Estimates indicate that by the year 2030, the volume of primary total knee arthroplasty (TKA) cases will increase to 3,480,000 and the number of revision procedures is expected to rise to 268,200 per year.1
 Indications for removing well-fixed total knee components include infection, malalignment, malpositioning, instability, periprosthetic fracture, stiffness, or aseptic loosening of other part(s).
Indications for removing well-fixed total knee components include infection, malalignment, malpositioning, instability, periprosthetic fracture, stiffness, or aseptic loosening of other part(s).
 Achieving the goal of safe removal of well-fixed components during revision TKA depends on meticulous surgical technique and availability of appropriate instruments. In many ways, these are the most important portions of the revision TKA procedure because careless technique may lead to damage of the remaining bone stock, iatrogenic fracture, and disruption of soft tissues, ultimately compromising the quality of the revision construct and the outcome for the patient.
Achieving the goal of safe removal of well-fixed components during revision TKA depends on meticulous surgical technique and availability of appropriate instruments. In many ways, these are the most important portions of the revision TKA procedure because careless technique may lead to damage of the remaining bone stock, iatrogenic fracture, and disruption of soft tissues, ultimately compromising the quality of the revision construct and the outcome for the patient.
ANATOMY
 Removal of well-fixed TKA components necessitates good exposure.
Removal of well-fixed TKA components necessitates good exposure.
 Protection of neurovascular structures and the extensor mechanism is essential. A medial parapatellar arthrotomy allows extensile exposure, and when combined with synovectomy, lateral retinacular release and quadriceps snip provide the necessary exposure required for safe component removal and subsequent reconstruction in most cases. Extensile exposure techniques using a quadriceps snip, tibial tubercle osteotomy, or V-Y quadricepsplasty allow enhanced exposure when necessary and are described in Chapters 37 and 39.
Protection of neurovascular structures and the extensor mechanism is essential. A medial parapatellar arthrotomy allows extensile exposure, and when combined with synovectomy, lateral retinacular release and quadriceps snip provide the necessary exposure required for safe component removal and subsequent reconstruction in most cases. Extensile exposure techniques using a quadriceps snip, tibial tubercle osteotomy, or V-Y quadricepsplasty allow enhanced exposure when necessary and are described in Chapters 37 and 39.
PATHOGENESIS
 Indications for removal of well-fixed TKA components include infection, malalignment, malpositioning, instability, periprosthetic fracture, stiffness, or aseptic loosening of other component(s).
Indications for removal of well-fixed TKA components include infection, malalignment, malpositioning, instability, periprosthetic fracture, stiffness, or aseptic loosening of other component(s).
PATIENT HISTORY AND PHYSICAL FINDINGS
 The history and physical examination should determine whether the patient’s pain is extrinsic or intrinsic to the TKA.
The history and physical examination should determine whether the patient’s pain is extrinsic or intrinsic to the TKA.
 Extrinsic sources of pain (eg, lumbar radiculopathy, referred hip pain) should be considered for differential diagnosis.
Extrinsic sources of pain (eg, lumbar radiculopathy, referred hip pain) should be considered for differential diagnosis.
 Pain that is determined to be intrinsic to the TKA should be correlated with history, physical examination, and radiographic findings to confirm that the cause of the pain can be corrected with revision TKA.
Pain that is determined to be intrinsic to the TKA should be correlated with history, physical examination, and radiographic findings to confirm that the cause of the pain can be corrected with revision TKA.
 Failure to identify a cause for the patient’s pain before performing the revision TKA portends a poor outcome.
Failure to identify a cause for the patient’s pain before performing the revision TKA portends a poor outcome.
 Physical examination includes the following:
Physical examination includes the following:
Visual inspection of the previous incision and the surrounding skin. The most lateral anterior-based incision is selected to avoid wound necrosis and maximize healing potential.
Passive and active range of motion (ROM) is assessed. Normal ROM after TKA ranges from full extension to 120 to 135 degrees. It is important to inform patients that revision TKA may not improve their ROM. Stiff knees may require extensile exposure techniques.
The medial and lateral collateral ligaments are tested in full extension and at 30 degrees of flexion. Coronal plane instability may make it necessary to remove well-fixed components and implant appropriately sized and positioned components, occasionally with more constraint.
The anterior and posterior stability of the knee is assessed. Sagittal plane instability may make it necessary to remove components to improve flexion–extension gap balancing or to compensate for a deficient posterior cruciate ligament (PCL) in patients with a cruciate-retaining design.
The coronal plane alignment is assessed with the patient standing. The femorotibial angle is measured; it is usually 5 to 7 degrees of valgus. It may be necessary to remove well-fixed components to correct malalignment.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Standard radiographic views include standing anteroposterior (AP), lateral, and tangential patellofemoral (Merchant) views.
Standard radiographic views include standing anteroposterior (AP), lateral, and tangential patellofemoral (Merchant) views.
 Full-length standing AP radiographs are useful to determine the overall mechanical alignment of the lower limb.
Full-length standing AP radiographs are useful to determine the overall mechanical alignment of the lower limb.
 The radiographs should include the diaphysis above the femoral prosthesis and well below the tibial prosthesis.
The radiographs should include the diaphysis above the femoral prosthesis and well below the tibial prosthesis.
 The radiographs are assessed for alignment, component positioning and size, joint line position, loosening, bone stock, and osteolysis.
The radiographs are assessed for alignment, component positioning and size, joint line position, loosening, bone stock, and osteolysis.
 Computed tomography (CT) scans are useful to assess for presence and severity of osteolysis or to assess femoral and tibial component rotation.
Computed tomography (CT) scans are useful to assess for presence and severity of osteolysis or to assess femoral and tibial component rotation.
 Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are obtained to screen for the presence of infection.
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are obtained to screen for the presence of infection.
 Aspiration of the knee is indicated if either the ESR or CRP is elevated or if there is clinical suspicion of infection.
Aspiration of the knee is indicated if either the ESR or CRP is elevated or if there is clinical suspicion of infection.
DIFFERENTIAL DIAGNOSIS
 Lumbar radiculopathy
Lumbar radiculopathy
 Hip pathology
Hip pathology
 Neuropathy
Neuropathy
 Complex regional pain syndrome
Complex regional pain syndrome
 Vascular claudication
Vascular claudication
 Primary bone tumors
Primary bone tumors
 Metastatic disease
Metastatic disease
 Inflammatory arthritis
Inflammatory arthritis
 Infection
Infection
NONOPERATIVE MANAGEMENT
 Nonoperative management of failed TKA may consist of activity modification, physical therapy, bracing, and consultation with pain management specialists.
Nonoperative management of failed TKA may consist of activity modification, physical therapy, bracing, and consultation with pain management specialists.
SURGICAL MANAGEMENT
 Surgical management begins with preoperative planning.
Surgical management begins with preoperative planning.
 The patient’s history, physical examination, radiographs, and laboratory studies are reviewed well in advance of the surgery to allow for adequate preparation time.
The patient’s history, physical examination, radiographs, and laboratory studies are reviewed well in advance of the surgery to allow for adequate preparation time.
 The cause for failure of the TKA is determined.
The cause for failure of the TKA is determined.
 The surgical plan is delineated, a primary plan is formulated, and contingency plans are developed.
The surgical plan is delineated, a primary plan is formulated, and contingency plans are developed.
 The appropriate instrumentation, implants, and bone graft (if necessary) are ordered.
The appropriate instrumentation, implants, and bone graft (if necessary) are ordered.
 The knee is exposed, with extensile approaches if necessary.
The knee is exposed, with extensile approaches if necessary.
 Disruption of the prosthesis–cement interface is targeted in cemented components.
Disruption of the prosthesis–cement interface is targeted in cemented components.
 Disruption of the prosthesis–bone interface is targeted in noncemented components.
Disruption of the prosthesis–bone interface is targeted in noncemented components.
 The components are removed carefully with meticulous attention paid to preservation of bone stock and the soft tissues.
The components are removed carefully with meticulous attention paid to preservation of bone stock and the soft tissues.
 The knee is subsequently reconstructed.
The knee is subsequently reconstructed.
 Layered closure is performed carefully.
Layered closure is performed carefully.
Preoperative Planning
 The key to any successful revision TKA is preoperative planning. The reason for failure of the original TKA is determined from study of the preoperative history, physical examination, imaging studies, and laboratory results.
The key to any successful revision TKA is preoperative planning. The reason for failure of the original TKA is determined from study of the preoperative history, physical examination, imaging studies, and laboratory results.
 It is decided whether removal of the femoral, tibial, and/or patellar component is necessary.
It is decided whether removal of the femoral, tibial, and/or patellar component is necessary.
 Previous operative reports are reviewed, with particular attention paid to the surgical approach, releases performed, and implants that were used.
Previous operative reports are reviewed, with particular attention paid to the surgical approach, releases performed, and implants that were used.
 Careful review of the operative report or implant stickers allows planning and availability of compatible implants or tibial polyethylene liners when partial revisions are planned. It should be determined whether the tibial polyethylene component is modular and what sterilization method was used. If some of the index TKA components are to remain in situ, the surgeon must determine whether compatible parts are available. In addition, for some implants, implant-specific extraction devices may facilitate implant removal.
Careful review of the operative report or implant stickers allows planning and availability of compatible implants or tibial polyethylene liners when partial revisions are planned. It should be determined whether the tibial polyethylene component is modular and what sterilization method was used. If some of the index TKA components are to remain in situ, the surgeon must determine whether compatible parts are available. In addition, for some implants, implant-specific extraction devices may facilitate implant removal.
 Radiographs are reviewed for bone stock quality and quantity.
Radiographs are reviewed for bone stock quality and quantity.
 Particular attention is paid to the fixation method of the components. Ultrasonic cement removal tools may facilitate cement removal, particularly in the setting of previously cemented stemmed implants.
Particular attention is paid to the fixation method of the components. Ultrasonic cement removal tools may facilitate cement removal, particularly in the setting of previously cemented stemmed implants.
Surgical Instruments to Have Available Intraoperatively
 Generic or implant-specific femoral and tibial extraction tools
Generic or implant-specific femoral and tibial extraction tools
 Flexible and rigid osteotomes
Flexible and rigid osteotomes
 Narrow and wide osteotomes
Narrow and wide osteotomes
 Oscillating, reciprocating, and microsagittal power saws
Oscillating, reciprocating, and microsagittal power saws
 Gigli saw
Gigli saw
 Moreland cement and noncement removal instruments
Moreland cement and noncement removal instruments
 High-speed burr
High-speed burr
 Vice grips
Vice grips
 Ultrasonic cement removal device
Ultrasonic cement removal device
Positioning
 The patient is positioned supine on the operating table.
The patient is positioned supine on the operating table.
 Two paint rollers are placed in locations to stabilize the foot as the knee is held at both 90 degrees of flexion and hyperflexion.
Two paint rollers are placed in locations to stabilize the foot as the knee is held at both 90 degrees of flexion and hyperflexion.
 The knee is draped to allow for an extensile surgical exposure.
The knee is draped to allow for an extensile surgical exposure.
 The knee is ranged through a full ROM and stressed in all directions to assess stability.
The knee is ranged through a full ROM and stressed in all directions to assess stability.
Approach
 The preferred surgical approach is a standard medial parapatellar approach, although an extensile approach may be necessary (see Chaps. 45 and 46).
The preferred surgical approach is a standard medial parapatellar approach, although an extensile approach may be necessary (see Chaps. 45 and 46).
 Medial subperiosteal exposure with tibial external rotation decreases tension on the patellar tendon. Patella subluxation is preferred over eversion to decrease the risk of patellar tendon avulsion.
Medial subperiosteal exposure with tibial external rotation decreases tension on the patellar tendon. Patella subluxation is preferred over eversion to decrease the risk of patellar tendon avulsion.
 Good exposure is important to allow unimpeded access to interfaces between components and bone or cement, allow axial extraction of existing implants, and protect key structures.
Good exposure is important to allow unimpeded access to interfaces between components and bone or cement, allow axial extraction of existing implants, and protect key structures.
 Implant removal proceeds in the following order (if all components are being removed): tibial polyethylene, femoral component, tibial tray, and patellar component.
Implant removal proceeds in the following order (if all components are being removed): tibial polyethylene, femoral component, tibial tray, and patellar component.
Removal of a modular tibial polyethylene creates more space, enhancing exposure of all components.
Removal of the femoral component initially creates more space for axial extraction of the tibial component.
If the trajectory of removal of the tibial tray is not obstructed by the femoral component, the tibial tray can be removed prior to the femoral component.
TECHNIQUES
 Exposure
Exposure
The extensor mechanism must be subluxed laterally, with careful attention to avoid detaching the insertion of the patellar tendon. We protect the extensor mechanism by using an A-cup Hohmann retractor along the lateral tibial plateau to retract the quadriceps tendon.
A thorough synovectomy is performed and the medial and lateral gutters are recreated.
If there is lateral scarring or retinacular tightness compromising lateral patellar displacement, a lateral retinacular release is helpful in improving lateral patellar translation.
A quadriceps snip may also decrease proximal lateral tightness and facilitate exposure.
The collateral ligaments are identified and protected.
The prosthesis–cement interface of the femoral, tibial, and patellar implants must be adequately visualized and unimpeded exposure must be achieved.
 Tibial Component Polyethylene Removal
Tibial Component Polyethylene Removal
The tibial polyethylene is removed first. This allows a larger working space to ease removal of the components.
If a modular implant was used, it is removed by inserting an osteotome at the interface of the polyethylene and the tray and then levering the polyethylene out. This can also be accomplished with a nonmodular design (TECH FIG 1).
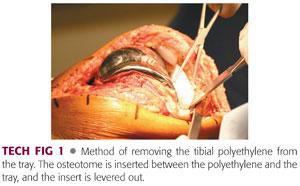
One must be aware that certain posterior-stabilized designs have a reinforcing metal pin in the post which fixes the polyethylene insert to the tray. Other inserts can be secured to the tray with clips or screws. These may need to be removed before the polyethylene can be levered out.
Special instruments from the implant manufacturer may need to be ordered to facilitate removal of the polyethylene.
If special instruments are unavailable, a saw can be used to divide the post, and the pin can be removed with a rongeur.
As a last resort, the tibial tray and polyethylene insert can be removed together as a single unit. However, additional care must be taken to clear the trajectory for two-component extraction.
 Femoral Component Removal
Femoral Component Removal
Initially, a clear visualization of the interface is achieved by removing scar tissue, bone, and cement using an osteotome, curette, rongeur, or burr.
Methods to disrupt the prosthesis–cement interface are listed in the following text:
A thin saw can be used initially with careful protection of the soft tissues.
We typically use a reciprocating saw in the interface along the anterior surface around the femoral component as well as along the anterior chamfer and distal surface (TECH FIG 2A).
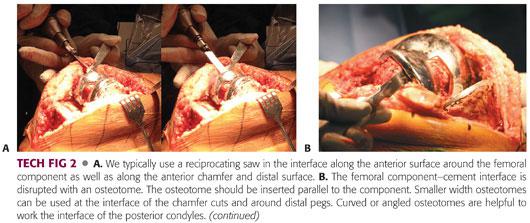
We then use osteotomes to continue to disrupt these interfaces for the posterior chamfer and the posterior condylar interface (TECH FIG 2B,C).
Thin osteotomes are preferred for well-fixed cementless implants to minimize bone loss.
Rigid osteotomes are easier to control and often work better for cemented implants when properly placed in the interval between the implant and cement and often displace the implant from the cement. However, care must be taken, as excessive levering can impact or fracture the bone of the distal femur.
Straight osteotomes are suitable for clearing the anterior flange and posterior condyles as well as the outer portion of the medial and lateral condylar “runners.”
Narrow osteotomes are used for the chamfer cuts and for prostheses where there are pegs at the distal aspect of the component.
The posterior condylar interface can be disrupted with a curved, angled, or offset osteotome.
It may be necessary to use a metal-cutting instrument if certain implants, specifically PCL-sacrificing implants with a central housing, do not come out easily after releasing all available surfaces. This allows exposure of the inner interfaces of the runners, which can be disrupted with osteotomes.
Care must be taken with the use of Gigli saws, as they can result in the removal of more bone than is seen with the meticulous use of osteotomes.
The interfaces should be worked from the medial and lateral sides rather than attempting to traverse the entire prosthesis with the instruments. This allows a more controlled division of the interface and minimizes iatrogenic bone loss.
It is important to direct the removal instruments parallel to the component to avoid removing additional bone unnecessarily.
After the prosthesis–cement interface is disrupted, it is possible to remove the implant easily by hand, with light taps from a punch set on the anterior flange or with an extraction device.
Alternatively, a femoral extractor that grasps the distal aspect of the femoral component can be used to gently remove the implant (TECH FIG 2D). Excessive force may result in unnecessary bone loss or fracture.
If it is difficult to extract the implant, the surgeon must reassess and ensure all interfaces have been disrupted. Axial extraction is important in these cases.
The remaining cement is then removed with saws, burrs, osteotomes, and curettes. Cement gouges and splitters can break the cement plug or mantle.
Ultrasonic instruments facilitate bone preservation during cement removal, especially with cemented, stemmed implants. Ultrasonic instruments are occasionally useful in disrupting the prosthesis–bone interface in noncemented implants.
 Tibial Component Removal
Tibial Component Removal
Methods to disrupt the prosthesis–cement interface are listed below.
The prosthesis–cement interface is initially disrupted with an osteotome or saw to separate the interface. If the component does not separate readily from the cement mantle–bone portion, then further work with saws or osteotomes is necessary. Excessive force will lead to unnecessary bone loss or fracture.
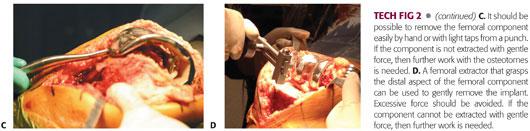
A thin oscillating saw blade, with careful protection of the soft tissues, can also be used initially to disrupt the interface medial to the patellar tendon (TECH FIG 3A). Oscillating saws can be the easiest way of disrupting the interface, but care must be taken to protect the patellar tendon and collateral ligaments.
The area under the tray posterior and lateral to the patellar tendon is not safely accessible to an oscillating saw and can be disrupted with a narrower reciprocating saw or osteotome (TECH FIG 3B).
Narrow and broad osteotomes are effective but care must be taken to avoid impaction or fracture of the underlying bone when levering is used to extract the implant (TECH FIG 3C).
Stacking of osteotomes can disrupt the interface between the prosthesis and cement and facilitate tibial component extraction. When stacking osteotomes, it is important that the widest osteotome be adjacent to tibial bone to distribute force over a large surface area and decrease the risk of tibial bone compression or fracture (TECH FIG 3D).
Once the interface is disrupted prior to extraction, a clear trajectory for egress of the tibial component must be achieved.
The tibia can be externally rotated to provide access to the posterior aspect of the component. Care must be taken to protect the neurovascular structures posteriorly.
The tibia can be hyperflexed and anteriorly subluxed or dislocated to provide access to the posterolateral aspect of the tibia. The tibial component must clear the posterolateral femoral condyle. Care must be taken to avoid injury to the patellar tendon and medial collateral ligament.
Once the implant interface is entirely disrupted, it can be removed by hand with a punch or generic or implant-specific extractions devices.
We prefer to use a femoral extractor to extract the tibial component if hand removal is inadequate (TECH FIG 3E,F). This allows even force distribution while elevating the tibial component, preserving bone stock around the keel.
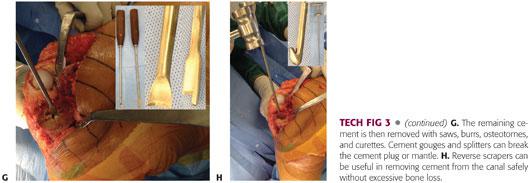
The remaining cement is then removed with saws, burrs, osteotomes, and curettes. Cement gouges and splitters can break the cement plug or mantle (TECH FIG 3G). Cement drills can create a central hole in the cement plug and reverse scrapers can be useful in removing cement from the canal (TECH FIG 3H).
If the implants are press-fitted, a similar means of removal can be used at the prosthesis bone interface.
 Patellar Component Removal
Patellar Component Removal
The removal of a well-fixed polyethylene patellar component should be done only after thoughtful consideration.
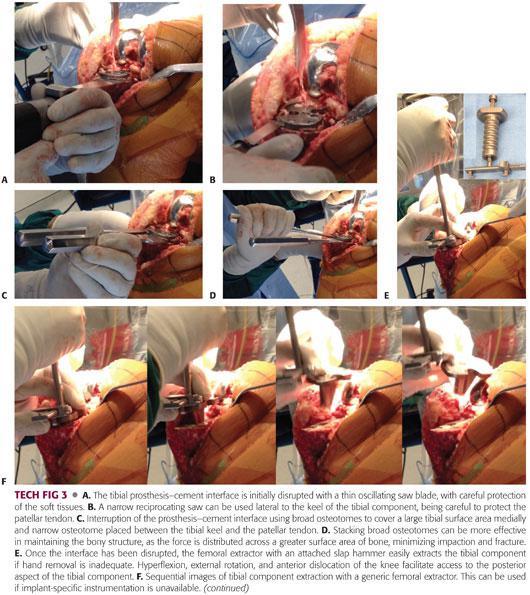
The remaining patella bone stock is often thin and osteopenic with one or several stress risers from previous fixation pegs. It is usually covered with a scar that should be débrided prior to finalizing the decision for removal or retention of the component (TECH FIG 4A).

The target interface is disrupted with a thin saw blade.
All polyethylene components can be removed with a saw blade and the pegs subsequently burred. Cementless components may require the use of a metal-cutting diamond wheel to sever the pegs from the plate. A pencil-tip burr can then be used to remove the pegs (TECH FIG 4B,C).
Any remaining cement is removed with curettes, saws, and burrs.
 Stemmed Implant Removal
Stemmed Implant Removal
Stemmed implants can usually be removed once the fixation between the condylar portion of the femoral component and the tray portion of the tibial component has been separated from the bone.
Preoperative planning should take into consideration the use of stemmed implants, which may complicate extraction of the component.
Some modular designs allow for disassembly of the stem from the remainder of the implant.
Metal-cutting burrs may be necessary to separate the condylar portion of the femoral implant or the keel portion of the tibial implant from the stem. The stem can then be removed with trephine reamers, burrs, or ultrasonic tools. Some companies may make special extraction devices available to assist in removal of the stem.
Rarely, it may be necessary to perform a tibial tubercle osteotomy to extract well-fixed stems.
PEARLS AND PITFALLS | |
Preoperative planning |
|
Preoperative workup |
|
| |
| |
| |
Intraoperative technique |
|
| |
| |
| |
| |
| |
COMPLICATIONS
 Bone loss
Bone loss
 Fracture
Fracture
 Ligament disruption
Ligament disruption
 Tendon disruption
Tendon disruption
REFERENCE
1. Kurtz S, Ong KL, Schmier J, et al. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am 2007;89A:144–151.
< div class='tao-gold-member'>














