Obtaining adequate anterior exposure of the knee can be difficult using standard approaches during revision total knee arthroplasty (TKA).
 The options available for dealing with difficult exposure include quadriceps snip (done 5 to 8 cm proximal to the superior pole of the patella), V-Y quadriceps turndown, and tibial tubercle osteotomy.
The options available for dealing with difficult exposure include quadriceps snip (done 5 to 8 cm proximal to the superior pole of the patella), V-Y quadriceps turndown, and tibial tubercle osteotomy.
 Tibial tubercle osteotomy is performed to obtain an extensile exposure of the knee during difficult revision TKA.
Tibial tubercle osteotomy is performed to obtain an extensile exposure of the knee during difficult revision TKA.
 An osteoperiosteal segment—which includes the tibial tubercle and upper tibial crest—is elevated to relax the extensor mechanism and allow safe subluxation of the patella.
An osteoperiosteal segment—which includes the tibial tubercle and upper tibial crest—is elevated to relax the extensor mechanism and allow safe subluxation of the patella.
 The technique was first described by Dolin6 in 1983 but subsequently was modified and popularized for exposure in revision TKA by Whiteside.10
The technique was first described by Dolin6 in 1983 but subsequently was modified and popularized for exposure in revision TKA by Whiteside.10
ANATOMY
 The extensor mechanism consists of the quadriceps muscles (ie, rectus femoris, vastus lateralis, vastus medialis, and vastus lateralis), quadriceps tendon, patella, and patellar tendon.
The extensor mechanism consists of the quadriceps muscles (ie, rectus femoris, vastus lateralis, vastus medialis, and vastus lateralis), quadriceps tendon, patella, and patellar tendon.
 The quadriceps muscle inserts into the patella via the quadriceps tendon and then into the tibial tuberosity via the patellar tendon.
The quadriceps muscle inserts into the patella via the quadriceps tendon and then into the tibial tuberosity via the patellar tendon.
 Tendinous fibers of the vastus medialis and vastus lateralis form the medial and lateral patellar retinaculae, respectively, which together reinforce the capsule of the knee joint anteriorly (FIG 1A).
Tendinous fibers of the vastus medialis and vastus lateralis form the medial and lateral patellar retinaculae, respectively, which together reinforce the capsule of the knee joint anteriorly (FIG 1A).
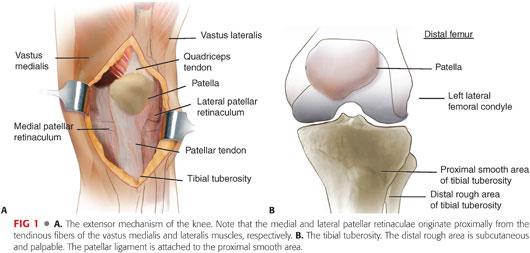
 The tibial tuberosity forms the truncated apex of a triangular area at the proximal end of the tibia. It has a distal “rough” area, which is subcutaneous and palpable, and a proximal “smooth” area attached to the patellar ligament (FIG 1B).
The tibial tuberosity forms the truncated apex of a triangular area at the proximal end of the tibia. It has a distal “rough” area, which is subcutaneous and palpable, and a proximal “smooth” area attached to the patellar ligament (FIG 1B).
PATHOGENESIS
 Adequate anterior exposure of the distal femur and tibial plateau during revision TKA is crucial for gentle soft tissue handling, safe implant removal, recognition of bone defects, and correct placement of revision components.
Adequate anterior exposure of the distal femur and tibial plateau during revision TKA is crucial for gentle soft tissue handling, safe implant removal, recognition of bone defects, and correct placement of revision components.
 During revision TKA, adhesions and fibrosis within the extensor mechanism restrict subluxation of the patella and limit exposure.
During revision TKA, adhesions and fibrosis within the extensor mechanism restrict subluxation of the patella and limit exposure.
 A medial parapatellar arthrotomy, combined with intra-articular excision of the fibrous pseudocapsule, allows subluxation of the patella in most cases.
A medial parapatellar arthrotomy, combined with intra-articular excision of the fibrous pseudocapsule, allows subluxation of the patella in most cases.
 Inadequate exposure with continued forceful retraction of the extensor mechanism risks avulsion of the patellar ligament from the tibial tubercle.
Inadequate exposure with continued forceful retraction of the extensor mechanism risks avulsion of the patellar ligament from the tibial tubercle.
NATURAL HISTORY
 Avulsion of the patellar tendon is a serious complication during revision TKA because it results in prolonged immobilization, extensor lag, and a poor functional outcome.
Avulsion of the patellar tendon is a serious complication during revision TKA because it results in prolonged immobilization, extensor lag, and a poor functional outcome.
 To avoid this complication, an extensile exposure is required to relax the extensor mechanism and allow safe eversion of the patella.
To avoid this complication, an extensile exposure is required to relax the extensor mechanism and allow safe eversion of the patella.
 Three options for obtaining such an extensile exposure during revision TKA are quadriceps snip, V-Y quadriceps turndown, and tibial tubercle osteotomy.
Three options for obtaining such an extensile exposure during revision TKA are quadriceps snip, V-Y quadriceps turndown, and tibial tubercle osteotomy.
 Tibial tubercle osteotomy is preferred to a V-Y quadriceps turndown because it has a lower incidence of extensor lag and quadriceps weakness.1,7
Tibial tubercle osteotomy is preferred to a V-Y quadriceps turndown because it has a lower incidence of extensor lag and quadriceps weakness.1,7
PATIENT HISTORY AND PHYSICAL FINDINGS
 A history of joint stiffness and complications after primary TKA (eg, arthrofibrosis, infection, hematoma) should alert the surgeon regarding potential difficulties with exposure during revision TKA.
A history of joint stiffness and complications after primary TKA (eg, arthrofibrosis, infection, hematoma) should alert the surgeon regarding potential difficulties with exposure during revision TKA.
 Physical findings indicating possible difficulty with exposure during revision TKA include multiple scars, reduced active and passive knee range of movement, a tight posterior cruciate ligament, and patella baja.
Physical findings indicating possible difficulty with exposure during revision TKA include multiple scars, reduced active and passive knee range of movement, a tight posterior cruciate ligament, and patella baja.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Standing anteroposterior and lateral radiographs of the knee usually are adequate in planning for extensile exposures during revision TKA.
Standing anteroposterior and lateral radiographs of the knee usually are adequate in planning for extensile exposures during revision TKA.
 The radiographs are specifically inspected for tibial osteopenia (especially around the tibial tuberosity) and osteolysis, both of which are relative contraindications for tibial tubercle osteotomy.
The radiographs are specifically inspected for tibial osteopenia (especially around the tibial tuberosity) and osteolysis, both of which are relative contraindications for tibial tubercle osteotomy.
SURGICAL MANAGEMENT
 A tibial tubercle osteotomy is indicated when there is any concern regarding patellar tendon avulsion despite adequate initial soft tissue release, as discussed later in this chapter.
A tibial tubercle osteotomy is indicated when there is any concern regarding patellar tendon avulsion despite adequate initial soft tissue release, as discussed later in this chapter.
Preoperative Planning
 Exposure should be thought about preoperatively: The history and physical findings should alert the surgeon regarding the potential need for extensile exposures during revision TKA.
Exposure should be thought about preoperatively: The history and physical findings should alert the surgeon regarding the potential need for extensile exposures during revision TKA.
 Previous operative records and radiographs are studied to identify the initial approach during primary TKA, design of the implanted components to be removed, and potential problems during implant removal.
Previous operative records and radiographs are studied to identify the initial approach during primary TKA, design of the implanted components to be removed, and potential problems during implant removal.
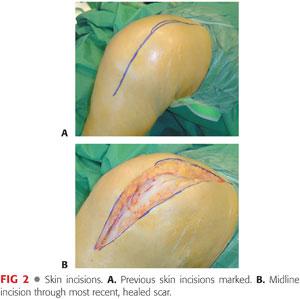
 The quality of skin overlying the tibial tubercle should be assessed. In patients with multiple scars, the most recent, appropriate, healed scar is used, but in many situations where tibial tubercle osteotomy is indicated, it may be necessary to consult with a plastic surgical team to plan soft tissue coverage (FIG 2).
The quality of skin overlying the tibial tubercle should be assessed. In patients with multiple scars, the most recent, appropriate, healed scar is used, but in many situations where tibial tubercle osteotomy is indicated, it may be necessary to consult with a plastic surgical team to plan soft tissue coverage (FIG 2).
Positioning
 The patient is positioned supine on the operating table.
The patient is positioned supine on the operating table.
 A tourniquet is sited around the upper thigh, and the leg is exsanguinated before inflation.
A tourniquet is sited around the upper thigh, and the leg is exsanguinated before inflation.
Approach
 A medial parapatellar approach is used whenever possible because extensile exposures are most easily incorporated proximally (V-Y quadriceps turndown) and distally (tibial tubercle osteotomy).
A medial parapatellar approach is used whenever possible because extensile exposures are most easily incorporated proximally (V-Y quadriceps turndown) and distally (tibial tubercle osteotomy).
TECHNIQUES
 Initial Soft Tissue Release Before Tibial Tubercle Osteotomy
Initial Soft Tissue Release Before Tibial Tubercle Osteotomy
If the patella cannot be everted following medial parapatellar arthrotomy, the following soft tissue releases are performed sequentially before considering a tibial tubercle osteotomy.
Medial release: The dissection is carried medially around the proximal tibia with subperiosteal elevation of the medial retinaculum and deep medial collateral ligament around to the semimembranosus insertion (TECH FIG 1A,B). This allows external rotation of the tibia and relaxes the extensor mechanism (TECH FIG 1C,D).
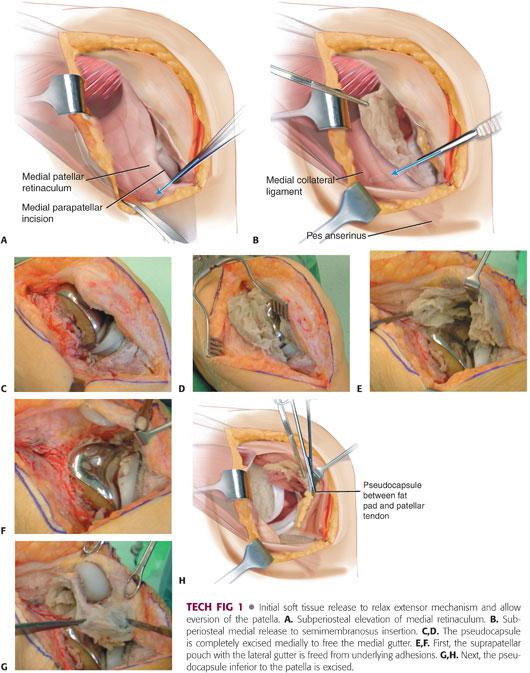
Lateral gutter release and pseudocapsule excision
• Superior to the patella, the suprapatellar pouch is freed by dividing the underlying adhesions tethering the extensor mechanism to the anterior femur (TECH FIG 1E).
• Lateral to the patella, adhesions in the lateral gutter tethering the extensor mechanism are divided (TECH FIG 1F).
• Inferior to the patella, the interval between the patellar tendon anteriorly and fat pad posteriorly is identified and the intervening pseudocapsule excised distally to the insertion of the patellar tendon (TECH FIG 1G,H). The interval between the posterior patellar tendon and the tibia should be freed of scar and adhesions.
If the patella still cannot be retracted appropriately, a tibial tubercle osteotomy is performed to reduce the risk of patellar tendon avulsion from forceful retraction of the extensor mechanism.
 Tibial Tubercle Osteotomy
Tibial Tubercle Osteotomy
The skin incision is extended 8 to 10 cm below the tibial tubercle.
The periosteum is vertically incised 1 cm medial to the tibial tubercle.
An osteotomy site measuring 6 cm long, 2 cm wide, and 1 cm thick,5,7 which includes the tibial tubercle and anterior tibial crest, is marked with electrocautery (TECH FIG 2A,B).
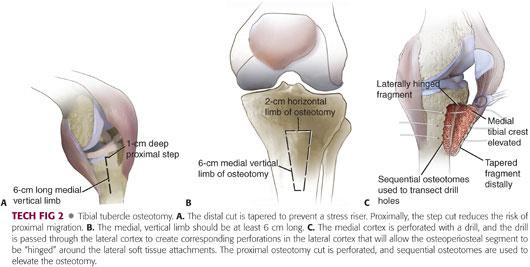
The 6-cm medial, vertical limb of the osteotomy is tapered distally to prevent a stress riser.
The 2-cm horizontal limb proximal to the insertion of the patellar tendon resists proximal migration of the osteotomized segment.
The proposed medial, lateral, and proximal osteotomy cuts are perforated using a drill (TECH FIG 2C).
Sequential osteotomes are used to transect the medial tibial crest and separate the osteotomized segment from the tibia.
The lateral cortex is transected through the osteotomy, but the lateral periosteum and soft tissues are left attached to the elevated segment to act as a “hinge,” allowing eversion of the extensor mechanism.
 Reattachment of Osteotomy with Wires
Reattachment of Osteotomy with Wires
In our preferred technique, three 18-gauge stainless steel wires are inserted and left untied before the final components are implanted.
The most proximal wire is passed through the osteotomized segment and through a drilled hole in the medial tibial cortex. Placement of a wire through the fragment prevents proximal migration.
The two distal wires are passed around the osteotomized segment and through drilled holes in the medial and lateral tibial cortices (TECH FIG 3).
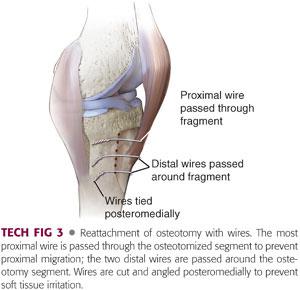
The wires are twisted until tight, cut, and angled 45 degrees posteromedially to prevent soft tissue irritation.10
 Reattachment of Osteotomy with Screws
Reattachment of Osteotomy with Screws
At least three cortical screws are inserted after implantation of the tibial component (TECH FIG 4).
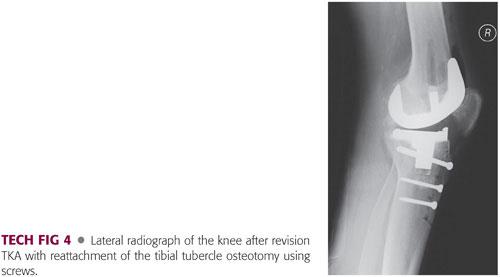
The screws are passed posteromedially and posterolaterally around the tibial component using the triangular cross-section of the proximal tibia.3,9
PEARLS AND PITFALLS | |
Indications |
|
| |
Initial exposure |
|
| |
Tibial tubercle osteotomy |
|
| |
| |
| |
Reattachment of osteotomy |
|
| |
POSTOPERATIVE CARE
 If fixation of the tibial tubercle osteotomy is adequate, weight bearing is permitted as tolerated with unrestricted range of movement in a hinged knee brace.
If fixation of the tibial tubercle osteotomy is adequate, weight bearing is permitted as tolerated with unrestricted range of movement in a hinged knee brace.
 If fixation is not adequate, the patient can bear weight as tolerated with the knee locked in full extension in a brace until there is radiologic evidence of union.
If fixation is not adequate, the patient can bear weight as tolerated with the knee locked in full extension in a brace until there is radiologic evidence of union.
OUTCOMES
 Whiteside10 reported good results using a tibial tubercle osteotomy to gain extensile exposure during 136 TKAs, of which 110 were revision procedures. At 2-year follow-up, the mean postoperative range of movement was 94 degrees, with a 1.5% incidence of extensor lag. Three tibial shaft fractures and two avulsions of the tibial tubercle were reported in this series but no nonunions.
Whiteside10 reported good results using a tibial tubercle osteotomy to gain extensile exposure during 136 TKAs, of which 110 were revision procedures. At 2-year follow-up, the mean postoperative range of movement was 94 degrees, with a 1.5% incidence of extensor lag. Three tibial shaft fractures and two avulsions of the tibial tubercle were reported in this series but no nonunions.
 Mendes et al8 reported 87% good-to-excellent results (based on the Knee Society Score [KSS]) in 64 patients in whom a tibial tubercle osteotomy was used for extensile exposure during revision TKA. At an average follow-up of 30 months, the mean postoperative range of movement was 107 degrees, with a 4.5% incidence of extensor lag. One fracture of the tibia, no tibial avulsions, and two nonunions of the osteotomy were reported in this series.
Mendes et al8 reported 87% good-to-excellent results (based on the Knee Society Score [KSS]) in 64 patients in whom a tibial tubercle osteotomy was used for extensile exposure during revision TKA. At an average follow-up of 30 months, the mean postoperative range of movement was 107 degrees, with a 4.5% incidence of extensor lag. One fracture of the tibia, no tibial avulsions, and two nonunions of the osteotomy were reported in this series.
 Barrack et al1 reported a significantly lower incidence of extensor lag following tibial tubercle osteotomy when compared to V-Y quadriceps turndown, although outcome scores were similar for both groups at the 4-year follow-up.
Barrack et al1 reported a significantly lower incidence of extensor lag following tibial tubercle osteotomy when compared to V-Y quadriceps turndown, although outcome scores were similar for both groups at the 4-year follow-up.
 Biomechanical studies show that although reattachment of an osteotomy with screws has greater fixation strength than cerclage wires, placement of screws around revision tibial component stems is difficult.3 Cerclage wires are easier to place and still provide solid fixation, especially when combined with a proximal step cut osteotomy.
Biomechanical studies show that although reattachment of an osteotomy with screws has greater fixation strength than cerclage wires, placement of screws around revision tibial component stems is difficult.3 Cerclage wires are easier to place and still provide solid fixation, especially when combined with a proximal step cut osteotomy.
 High rates of fixation failure with tibial tubercle osteotomy most likely are due to the use of small (<3 cm) osteoperiosteal fragments and failure to maintain lateral soft tissue attachments in continuity with the osteotomized segment.11
High rates of fixation failure with tibial tubercle osteotomy most likely are due to the use of small (<3 cm) osteoperiosteal fragments and failure to maintain lateral soft tissue attachments in continuity with the osteotomized segment.11
 Bruni et al2 prospectively randomized patients being treated with two-stage exchange to either receive a quadriceps snip or a tibial tubercle osteotomy. The tibial tubercle osteotomy group showed a higher mean KSS score and a higher mean maximal flexion and a lower incidence of extension lag than the quadriceps snip group.
Bruni et al2 prospectively randomized patients being treated with two-stage exchange to either receive a quadriceps snip or a tibial tubercle osteotomy. The tibial tubercle osteotomy group showed a higher mean KSS score and a higher mean maximal flexion and a lower incidence of extension lag than the quadriceps snip group.
 Choi et al4 has reported on the outcome of sequential repeated tibial tubercle osteotomy performed in two-stage revision in 13 patients and found satisfactory clinical and radiographic outcomes. However, there were three cases of proximal migration of the osteotomy fragment and one case of partial avulsion of the osteotomy fragment.
Choi et al4 has reported on the outcome of sequential repeated tibial tubercle osteotomy performed in two-stage revision in 13 patients and found satisfactory clinical and radiographic outcomes. However, there were three cases of proximal migration of the osteotomy fragment and one case of partial avulsion of the osteotomy fragment.
COMPLICATIONS
 Tibial tuberosity avulsion9,10
Tibial tuberosity avulsion9,10
 Nonunion of osteotomy8
Nonunion of osteotomy8
ACKNOWLEDGEMENT
The authors wish to gratefully acknowledge the contributions made by Drs. Anish K. Amin and James T. Patton, authors of the previous chapter. Their material is incorporated into this chapter.
REFERENCES
1. Barrack RL, Smith P, Munn B, et al. The Ranawat Award. Comparison of surgical approaches in total knee arthroplasty. Clin Orthop Relat Res 1998;356:16–21.
2. Bruni D, Iacono F, Sharma B, et al. Tibial tubercle osteotomy or quadriceps snip in two-stage revision for prosthetic knee infection? A randomized prospective study. Clin Orthop Relat Res 2013;471(4):1305–1318.
3. Caldwell PE, Bohlen BA, Owen JR, et al. Dynamic confirmation of fixation techniques of the tibial tubercle osteotomy. Clin Orthop Relat Res 2004;424:173–179.
4. Choi HR, Kwon YM, Burke DW, et al. The outcome of sequential repeated tibial tubercle osteotomy performed in 2-stage revision arthroplasty for infected total knee arthroplasty. J Arthroplasty 2012;27(8):1487–1491.
5. Clarke HD. Tibial tubercle osteotomy. J Knee Surg 2003;16:58–61.
6. Dolin MG. Osteotomy of the tibial tubercle in total knee replacement: a technical note. J Bone Joint Surg Am 1983;65A:704–706.
7. Kelly MA, Clarke HD. Stiffness and ankylosis in primary total knee arthroplasty. Clin Orthop Relat Res 2003;416:68–73.
8. Mendes MW, Caldwell P, Jiranek WA. The results of tibial tubercle osteotomy for revision total knee arthroplasty. J Arthroplasty 2004;19:167–174.
9. Ries MD, Richman JA. Extended tibial tubercle osteotomy in total knee arthroplasty. J Arthroplasty 1996;11:964–967.
10. Whiteside LA. Exposure in difficult total knee arthroplasty using tibial tubercle osteotomy. Clin Orthop Relat Res 1995;321:32–35.
11. Wolff AM, Hungerford DS, Krackow KA, et al. Osteotomy of the tibial tubercle during total knee replacement. J Bone Joint Surg Am 1989;71A:848–852.
< div class='tao-gold-member'>
















