited but may take, on average, about 9 months to heal.5
Osteitis pubis is self-limited but may take, on average, about 9 months to heal.5
PATIENT HISTORY AND PHYSICAL FINDINGS
 Patient history is the most important aspect of the evaluation of athletic pubalgia.
Patient history is the most important aspect of the evaluation of athletic pubalgia.
 The patient must be asked for duration of symptoms, any inciting events, relieving and exacerbating factors, and timing of pain.
The patient must be asked for duration of symptoms, any inciting events, relieving and exacerbating factors, and timing of pain.
 A thorough hip examination must be performed to rule out intra-articular hip sources of pain such as labral tears and femoroacetabular impingement (FAI).
A thorough hip examination must be performed to rule out intra-articular hip sources of pain such as labral tears and femoroacetabular impingement (FAI).
Flexion, adduction, and internal rotation of the hip are used to identify anterior FAI. The FABER test (flexion, abduction, and external rotation of the hip) is used to identify posterior impingement.
Decreased hip internal rotation is common in patients with cam-lesion FAI. Internal rotation of less than 25 degrees is considered abnormal.
Hip flexion against resistance: tests the strength of the iliopsoas and may detect a strain or tear of this muscle.
 Groin examination:
Groin examination:
Palpation of the insertion of the rectus and origin of the adductors can identify partial tears, inflammation, or injury to these tendons.
Palpation of insertion of conjoint tendon: Tenderness may increase, and a bulge may be felt by having the patient perform a Valsalva maneuver.
Straight-leg raise: In patients with radicular low back pain, this will reproduce the pain they are having.
Groin adduction resistance: helps to diagnose an adductor strain or tear
Palpation of the pubic symphysis: characteristic of osteitis pubis
Ober test: Patient’s inability to lower the upper leg completely to the examination table is pathognomonic of a tight iliotibial band.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Three views of the affected hip should be obtained including anteroposterior (AP), lateral, and Dunn view to evaluate for possible FAI.
Three views of the affected hip should be obtained including anteroposterior (AP), lateral, and Dunn view to evaluate for possible FAI.
 Radiographs can be helpful in excluding fractures or avulsions.4
Radiographs can be helpful in excluding fractures or avulsions.4
Stress fractures usually are not evident on radiographs.
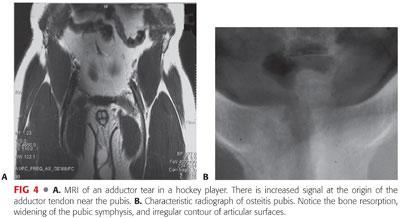
 Magnetic resonance imaging (MRI) can be used to confirm muscle strain or tears and partial or complete tendon tears (FIG 4A).
Magnetic resonance imaging (MRI) can be used to confirm muscle strain or tears and partial or complete tendon tears (FIG 4A).
MRI has been used to detect sports hernias, although it is not always successful.4
MRI can also be used to evaluate for possible hip labral tears.
 Dynamic ultrasound has been found, in certain cases, to detect posterior wall defects but is highly operator dependent.17
Dynamic ultrasound has been found, in certain cases, to detect posterior wall defects but is highly operator dependent.17
 Herniography, which involves an intraperitoneal injection of contrast dye followed by fluoroscopy or radiography, has been shown to identify sports hernias but has limited sensitivity and a substantial risk of perforation in up to 5% of patients.2
Herniography, which involves an intraperitoneal injection of contrast dye followed by fluoroscopy or radiography, has been shown to identify sports hernias but has limited sensitivity and a substantial risk of perforation in up to 5% of patients.2
 Osteitis pubis has characteristic radiologic findings, including bone resorption, widening of the pubic symphysis, and irregular contour of articular surfaces or periarticular sclerosis (FIG 4B).
Osteitis pubis has characteristic radiologic findings, including bone resorption, widening of the pubic symphysis, and irregular contour of articular surfaces or periarticular sclerosis (FIG 4B).
A bone scan may show increased uptake in the area of the pubic symphysis in osteitis pubis; however, not all patients who have symptoms show an abnormality.12
MRI has become increasingly useful in the diagnosis of osteitis pubis. Findings can include bone marrow edema or symphysial disc extrusion.16
DIFFERENTIAL DIAGNOSIS
 Groin disruption or strain
Groin disruption or strain
 Labral tear of the hip
Labral tear of the hip
 Cam or pincer FAI
Cam or pincer FAI
 Osteitis pubis
Osteitis pubis
 Pelvic stress fractures
Pelvic stress fractures
 Indirect and direct hernia
Indirect and direct hernia
 Avascular necrosis of the hip
Avascular necrosis of the hip
 Hip osteoarthritis
Hip osteoarthritis
 Abdominal muscle tear
Abdominal muscle tear
 Lumbar radiculopathy
Lumbar radiculopathy
 Nerve entrapment
Nerve entrapment
 Tumors
Tumors
 Genitourinary problems
Genitourinary problems
 Inflammatory bowel disease
Inflammatory bowel disease
 Endometriosis
Endometriosis
 Pelvic inflammatory disease
Pelvic inflammatory disease
NONOPERATIVE MANAGEMENT
 Initial treatment for lower abdominal strains or groin injuries consists of activity modification, anti-inflammatory medication, and physical therapy.
Initial treatment for lower abdominal strains or groin injuries consists of activity modification, anti-inflammatory medication, and physical therapy.
Core-strengthening exercises target the abdomen, lumbar spine, and hips.
Stretching focuses on the hip rotators, adductors, and hamstrings.
The goal of therapy is to correct the imbalance of the hip and pelvic muscle stabilizers.18
After 4 to 6 weeks, the athlete gradually returns to sport-specific activities as tolerated.
Acute treatment of adductor strain includes rest, ice, compression, and elevation.
The next goal is restoration of range of motion (ROM) and prevention of atrophy. Once the patient can tolerate this, the focus should be to regain strength, flexibility, and endurance.8
 Nonoperative management of athletic pubalgia includes physical therapy, anti-inflammatory drugs, and corticosteroid injections at the site of pain.1,9
Nonoperative management of athletic pubalgia includes physical therapy, anti-inflammatory drugs, and corticosteroid injections at the site of pain.1,9
 Osteitis pubis is a self-limiting condition; therapy should focus on hip ROM as well as adductor stretching and strengthening.
Osteitis pubis is a self-limiting condition; therapy should focus on hip ROM as well as adductor stretching and strengthening.
Corticosteroid injection in osteitis pubis is controversial but may be helpful in select populations of athletic patients.10,16
 Treatment in pelvic stress fractures is straightforward and involves 4 to 6 weeks of rest from the activities aggravating the area.
Treatment in pelvic stress fractures is straightforward and involves 4 to 6 weeks of rest from the activities aggravating the area.
SURGICAL MANAGEMENT
 Surgical exploration and repair is indicated if nonoperative treatment fails and alternative diagnoses have been excluded.
Surgical exploration and repair is indicated if nonoperative treatment fails and alternative diagnoses have been excluded.
 Three general categories of surgical repair are described, including pelvic floor repair with mesh, primary pelvic floor repair without mesh, and laparoscopic mesh repair.
Three general categories of surgical repair are described, including pelvic floor repair with mesh, primary pelvic floor repair without mesh, and laparoscopic mesh repair.
 There is no consensus to which surgical approach is best.
There is no consensus to which surgical approach is best.
 Some feel the use of mesh in athletes is not recommended due to the localized stiffness of the abdominal muscles and restricted movement caused by the mesh.15
Some feel the use of mesh in athletes is not recommended due to the localized stiffness of the abdominal muscles and restricted movement caused by the mesh.15
 Our preferred management of adductor injuries that occur in conjunction with athletic pubalgia is to treat the underlying inguinal floor injury surgically and to manage the adductor component by therapy and rehabilitation.
Our preferred management of adductor injuries that occur in conjunction with athletic pubalgia is to treat the underlying inguinal floor injury surgically and to manage the adductor component by therapy and rehabilitation.
Preoperative Planning
 Preoperative planning involves extreme care to ascertain that the patient truly has athletic pubalgia and not another disease process. This requires a complete history and physical examination performed by an examiner who understands the pathophysiology of this injury.
Preoperative planning involves extreme care to ascertain that the patient truly has athletic pubalgia and not another disease process. This requires a complete history and physical examination performed by an examiner who understands the pathophysiology of this injury.
 The preoperative MRI can be used to plan the surgery. Evaluation of the rectus insertion can help in determining whether a formal rectus repair is necessary compared to simply tightening the muscle insertion.
The preoperative MRI can be used to plan the surgery. Evaluation of the rectus insertion can help in determining whether a formal rectus repair is necessary compared to simply tightening the muscle insertion.
Positioning
 The patient is positioned supine and draped with the affected groin exposed.
The patient is positioned supine and draped with the affected groin exposed.
Anesthesia
 We use general anesthesia for our surgery.
We use general anesthesia for our surgery.
 Preemptive analgesia is important to reduce postoperative pain and to make the anesthetic experience smoother. Also, local anesthesia is bactericidal, reducing the risk of infection.
Preemptive analgesia is important to reduce postoperative pain and to make the anesthetic experience smoother. Also, local anesthesia is bactericidal, reducing the risk of infection.
 We suggest 0.25% Marcaine with epinephrine and sodium bicarbonate.
We suggest 0.25% Marcaine with epinephrine and sodium bicarbonate.
TECHNIQUES
 The Minimal Repair Technique
The Minimal Repair Technique
Incision, Dissection, and Site Evaluation
The incision is made along the path of the inguinal ligament, 1 cm medial and superior to the ligament. A length of 5 to 6 cm is adequate.
Dissection is performed down to the external oblique fascia.
The external oblique is incised to the external ring, and the fascia is mobilized both medially and laterally.
The spermatic cord is carefully evaluated and mobilized.
The strength of the posterior inguinal wall is evaluated by digital palpation.
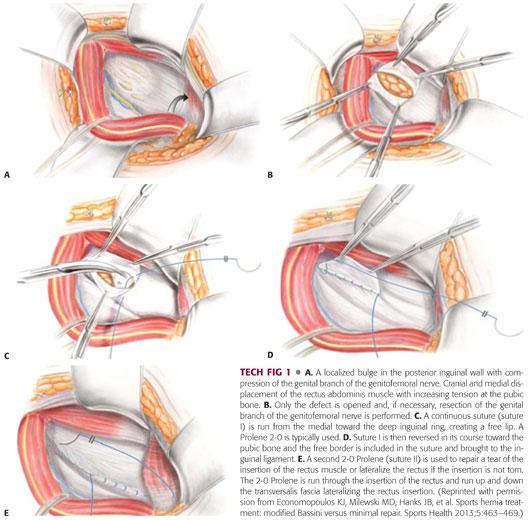
Typically, a circumscribed weakness is found in the posterior wall with the surrounding tissue being firm and intact (TECH FIG 1A).
Repair
The transversalis fascia is split, starting in the area of the defect toward the deep internal ring (TECH FIG 1B).
The transversalis fascia is only opened in the area where weakness is appreciated, and normal tissue is not opened.
The genital branch of the genitofemoral nerve is assessed.
If the nerve is uninjured, it is retracted out of the zone of injury.
If the nerve is entrapped, a neurolysis is performed.
A severely injured and fibrotic nerve is resected.
A continuous 2-0 Prolene suture (suture I) is performed from the medial toward the deep inguinal ring, creating a free fascial lip out of the iliopubic tract (TECH FIG 1C).
The suture is then reversed and run toward the pubic bone (TECH FIG 1D).
The free lip is then included in the suture and brought to the inguinal ligament.
A second suture (suture II) is used to stabilize or repair the rectus abdominis. If a tear is present, a primary repair back down to the pubis is performed. If the insertion of the rectus is attenuated but not torn, suture II is used to lateralize the rectus. This is accomplished by suturing the lateral edge of the rectus to the transversalis fascia (TECH FIG 1E).
This second suture is used to lateralize the rectus abdominis if no tear is present. This suture counteracts the increased tension at the pubic bone caused by the retraction of the rectus muscle in the upward and medial direction.
Marcaine is injected thoroughly, and the external oblique, Scarpa fascia, and skin are closed with an absorbable suture.
PEARLS AND PITFALLS | |
| |
| |
| |
| |
POSTOPERATIVE CARE
 The goal of rehabilitation is to establish a full, normal ROM and flexibility followed by incremental increases in resistance for strength training.
The goal of rehabilitation is to establish a full, normal ROM and flexibility followed by incremental increases in resistance for strength training.
 Athletes are permitted to lift up to 20 kg immediately after surgery.
Athletes are permitted to lift up to 20 kg immediately after surgery.
 Biking with no resistance may be started on the second postoperative day.
Biking with no resistance may be started on the second postoperative day.
 Runners should be running in 2 weeks and golfers golfing in 1 week.
Runners should be running in 2 weeks and golfers golfing in 1 week.
 Contact athletes should be able to return to competition in 3 to 4 weeks.
Contact athletes should be able to return to competition in 3 to 4 weeks.
OUTCOMES
 With appropriate indications and surgical technique, success rates in sports hernia repair have been as high as 97% to 100% in high-performance athletes, with success measured as a return to previous levels of performance and freedom from pain.6,14
With appropriate indications and surgical technique, success rates in sports hernia repair have been as high as 97% to 100% in high-performance athletes, with success measured as a return to previous levels of performance and freedom from pain.6,14
 Using the minimal repair technique, 96.1% of patients resumed training at the 4-week point. The median time to return to training was 7 days. In a subset of professional athletes, 83.7% had returned to unrestricted sports activities at the 1-month follow-up.15
Using the minimal repair technique, 96.1% of patients resumed training at the 4-week point. The median time to return to training was 7 days. In a subset of professional athletes, 83.7% had returned to unrestricted sports activities at the 1-month follow-up.15
 Our own study found patients who underwent the minimal repair technique returned to sports at a median of 5.6 weeks, which was significantly faster compared with the modified Bassini repair group, with the median return of 25.8 weeks.3
Our own study found patients who underwent the minimal repair technique returned to sports at a median of 5.6 weeks, which was significantly faster compared with the modified Bassini repair group, with the median return of 25.8 weeks.3
COMPLICATIONS
 Recurrence
Recurrence
 Thigh pain in the early postoperative period
Thigh pain in the early postoperative period
 Infection
Infection
 Hematoma
Hematoma
 Continued pain
Continued pain
REFERENCES
1. Ashby EC. Chronic obscure groin pain is commonly caused by enthesopathy: “tennis elbow” of the groin. Br J Surg 1994;81(11):1632–1634.
2. Calder F, Evans R, Neilson D, et al. Value of herniography in the management of occult hernia and chronic groin pain in adults. Br J Surg 2000;87(6):824–825.
3. Economopoulos KJ, Milewski MD, Hanks JB, et al. Sports hernia treatment: modified Bassini versus minimal repair. Sports Health 2013;5(5):463–469.
4. Ekberg O, Sjoberg S, Westlin N. Sports-related groin pain: evaluation with MR imaging. Eur Radiol 1996;6(1):52–55.
5. Fricker PA, Taunton JE, Ammann W. Osteitis pubis in athletes. Infection, inflammation or injury? Sports Med 1991;12(4):266–279.
6. Genitsaris M, Goulimaris I, Sikas N. Laparoscopic repair of groin pain in athletes. Am J Sports Med 2004;32(5):1238–1242.
7. Hackney RG. The sports hernia: a cause of chronic groin pain. Br J Sports Med 1993;27(1):58–62.
8. Holmich P. Adductor related groin pain in athletes. Sports Med Arthroscopy Rev 1997;5:285–291.
9. Holmich P, Uhrskou P, Ulnits L, et al. Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial. Lancet 1999;353(9151):439–443.
10. Holt MA, Keene JS, Graf BK, et al. Treatment of osteitis pubis in athletes. Results of corticosteroid injections. Am J Sports Med 1995;23(5):601–606.
11. Joesting DR. Diagnosis and treatment of sportsman’s hernia. Curr Sports Med Rep 2002;1(2):121–124.
12. Karlsson J, Jerre R. The use of radiography, magnetic resonance, and ultrasound in the diagnosis of hip, pelvis, and groin injuries. Sports Med Arthroscopy Rev 1997;5268–5273.
13. LeBlanc KE, LeBlanc KA. Groin pain in athletes. Hernia 2003;7(2):68–71.
14. Meyers WC, Foley DP, Garrett WE, et al. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med 2000;28(1):2–8.
15. Muschaweck U, Berger L. Minimal repair technique of sportsmen’s groin: an innovative open-suture repair to treat chronic inguinal pain. Hernia 2010;14(1):27–33.
16. O’Connell MJ, Powell T, McCaffrey NM, et al. Symphyseal cleft injection in the diagnosis and treatment of osteitis pubis in athletes. AJR Am J Roentgenol 2002;179(4):955–959.
17. Orchard JW, Read JW, Neophyton J, et al. Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian Rules footballers. Br J Sports Med 1998;32(2):134–139.
18. Taylor DC. Abdominal musculature abnormalities as a cause of groin pain in athletes. Inguinal hernias and pubalgia. Am J Sports Med 1991;19:239–242.
< div class='tao-gold-member'>







