Extensor mechanism disruption following total knee arthroplasty (TKA) is a devastating complication, with a prevalence of 0.17% to 2.5%.1,3
 The patella tendon is involved more commonly (0.22%) than the quadriceps tendon (0.1%).
The patella tendon is involved more commonly (0.22%) than the quadriceps tendon (0.1%).
 Despite reports of encouraging results following direct repair in native knees, primary repair in TKA rarely results in successful restoration of extensor function.
Despite reports of encouraging results following direct repair in native knees, primary repair in TKA rarely results in successful restoration of extensor function.
 Augmentation or reconstruction with allograft tissue is recommended to increase success of repair.
Augmentation or reconstruction with allograft tissue is recommended to increase success of repair.
ANATOMY
 The patella tendon connects the tibia and the patella. It originates from the inferior pole of the patella and inserts onto the tibial tuberosity. It is about 5 to 6 cm long and 3 cm wide.
The patella tendon connects the tibia and the patella. It originates from the inferior pole of the patella and inserts onto the tibial tuberosity. It is about 5 to 6 cm long and 3 cm wide.
 Anteriorly, the fibers of the rectus femoris traverse the patella and insert on the tibial tubercle inferior to the patella as the patella tendon.
Anteriorly, the fibers of the rectus femoris traverse the patella and insert on the tibial tubercle inferior to the patella as the patella tendon.
 The fibers of the vastus lateralis muscle expand to the superolateral border of the patella and proximal tibia to form the lateral retinaculum.
The fibers of the vastus lateralis muscle expand to the superolateral border of the patella and proximal tibia to form the lateral retinaculum.
 The fibers of the vastus medialis muscle insert into the superomedial border of the patella and tibia to form the medial retinaculum.
The fibers of the vastus medialis muscle insert into the superomedial border of the patella and tibia to form the medial retinaculum.
PATHOGENESIS
 The etiology of extensor mechanism disruption is multifactorial.
The etiology of extensor mechanism disruption is multifactorial.
 Factors associated with patella tendon rupture include the following:
Factors associated with patella tendon rupture include the following:
Difficult exposure in stiff knees
Extensive release of the patella tendon at the time of surgical exposure
Manipulation for treatment of limited motion
Revision TKA
Malrotation of the components
Overly aggressive postoperative physical therapy
Distal realignment procedures
 Factors associated with quadriceps tendon rupture include the following:
Factors associated with quadriceps tendon rupture include the following:
Steroid use
Systemic diseases such as diabetes mellitus, chronic renal failure, Parkinson disease, or gout
Morbid obesity
Multiple intra-articular injections
Lateral release
Quadriceps snip
NATURAL HISTORY
 Only partial ruptures, where active extension is intact, can be treated with observation.
Only partial ruptures, where active extension is intact, can be treated with observation.
 The majority of full-thickness ruptures require surgical intervention.
The majority of full-thickness ruptures require surgical intervention.
 Direct repair following TKA rarely results in successful restoration of extensor function.
Direct repair following TKA rarely results in successful restoration of extensor function.
 Augmentation with autograft or allograft tissue often is required.
Augmentation with autograft or allograft tissue often is required.
PATIENT HISTORY AND PHYSICAL FINDINGS
 The patient presents with weak or no active extension of the knee.
The patient presents with weak or no active extension of the knee.
 Quadriceps tendon rupture
Quadriceps tendon rupture
An injury is often associated with tear, such as a fall or vigorous activity.
Patient presents with severe pain and weakness.
There is difficulty with weight bearing.
Pain is localized just above the patella.
On examination, there is swelling of the knee with tenderness in the quadriceps tendon. There may be a palpable defect above the superior pole of the patella.
 Patella tendon rupture
Patella tendon rupture
Patients may or may not report a history of injury.
Often occurs intraoperatively or in the perioperative period.
Presents with pain at the region of the tibial tubercle
It may be difficult to distinguish normal surgical pain from patella tendon rupture.
On examination, the most common finding is a high-riding patella. There is swelling and pain below the patella.
There may be a palpable defect at the level of the patella tendon.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Anteroposterior (AP) and lateral radiographs of the knee should be obtained.
Anteroposterior (AP) and lateral radiographs of the knee should be obtained.
 Comparison with immediate postoperative or preoperative films is helpful.
Comparison with immediate postoperative or preoperative films is helpful.
 Patella alta may be present in complete patella tendon rupture (FIG 1).
Patella alta may be present in complete patella tendon rupture (FIG 1).

 Patella baja or distal position of the patella may be present in quadriceps tendon rupture. However, a normal patella position does not rule out rupture of the quadriceps tendon.
Patella baja or distal position of the patella may be present in quadriceps tendon rupture. However, a normal patella position does not rule out rupture of the quadriceps tendon.
 Bony fragments may be seen superior or inferior to the patella at/or near the tibial tubercle, indicating avulsion of the tendon.
Bony fragments may be seen superior or inferior to the patella at/or near the tibial tubercle, indicating avulsion of the tendon.
DIFFERENTIAL DIAGNOSIS
 Patella tendon rupture
Patella tendon rupture
 Quadriceps tendon rupture
Quadriceps tendon rupture
 Patellar fracture
Patellar fracture
 Patellar contusion
Patellar contusion
 Patellar tendonitis
Patellar tendonitis
 Prepatellar bursitis
Prepatellar bursitis
NONOPERATIVE MANAGEMENT
 Nonoperative management of extensor mechanism disruption is uncommon.
Nonoperative management of extensor mechanism disruption is uncommon.
 For the rare person with partial tendon rupture where active extension is preserved, consideration for cast or brace immobilization in full extension for 8 to 10 weeks followed by physical therapy to regain motion. Progress should be slow; regaining functional range of motion (ROM) should be the primary goal after immobilization. Strengthening exercises should be delayed for 3 months.
For the rare person with partial tendon rupture where active extension is preserved, consideration for cast or brace immobilization in full extension for 8 to 10 weeks followed by physical therapy to regain motion. Progress should be slow; regaining functional range of motion (ROM) should be the primary goal after immobilization. Strengthening exercises should be delayed for 3 months.
 Contraindications for surgical reconstruction include the following:
Contraindications for surgical reconstruction include the following:
Active infection
Inability to comply with postoperative immobilization and the physical therapy program
SURGICAL MANAGEMENT
 A deficient extensor mechanism in patients with a TKA poses a very challenging problem.
A deficient extensor mechanism in patients with a TKA poses a very challenging problem.
 Direct suture or staple repair alone is often unsuccessful.
Direct suture or staple repair alone is often unsuccessful.
 Options for management of extensor mechanism disruption after TKA include direct repair with augmentation using autogenous hamstrings tendon (semitendinosus tendon), allograft Achilles tendon or whole quadriceps-patella-patellar tendon allograft, or a synthetic graft or mesh.
Options for management of extensor mechanism disruption after TKA include direct repair with augmentation using autogenous hamstrings tendon (semitendinosus tendon), allograft Achilles tendon or whole quadriceps-patella-patellar tendon allograft, or a synthetic graft or mesh.
 This chapter will describe the use of Achilles tendon allograft tissue in the reconstruction of complete disruption of the extensor mechanism after TKA. Calcaneal bone block may be used if allograft needs to be extended past the tibial attachment of the patella tendon, such as in avulsion injuries of the patella tendon.
This chapter will describe the use of Achilles tendon allograft tissue in the reconstruction of complete disruption of the extensor mechanism after TKA. Calcaneal bone block may be used if allograft needs to be extended past the tibial attachment of the patella tendon, such as in avulsion injuries of the patella tendon.
Preoperative Planning
 Initial evaluation of the patient should include the following:
Initial evaluation of the patient should include the following:
History
Physical examination
Radiographs
 Previous operative reports should be reviewed. The surgeon should be prepared to perform revision surgery of any of the components of the TKA, specifically to address malrotation or malalignment.
Previous operative reports should be reviewed. The surgeon should be prepared to perform revision surgery of any of the components of the TKA, specifically to address malrotation or malalignment.
 Make certain that optimal allograft tissue is available.
Make certain that optimal allograft tissue is available.
Fresh frozen allograft is preferable to freeze-dried allograft tissue.
The allograft should be inspected to ascertain it is of adequate size and quality.
A calcaneal bone segment of at least 3 cm attached to the patella tendon is preferred.
Positioning
 The patient is positioned supine on a radiolucent table.
The patient is positioned supine on a radiolucent table.
 A regular pneumatic tourniquet is used proximally around the thigh.
A regular pneumatic tourniquet is used proximally around the thigh.
Alternatively, a sterile tourniquet can be employed if there is concern for the proximal extent of the incision.
 The leg is prepared and draped in the standard, sterile fashion for joint replacement surgery.
The leg is prepared and draped in the standard, sterile fashion for joint replacement surgery.
 Fluoroscopic equipment is in the room with the technician in case imaging is necessary intraoperatively; for example, to aid in proximal tibial osteotomy, placement of fixation screws, judgment of joint line, and patellar height.
Fluoroscopic equipment is in the room with the technician in case imaging is necessary intraoperatively; for example, to aid in proximal tibial osteotomy, placement of fixation screws, judgment of joint line, and patellar height.
 The pneumatic tourniquet is inflated (usually to 250 to 300 mm Hg) after the limb has been exsanguinated with an Esmarch bandage.
The pneumatic tourniquet is inflated (usually to 250 to 300 mm Hg) after the limb has been exsanguinated with an Esmarch bandage.
Approach
 The previous incision should be used. In cases with more than one incision, the most midline (extensile) incision should be chosen (FIG 2).
The previous incision should be used. In cases with more than one incision, the most midline (extensile) incision should be chosen (FIG 2).

 The dissection is carried down the midline, elevating medial and lateral skin and subcutaneous flaps.
The dissection is carried down the midline, elevating medial and lateral skin and subcutaneous flaps.
 The extensor mechanism and retinacular tissue is exposed. Often, the incision is extended proximally and distally to expose normal tissue.
The extensor mechanism and retinacular tissue is exposed. Often, the incision is extended proximally and distally to expose normal tissue.
 The tendon rupture is exposed and identified (FIG 3).
The tendon rupture is exposed and identified (FIG 3).
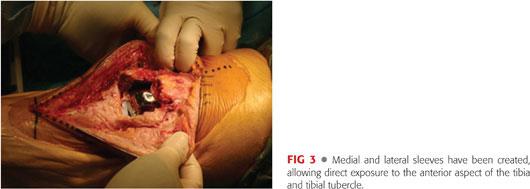
 To aid in dissection, a medial peripatellar approach can be incorporated for better exposure or access to the joint.
To aid in dissection, a medial peripatellar approach can be incorporated for better exposure or access to the joint.
 The joint is drained of any hematoma and irrigated using pulsatile lavage.
The joint is drained of any hematoma and irrigated using pulsatile lavage.
TECHNIQUES
 Primary Repair
Primary Repair
Primary repair of the ruptured tendon is always attempted.
In case of patella tendon rupture, two parallel drill holes are created longitudinally into the patella (TECH FIG 1A).
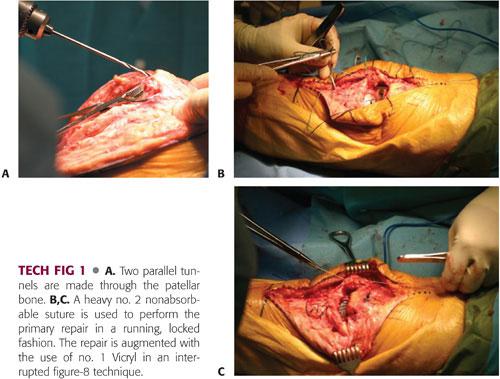
Use a no. 5 nonabsorbable suture (FiberWire [Arthrex, Naples, FL] or Ethibond) in a running, locked fashion into the remnant native tendon (TECH FIG 1B).
The suture is then passed into the drill holes and tied over bony bridge. The repair is performed with the knee in full extension (TECH FIG 1C).
The repair is augmented with no. 1 Vicryl to achieve end-to-end repair as best as possible.
 Preparation of the Tibia and Allograft
Preparation of the Tibia and Allograft
A small oscillating saw is used to make a rectangular cavity 2.5 × 1.5 × 1 cm in the proximal tibia slightly distal to the insertion of the patella tendon. Care should be taken to prevent iatrogenic fracture of the proximal tibia (TECH FIG 2A–C).
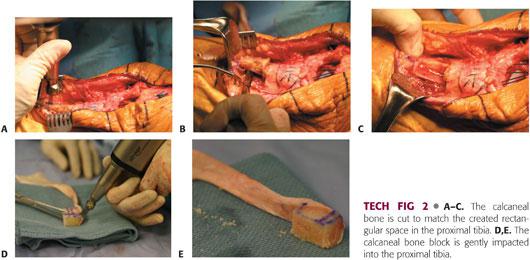
The allograft tendon is thawed and soaked in antibiotic-impregnated saline.
The allograft calcaneal bone is contoured to the desired shape on the back table. The goal is to form a trapezoidal bone block that will be press-fit into the tibial osteotomy site. Tight fit is preferred to get good bony stability and bone contact (TECH FIG 2D,E).
 Reduction and Fixation of Calcaneal Bone Block
Reduction and Fixation of Calcaneal Bone Block
The calcaneal bone block is gently impacted into the proximal tibia (TECH FIG 3A).
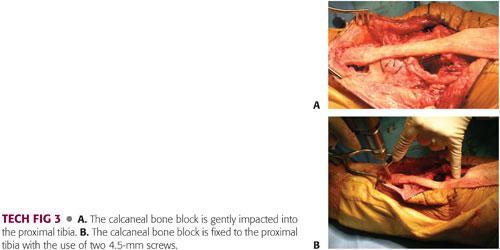
Two 3.5-mm screws, angled to avoid the tibial component, are used to secure the bone block to the tibia (TECH FIG 3B).
 Placement and Fixation of the Allograft Tendon
Placement and Fixation of the Allograft Tendon
The Achilles tendon is draped over the anterior tibia and patella while the knee is in full extension.
Tension is applied to the graft to keep it taut.
There is often excess allograft tendon. This proximal portion is trimmed to size and used to reinforce the reconstruction (TECH FIG 4A).
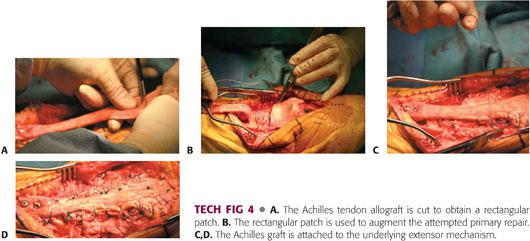
This excess patch of allograft is used to reinforce the repair at the rupture site (TECH FIG 4B).
The Achilles graft is attached to the underlying native extensor tissue using no. 1 and no. 2 nonabsorbable sutures (Ethibond or FiberWire) (TECH FIG 4C,D).
Care must be taken to keep graft under tension during the repair. Likewise, the knee is kept in full extension during the reconstruction.
 Wound Closure
Wound Closure
The subcutaneous flap is closed in the routine fashion using a combination of no. 1 Vicryl and 2-0 Vicryl sutures.
The skin is closed using skin staples, and a compression dressing is applied. The tourniquet is deflated after dressing is applied.
A knee immobilizer is applied to keep the knee in full extension.
PEARLS AND PITFALLS | |
Indications |
|
Graft |
|
| |
Reconstruction |
|
| |
| |
Revision of total knee comparison |
|
Postoperative care |
|
| |
| |
Failure |
|
| |
POSTOPERATIVE CARE
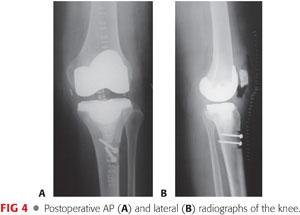
 Postoperative AP and lateral radiographs are obtained in the postoperative care unit (FIG 4).
Postoperative AP and lateral radiographs are obtained in the postoperative care unit (FIG 4).
 The knee is immobilized in full extension for 8 to 10 weeks using a hinged knee brace.
The knee is immobilized in full extension for 8 to 10 weeks using a hinged knee brace.
 Staples are removed 3 weeks postoperatively.
Staples are removed 3 weeks postoperatively.
 At 8 to 10 weeks, a brace with 30 degrees of flexion is used for 2 weeks and progressed to 60 degrees for an additional 2 weeks.
At 8 to 10 weeks, a brace with 30 degrees of flexion is used for 2 weeks and progressed to 60 degrees for an additional 2 weeks.
 Flexion past 90 degrees is delayed until 14 to 16 weeks postoperatively.
Flexion past 90 degrees is delayed until 14 to 16 weeks postoperatively.
OUTCOMES
 Short-term results are encouraging, but residual extensor lags of 5 to 20 degrees are common.2,4
Short-term results are encouraging, but residual extensor lags of 5 to 20 degrees are common.2,4
 The patient is encouraged to stay in the brace for 8 to 10 weeks postoperatively. Prolonged immobilization decreases the risk of extensor lag postoperatively.
The patient is encouraged to stay in the brace for 8 to 10 weeks postoperatively. Prolonged immobilization decreases the risk of extensor lag postoperatively.
 Longer term follow-up of patients with Achilles tendon reconstruction for extensor mechanism disruption is required.
Longer term follow-up of patients with Achilles tendon reconstruction for extensor mechanism disruption is required.
COMPLICATIONS
 Graft failure
Graft failure
 Infection
Infection
REFERENCES
1. Cadambi A, Engh GA. Use of a semitendinosus tendon autogenous graft for rupture of the patellar ligament after total knee arthroplasty: a report of seven cases. J Bone Joint Surg Am 1992;74(7):974–979.
2. Crossett LS, Sinha RK, Sechriest VF, et al. Reconstruction of a ruptured patellar tendon with Achilles tendon allograft following total knee arthroplasty. J Bone Joint Surg Am 2002;84(8):1354–1361.
3. Lynch AF, Rorabeck CH, Bourne RB. Extensor mechanism complications following total knee arthroplasty. J Arthroplasty 1987;2:135–140.
4. Rand JA. Extensor mechanism complications after total knee arthroplasty. Instr Course Lect 2005;54:241–250.
< div class='tao-gold-member'>















