Well-fixed femoral and acetabular components often must be removed during revision total hip arthroplasty (THA).
 Determine which well-fixed components should be removed and which should be left in place at the time of revision THA.
Determine which well-fixed components should be removed and which should be left in place at the time of revision THA.
ANATOMY
 Anatomic considerations during revision THA and the removal of well-fixed implants include pelvic landmarks as well as proximal femoral and diaphyseal landmarks.
Anatomic considerations during revision THA and the removal of well-fixed implants include pelvic landmarks as well as proximal femoral and diaphyseal landmarks.
The pelvic landmarks include the ischium, pubis, anterior and posterior acetabular columns, anterior inferior iliac spines, transverse acetabular ligament, sciatic notch, and acetabular walls.
The proximal femoral landmarks include the greater and lesser trochanters as well as the vastus ridge. These can be areas of relatively weak bone as a result of osteolysis, stress shielding, or previous surgery.
The femoral diaphyseal landmarks include the vastus ridge and linea aspera. These attachments for the vastus musculature must be reflected during an extended trochanteric osteotomy (ETO).
 The neurovascular structures at risk during revision THA and the removal of well-fixed implants include the sciatic, superior gluteal, and femoral nerves as well as the femoral vasculature.
The neurovascular structures at risk during revision THA and the removal of well-fixed implants include the sciatic, superior gluteal, and femoral nerves as well as the femoral vasculature.
 The sciatic nerve is at risk with the extensile posterior approach. The sciatic nerve can be identified in three distinct anatomic locations:
The sciatic nerve is at risk with the extensile posterior approach. The sciatic nerve can be identified in three distinct anatomic locations:
Exiting the sciatic notch deep to the piriformis muscle and superficial to the short external rotators (ie, superior gemellus, obturator internus, and inferior gemellus muscles)
Superficial to the ischium posterior and inferior to the posterior acetabular column superficial to the quadratus femoris muscle
Deep to the femoral insertion of the gluteus maximus tendon on the posterior femur
 The superior gluteal nerve is at risk during a transtrochanteric or extensile anterolateral approach. The superior gluteal nerve travels deep to the gluteus medius anteriorly along the ilium, approximately 4 to 5 cm proximal to the tip of the greater trochanter.
The superior gluteal nerve is at risk during a transtrochanteric or extensile anterolateral approach. The superior gluteal nerve travels deep to the gluteus medius anteriorly along the ilium, approximately 4 to 5 cm proximal to the tip of the greater trochanter.
 The femoral nerve is at risk with excessive anterior dissection and retraction as well as approaches to the hip that are medial to the anterior superior iliac spine (eg, extended iliofemoral).
The femoral nerve is at risk with excessive anterior dissection and retraction as well as approaches to the hip that are medial to the anterior superior iliac spine (eg, extended iliofemoral).
 The femoral vasculature is well anterior and usually protected by the iliopsoas muscle.
The femoral vasculature is well anterior and usually protected by the iliopsoas muscle.
PATHOGENESIS
 Conditions that necessitate the removal of well-fixed femoral or acetabular components include the following:
Conditions that necessitate the removal of well-fixed femoral or acetabular components include the following:
Infection
Recurrent dislocation (eg, malpositioned components)
Limb length discrepancy
Severe osteolysis
Polyethylene damage or wear
Acetabular locking mechanism failure
Component failure (eg, femoral stem fracture)
 Component removal with attention to bone preservation for subsequent reconstruction is critical.
Component removal with attention to bone preservation for subsequent reconstruction is critical.
NATURAL HISTORY
 Retention of well-fixed acetabular or femoral components has acceptable long-term performance during isolated component revision THA.2,16
Retention of well-fixed acetabular or femoral components has acceptable long-term performance during isolated component revision THA.2,16
PHYSICAL FINDINGS
 The physical examination of the patient undergoing revision THA includes the following:
The physical examination of the patient undergoing revision THA includes the following:
Gait pattern
Leg length discrepancy
Skin over the hip for previous scars
Muscle strength about the hip and leg
Distal neurovascular examination
IMAGING AND DIAGNOSTIC STUDIES
 Imaging studies identify which components are well fixed and evaluate the bone stock available for revision THA.
Imaging studies identify which components are well fixed and evaluate the bone stock available for revision THA.
Biplanar radiographs of the entire implant as well as the joint above and below the components are essential. These should include the entire cement mantle if a cemented femoral implant is being evaluated.
Oblique, or Judet, views of the pelvis may be useful to evaluate the anterior and posterior columns. Some acetabular defects cannot be recognized using routine anteroposterior (AP) pelvis radiograph.
Plain radiographs greatly underestimate the extent of osteolysis and available bone stock for revision THA. Some surgeons find computed tomographic (CT) scanning as a useful asset to guide the bone grafting of osteolytic lesions and to identify remaining bone stock for fixation.
Radiographic indicators of component stability include the following:
|
|
|
|
|
|
|
|
|
|
| |
|
Scintillography (ie, bone scan) is sensitive to implant loosening that may not be viewed on plain radiographs or at the time of surgery and may help the surgeon decide whether to retain or remove implants that appear well fixed. Scintillography is not specific for loosening and detects other metabolic, oncologic, and infectious processes.
 Serum diagnostic studies evaluate infection prior to revision THA.
Serum diagnostic studies evaluate infection prior to revision THA.
The combination of a normal erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) has a very high negative predictive value and indicate a very low (<1%) likelihood of infection.
Elevation of the ESR or CRP does not necessarily indicate infection but warrants an aspiration of the articulation with a manual cell count and differential as well as culture.
SURGICAL MANAGEMENT
Preoperative Planning
 The appropriate removal instruments and surgical approach are important considerations before revision THA with well-fixed implants.
The appropriate removal instruments and surgical approach are important considerations before revision THA with well-fixed implants.
 When performing revision THA with well-fixed implants, multiple options for the revision implant must be available to match the femoral and acetabular defect after extraction or discovered intraoperatively.
When performing revision THA with well-fixed implants, multiple options for the revision implant must be available to match the femoral and acetabular defect after extraction or discovered intraoperatively.
Positioning
 Patients can be positioned supine for the anterior or anterolateral approaches.
Patients can be positioned supine for the anterior or anterolateral approaches.
 Patients can be positioned in the lateral decubitus position for the anterolateral or posterior approaches.
Patients can be positioned in the lateral decubitus position for the anterolateral or posterior approaches.
TECHNIQUES
 Surgical Approach
Surgical Approach
Posterior (Also Known as Moore or Southern)
The patient is positioned in the lateral decubitus position, and the hip is exposed by splitting the iliotibial band and gluteus maximus muscle during the superficial dissection and reflecting the short external rotators and underlying hip capsule during the deep dissection. Deliberate repair of the posterior capsule and external rotators is required to reduce the incidence of dislocation after revision THA.
Anterolateral (Also Known as Watson-Jones or Hardinge)
The patient is positioned in the supine or lateral decubitus position, and the hip is exposed by splitting the iliotibial band and gluteus maximus muscle during the superficial dissection and reflecting the anterior third of the gluteus medius and minimus muscles with or without a portion of the vastus lateralis muscle during the deep dissection. This approach maintains the posterior attachments of the hip, which reduces the incidence of dislocation after revision THA.
Anterior (Also Known as Modified Smith-Petersen)
The patient is positioned in the supine position and the hip is exposed through the internervous plane between femoral and superior gluteal nerves, using the interval between the tensor fascia lata and the sartorius muscles during superficial dissection and the gluteus medius and rectus femoris muscles during deep dissection. This approach maintains the posterior attachments of the hip, which reduces the incidence of dislocation after revision THA.
 Osteotomy
Osteotomy
Extended Greater Trochanteric Osteotomy
The ETO is determined by the amount of prosthesis that is well fixed or the distal extent of the cement column that needs to be removed. This is rarely less than 12 cm from the tip of the greater trochanter. Approximately one-third of the lateral portion of the femoral cortical circumference is included in the ETO (TECH FIG 1A).
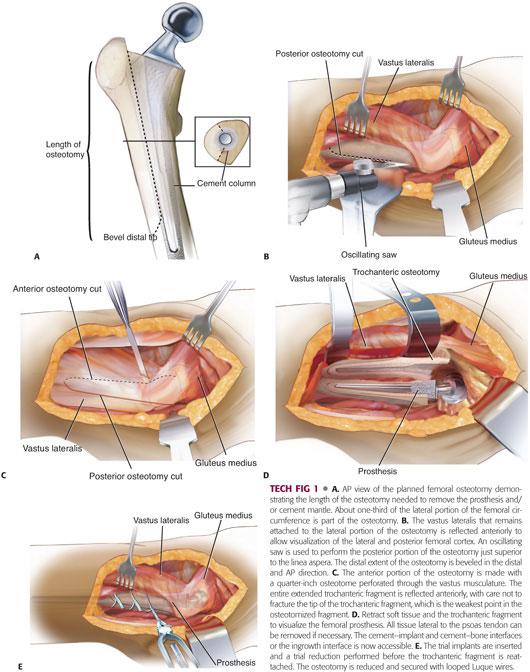
The vastus lateralis muscle remains attached to the lateral portion of the osteotomy at the vastus ridge, but distally, the vastus lateralis muscle is elevated off the linea aspera and retracted anteriorly to allow visualization of the lateral and posterior femoral cortex (TECH FIG 1B).
An oscillating saw is used to perform the posterior portion of the osteotomy just superior to the linea aspera (see TECH FIG 1B).
The distal extent of the osteotomy is beveled in the distal and AP direction. This portion of the osteotomy can be performed with a pencil-tipped high-speed burr (see TECH FIG 1B).
The distal extent of the anterior portion of the osteotomy is made with an oscillating saw or small half-inch osteotome.
The proximal extent of the anterior portion of the osteotomy is made with a small quarter-inch osteotome perforated through the vastus musculature. Multiple perforations are made in the same plane to complete the osteotomy (TECH FIG 1C). Alternatively, the proximal extent of the anterior portion of the osteotomy can be completed with a controlled fracture of the remaining cortex.
The entire extended trochanteric fragment with the gluteus medius muscle remains attached to the greater trochanter, and the vastus lateralis muscle that remains attached to the vastus ridge is reflected anteriorly, with extreme care not to fracture the tip of the greater trochanteric fragment (TECH FIG 1D). The greater trochanter is the weakest point in the extended trochanteric fragment.
The capsule surrounding the prosthesis below the greater trochanter is released or excised and the “shoulder” of the prosthesis exposed.
Curved Bennett-type retractors are inserted distal to the osteotomy for soft tissue retraction, and the anterior arm Charnley-type hip retractor or curved Bennett-type retractor is used to carefully retract the trochanteric fragment anteriorly to expose the femoral prosthesis.
Anterior and medial capsular attachments are taken down to the level of the psoas tendon. All tissue lateral to the psoas tendon can be removed at this point if needed to allow visualization of the femoral component.
The surgeon now has access to the cement–implant, cement–bone, or bone–implant interfaces as needed for femoral component removal.
Access to the acetabulum is obtained after femoral component extraction or with anterior dislocation of the hip. Anterior dislocation prior to femoral component extraction is preferred to avoid iatrogenic fracture of the osteotomy or proximal femur.
Preparation of the acetabulum, if necessary, as well as the femoral canal for long-stem fully coated or fluted-tapered femoral implant insertion, is completed with flexible reamers and proximal tapered reamers.
The trial implants are inserted and a trial reduction performed with the trochanteric fragment not attached.
Prior to femoral component insertion, most surgeons choose to place a cable around the femur just distal to the osteotomy site to prevent iatrogenic femoral shaft fracture.
ETO fixation is performed after the final implant is inserted. Often, small amounts of trochanteric bone must be removed to facilitate appropriate osteotomy reduction and fixation with looped Luque wires or cables (TECH FIG 1E).
Transfemoral (Also Known as Wagner) Osteotomy
The length of the transfemoral osteotomy (TFO) is determined by the amount of prosthesis that is well fixed or the distal extent of the cement column that needs to be removed. The TFO is particularly useful in the setting of coronal fracture fragments or extensive proximal bone loss.
The femur is split at the level of the greater trochanter using a large osteotome. The gluteus medius and minimus as well as vastus lateralis muscles are split but remain attached to the anterior and posterior portions of the osteotomy (TECH FIG 2A).
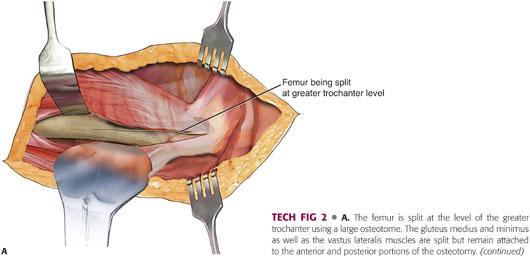
The distal extent of the osteotomy is completed by beveling the osteotomy anteriorly, posteriorly, or making a complete transfemoral cut booking open the proximal femur. This portion of the osteotomy can be performed with a pencil-tipped high-speed burr or oscillating saw (TECH FIG 2B).
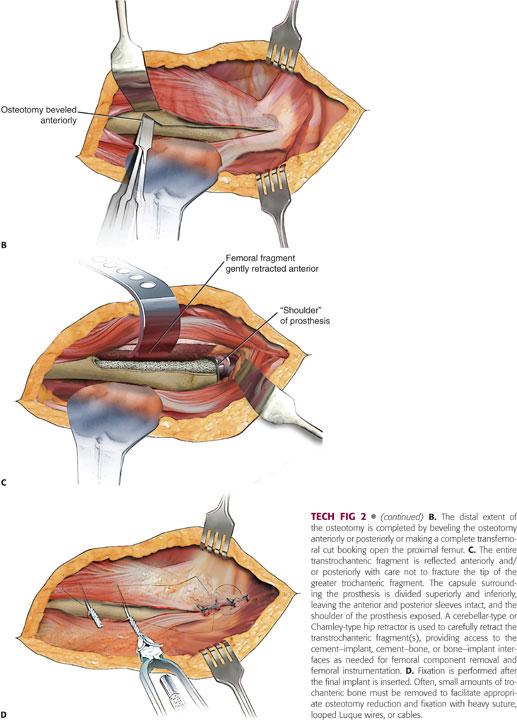
The entire transtrochanteric fragment is reflected anteriorly and/or posteriorly with extreme care not to fracture the tip of the greater trochanteric fragment (TECH FIG 2C). The greater trochanter is the weakest point in the transtrochanteric fragment.
The capsule surrounding the prosthesis is divided superiorly and inferiorly, leaving the anterior and posterior sleeves intact and the shoulder of the prosthesis exposed.
A cerebellar-type or Charnley-type hip retractor is used to carefully retract the transtrochanteric fragment(s) to expose the femoral prosthesis.
The surgeon now has access to the cement–implant, cement–bone, or bone–implant interfaces as needed for femoral component removal.
Access to the acetabulum is obtained after femoral component extraction or with anterior or posterior dislocation of the hip. Dislocation prior to femoral component extraction is preferred to avoid iatrogenic fracture of the osteotomy or distal femur.
Preparation of the acetabulum, if necessary, as well as the femoral canal for long-stem fully coated or fluted-tapered femoral implant insertion, is completed with flexible reamers and proximal tapered reamers.
The trial implants are inserted and a trial reduction performed with the transtrochanteric fragment(s) not attached.
Prior to femoral component insertion, most surgeons choose to place a cable around the femur just distal to the osteotomy site to prevent iatrogenic femoral shaft fracture.
TFO fixation is performed after the final implant is inserted. Often, small amounts of trochanteric bone must be removed to facilitate appropriate osteotomy reduction and fixation with heavy suture, looped Luque wires, or cables (TECH FIG 2D).
 Cortical Window
Cortical Window
The length of the cortical window is determined by the amount of prosthesis that is well fixed or the distal extent of the cement column that needs to be removed. Up to one-third of the lateral portion of the femoral cortical circumference may be included in a cortical window.
As in the ETO, the vastus lateralis muscle remains attached to the lateral portion of the osteotomy at the vastus ridge, but distally, the vastus lateralis muscle is elevated off the linea aspera and retracted anteriorly to allow visualization of the lateral and posterior femoral cortex.
Drill holes are made at the corner of the window to reduce any potential stress-risers that could lead to iatrogenic femur fracture.
The drill holes are connected via osteotome or oscillating saw.
The surgeon may remove the cortical window with an osteotomy and gain limited access to the cement–implant, cement–bone, or bone–implant interfaces as needed for femoral component removal. A carbide punch can be used to extract components in a retrograde fashion.
The cortical window is temporarily held into position with Farabeuf clamps during trialing and final component placement.
Fixation is performed after the final implant is inserted with looped Luque wires.
 Implant Removal
Implant Removal
Femoral Extraction
Most well-fixed femoral components require a femoral osteotomy for safe extraction. A femoral osteotomy offers several advantages during the removal of a well-fixed femoral component:
Preservation of bone stock and soft tissue attachments
Exposure of the femoral canal for reconstruction
Deformity correction
Soft tissue balance
Bone grafting
Increased union rate when compared to an iatrogenic fracture
Decreased operating time
Distal cement removal
Fracture planes may be used to gain access to well-fixed or loose femoral components in lieu of a femoral osteotomy or cortical window.
To make the subsequent reconstruction straightforward, care should be taken to prevent femoral cortical penetration and preserve as much bone stock as possible during femoral component extraction. Intraoperative fluoroscopy may be useful to prevent a cortical breach.
Cemented femoral stems are disimpacted from their cement mantle after clearing the medial collar and lateral shoulder of the prosthesis as well as medial greater trochanteric overhang with a high-speed burr. The use of osteotomes should be avoided at this phase. Osteotomes increase hoop stresses and may heighten the risk of iatrogenic greater trochanter fracture. An implant-specific or universal extractor is applied to the neck of the cemented stem. The stem is disimpacted from its cement mantle with three to five firm but controlled blows with a slap hammer. If the femoral component does not have a lipped taper, it may be necessary to notch the inferior aspect with a diamond-cutting wheel to allow proper grasping of the femoral prosthesis for extraction. If the cemented stem is not easily disimpacted, consider performing an ETO and removal similar to an uncemented femoral stem (see in the following text) or free up the proximal cement mantle with a pencil-tipped high-speed burr or flexible osteotomes. If the cement mantle is to be removed, this may be accomplished with a combination of manual cement removal instruments (eg, splitter, V osteotome, T osteotome, reverse hook, or pituitary rongeur), motorized osteotomes, pencil-tipped high-speed burr to create fault lines and control cement fracture, round high-speed burr for metaphyseal cement, drill, and orthopaedic ultrasonic cement removal system (eg, OSCAR, Orthosonics, Chatham, NJ). The distal cement plug may be removed in a retrograde fashion, especially if loose, through a cortical window or in antegrade fashion by making a central hole in the distal cement with a drill, burr, or ultrasonic device and using a reverse hook to extract the distal cement. If the distal cement is distal to the isthmus of the femur, a cortical window or ETO should be considered. If the cement mantle is to be retained, the well-fixed, noninfected cement mantle can be contoured and texturized with a burr or ultrasonic device to create space for a new femoral component that is cemented into the existing cement mantel (ie, cement-in-cement technique).12
Proximally, porous-coated uncemented femoral stems are disimpacted from the bone after clearing the medial collar and lateral shoulder of the prosthesis as well as medial greater trochanteric overhang with a high-speed burr. The bone–implant interface is disrupted with a pencil-tipped burr, flexible osteotomes, motorized osteotomes, and a U osteotome for the medial calcar. If the medial calcar is blocked by a collar, a metal-cutting burr is used to remove the collar and gain access to the calcar. Care should be taken, as osteotomes increase hoop stresses and may increase the risk of iatrogenic greater trochanter fracture. An implant-specific or universal extractor is applied to the neck of the cemented stem. The stem is disimpacted from its cement mantle with three to five firm but controlled blows with a slap hammer. If the femoral component does not have a lipped taper, it may be necessary to notch the inferior aspect of the femoral neck with a diamond-cutting wheel to allow proper grasping of the femoral prosthesis for extraction. If the proximally porous uncemented stem is not easily disimpacted, consider performing an ETO.
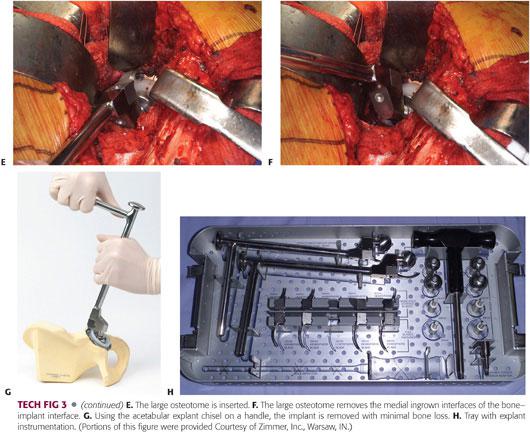
Fully porous-coated uncemented femoral stems require a femoral osteotomy for extraction (TECH FIG 3A). After the femoral osteotomy, if the implant is not fractured, the implant can be cut with a metal-cutting high-speed burr at the distal extent of the femoral osteotomy (TECH FIG 3B). The distal portion of the remaining implant should be cylindrical. A Gigli saw is passed along the proximal portion of the implant along the calcar, removing any proximal medial fixation (TECH FIG 3C). An appropriately sized trephine is used in conjunction with copious irrigation to remove the remaining distal portion of the well-fixed, fully porous-coated femoral implant (TECH FIG 3D). Multiple trephines, a minimum of four to six that are one size above and one size below the expected implant size, should be available, as trephines dull quickly and implant sizes are dictated incorrectly. Flexible osteotomes and a pencil-tipped high-speed burr should also be available.
Acetabular Extraction
Removal of a well-fixed acetabular component may be done from any approach to the hip.
Care should be taken to preserve as much acetabular bone stock as possible during acetabular component extraction for subsequent reconstruction. Aggressively twisting or pulling a well-fixed component is seldom required and can lead to unintended major bone loss.
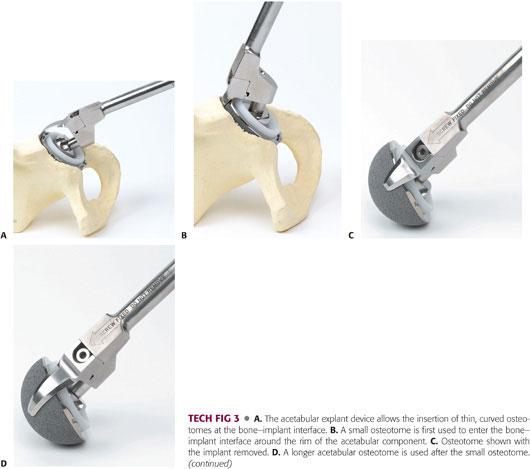
An acetabular osteotome (Explant Acetabular Removal System, Zimmer Inc, Warsaw, IN) is designed to rotate short- and long-curved chisels at a fixed radius, corresponding to the size of the acetabular component, and disrupt the bone–implant interface to facilitate acetabular component removal (TECH FIG 4A–D). All screws should be removed with the appropriate driver or screw removal system prior to using the explant osteotome. The original liner, a trial liner, or bipolar head can be reinserted to center the acetabular osteotome and remove the acetabular component.
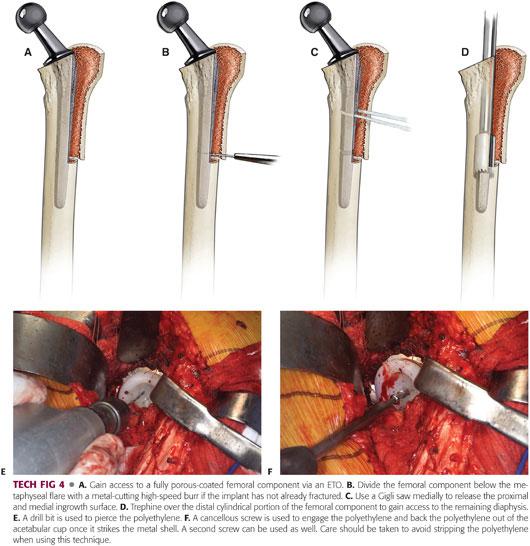
Removal of a well-fixed acetabular liner may be done from any approach to the hip. If the liner is ceramic or metal, the appropriate implant-specific extraction tool must be available. If the liner is polyethylene and cemented into the pelvis or acetabular component, it may be removed by reaming the polyethylene back to the cement mantle and extracting the cement if necessary with osteotomes, a high-speed burr, and/or an orthopaedic cement removal system. If the liner is polyethylene and locked into an acetabular component, it may be removed with the appropriate implant-specific extraction tool, a one- or two-screw technique (TECH FIG 4E,F), or in fragments with reamers, osteotomes, and/or high-speed burr.
PEARLS AND PITFALLS | |
Acetabular deficiencies |
|
ETO |
|
| |
| |
| |
| |
| |
| |
| |
Femoral component removal |
|
Acetabular component removal |
|
| |
| |
POSTOPERATIVE CARE
 Weight-bearing status is determined by a combination of bone quality, initial implant stability against that bone, and whether an osteotomy was used for exposure.
Weight-bearing status is determined by a combination of bone quality, initial implant stability against that bone, and whether an osteotomy was used for exposure.
 Weight bearing as tolerated can typically begin after isolated head and liner exchange with the retention of osseointegrated components.
Weight bearing as tolerated can typically begin after isolated head and liner exchange with the retention of osseointegrated components.
 Weight bearing is often restricted to 50% for 8 weeks with the use of a two-handed ambulatory assistive device if an extended osteotomy was done, if an implant was reinserted into relatively poor bone, and/or bone graft was used.
Weight bearing is often restricted to 50% for 8 weeks with the use of a two-handed ambulatory assistive device if an extended osteotomy was done, if an implant was reinserted into relatively poor bone, and/or bone graft was used.
Weight bearing is occasionally restricted to toe-touch for 8 weeks or more after major reconstructive procedures in which the bone loss was extensive or the fixation obtained is judged to be at risk.
 When an implant is removed for infection and an antibiotic-impregnated articulated or static spacer is inserted, weight-bearing status is again based on the bone quality, implant stability, and need for an osteotomy and is often, but not always, restricted with an ambulatory assistive device used until replantation.
When an implant is removed for infection and an antibiotic-impregnated articulated or static spacer is inserted, weight-bearing status is again based on the bone quality, implant stability, and need for an osteotomy and is often, but not always, restricted with an ambulatory assistive device used until replantation.
COMPLICATIONS
 Femoral fractures are common near the trochanteric region and in the femoral diaphysis during removal of well-fixed femoral implants.
Femoral fractures are common near the trochanteric region and in the femoral diaphysis during removal of well-fixed femoral implants.
 Nonunion can occur in the setting of ETO and TFO.
Nonunion can occur in the setting of ETO and TFO.
 Revision THA has a higher dislocation rate than primary THA.
Revision THA has a higher dislocation rate than primary THA.
 A tight diaphyseal fit is essential to prevent implant subsidence.
A tight diaphyseal fit is essential to prevent implant subsidence.
 Acetabular deficiencies may be extensive in the face of polyethylene wear and osteolysis.
Acetabular deficiencies may be extensive in the face of polyethylene wear and osteolysis.
OUTCOMES
 Short-term follow-up after ETO for revision THA1,5,9,13–15,17:
Short-term follow-up after ETO for revision THA1,5,9,13–15,17:
Osteotomy union rate: 97.8% to 100%
Greater trochanter fracture rate: 2.4% to 23.1%
Diaphyseal femoral fracture rate: 0.0% to 20.0%
Rate of implant subsidence: 1.4% to 23.0%
Dislocation rate: 7.1% to 30.8%
 Short-term follow-up after TFO for revision THA3,4,6–8,10,11,18–20:
Short-term follow-up after TFO for revision THA3,4,6–8,10,11,18–20:
Osteotomy union rate: 83.3% to 98.5%
Greater trochanter fracture rate: 60%
Diaphyseal femoral fracture rate: 0.0% to 17.6%
Rate of implant subsidence: 10.1% to 64.7%
Dislocation rate: 2.9% to 21.4%
REFERENCES
1. Aribindi R, Paprosky W, Nourbash P, et al. Extended proximal femoral osteotomy. Instr Course Lect 1999;48:19–26.
2. Berger RA, Quigley LR, Jacobs JJ, et al. The fate of stable cemented acetabular components retained during revision of a femoral component of a total hip arthroplasty. J Bone Joint Surg Am 1999;81:1682–1691.
3. Böhm P, Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am 2001;83-A(7):1023–1031.
4. Böhm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res 2004;(420):148–159.
5. Chen WM, McAuley JP, Engh CA Jr, et al. Extended slide trochanteric osteotomy for revision total hip arthroplasty. J Bone Joint Surg Am 2000;82:1215–1219.
6. Fink B, Grossmann A, Schubring S, et al. A modified transfemoral approach using modular cementless revision stems. Clin Orthop Relat Res 2007;462:105–114.
7. Grunig R, Morscher E, Ochsner PE. Three-to 7-year results with the uncemented SL femoral revision prosthesis. Arch Orthop Trauma Surg 1997;116:187–197.
8. Hartwig CH, Böhm P, Czech U, et al. The Wagner revision stem in alloarthroplasty of the hip. Arch Orthop Trauma Surg 1996;115:5–9.
9. Huffman GR, Ries MD. Combined vertical and horizontal cable fixation of an extended trochanteric osteotomy site. J Bone Joint Surg Am 2003;85-A(2):273–277.
10. Isacson J, Stark A, Wallensten R. The Wagner revision prosthesis consistently restores femoral bone structure. Int Orthop 2000;24:139–142.
11. Kolstad K, Adalberth G, Mallmin H, et al. The Wagner revision stem for severe osteolysis. 31 hips followed for 1.5-5 years. Acta Orthop Scand 1996;67:541–544.
12. Lieberman JR, Moeckel BH, Evans BG, et al. Cement-within-cement revision hip arthroplasty. J Bone Joint Surg Br 1993;75:869–871.
13. Mardones R, Gonzalez C, Cabanela ME, et al. Extended femoral osteotomy for revision of hip arthroplasty: results and complications. J Arthroplasty 2005;20:79–83.
14. Miner TM, Momberger NG, Chong D, et al. The extended trochanteric osteotomy in revision hip arthroplasty: a critical review of 166 cases at mean 3-year, 9-month follow-up. J Arthroplasty 2001;16:188–194.
15. Morshed S, Huffman GR, Ries MD. Extended trochanteric osteotomy for 2-stage revision of infected total hip arthroplasty. J Arthroplasty 2005;20:294–301.
16. Moskal JT, Shen FH, Brown TE. The fate of stable femoral components retained during isolated acetabular revision: a six-to-twelve-year follow-up study. J Bone Joint Surg Am 2002;84-A(2):250–255.
17. Peters PC Jr, Head WC, Emerson RH Jr. An extended trochanteric osteotomy for revision total hip replacement. J Bone Joint Surg Br 1993;75:158–159.
18. Wagner M, Wagner H. The transfemoral approach for revision of total hip replacement [in German]. Oper Orthop Traumatol 1999;11:278–295.
19. Warren PJ, Thompson P, Fletcher MD. Transfemoral implantation of the Wagner SL stem. The abolition of subsidence and enhancement of osteotomy union rate using Dall-Miles cables. Arch Orthop Trauma Surg 2002;122:557–560.
20. Wilkes RA, Birch J, Pearse MF, et al. The Wagner technique for revision arthroplasty of the hip: a review of 24 cases. J Orthop Rheumatol 1994;7:196–198.
< div class='tao-gold-member'>
















