Acetabular bone deficiency may occur primarily (eg, dysplasia, inflammatory arthritis, or seronegative arthropathy) or secondarily (eg, aseptic or septic loosening of acetabular components, osteolysis, trauma, or iatrogenic loss during removal of well-fixed components).
 The use of antiprotrusio cages is indicated in situations where an uncemented porous-coated acetabular component will not gain reliable initial stability.
The use of antiprotrusio cages is indicated in situations where an uncemented porous-coated acetabular component will not gain reliable initial stability.
ANATOMY
 The confluence of the ilium, the ischium, and the pubis forms the hemispherically shaped acetabulum, each contributing to the anterior and posterior walls and columns.
The confluence of the ilium, the ischium, and the pubis forms the hemispherically shaped acetabulum, each contributing to the anterior and posterior walls and columns.
 Surgical landmarks include the anterior and posterior walls, dome, and medial wall “teardrop.”
Surgical landmarks include the anterior and posterior walls, dome, and medial wall “teardrop.”
 The acetabulum is normally oriented with 45 degrees of inclination and 15 degrees of anteversion relative to the pelvic plane.
The acetabulum is normally oriented with 45 degrees of inclination and 15 degrees of anteversion relative to the pelvic plane.
PATHOGENESIS
 Acetabular bone deficiency may occur primarily due to dysplasia. This type of deficiency usually does not require the use of an antiprotrusio cage.
Acetabular bone deficiency may occur primarily due to dysplasia. This type of deficiency usually does not require the use of an antiprotrusio cage.
 Certain conditions (eg, rheumatoid arthritis, juvenile rheumatoid arthritis, ankylosing spondylitis, or Paget disease) may predispose patients to acetabular protrusio but usually do not require the use of an antiprotrusio cage.
Certain conditions (eg, rheumatoid arthritis, juvenile rheumatoid arthritis, ankylosing spondylitis, or Paget disease) may predispose patients to acetabular protrusio but usually do not require the use of an antiprotrusio cage.
 The antiprotrusio cage is used most often in cases of secondary bone stock deficiency so massive that the use of a cementless press-fit acetabular component is precluded.
The antiprotrusio cage is used most often in cases of secondary bone stock deficiency so massive that the use of a cementless press-fit acetabular component is precluded.
NATURAL HISTORY
 The natural history of massive acetabular bone defects that would require an antiprotrusio cage is not known. Patients usually require revision surgery to return to functional activities.
The natural history of massive acetabular bone defects that would require an antiprotrusio cage is not known. Patients usually require revision surgery to return to functional activities.
PATIENT HISTORY AND PHYSICAL FINDINGS
 The history should be conducted to determine whether the source of pain is extrinsic or intrinsic.
The history should be conducted to determine whether the source of pain is extrinsic or intrinsic.
 The patient’s pain may be extrinsic (eg, lumbar radiculopathy or intrapelvic pathology), in which case revision surgery may fail to relieve pain completely.
The patient’s pain may be extrinsic (eg, lumbar radiculopathy or intrapelvic pathology), in which case revision surgery may fail to relieve pain completely.
Pain usually, but not always, is located in the groin.
 Infection must always be assessed with careful questioning about previous infections, fevers, chills, wound drainage, and pain at rest.
Infection must always be assessed with careful questioning about previous infections, fevers, chills, wound drainage, and pain at rest.
 Start-up pain is an indication of loosening.
Start-up pain is an indication of loosening.
 Medical comorbidities must be assessed to determine the presence of any that may compromise the outcome of the surgery or place the patient at increased risk of complications.
Medical comorbidities must be assessed to determine the presence of any that may compromise the outcome of the surgery or place the patient at increased risk of complications.
 The skin should be inspected visually for placement of prior incisions and signs of infection.
The skin should be inspected visually for placement of prior incisions and signs of infection.
The appropriate incision for the surgical approach must be used with an adequate (6 cm) skin bridge.
IMAGING AND OTHER DIAGNOSTIC STUDIES
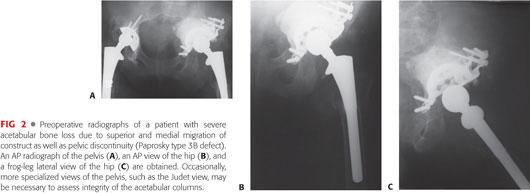
 Plain radiographs, including anteroposterior (AP) of the pelvis and AP and true lateral of the hip, should be obtained to classify bone loss and to adequately plan preoperatively (FIG 1).
Plain radiographs, including anteroposterior (AP) of the pelvis and AP and true lateral of the hip, should be obtained to classify bone loss and to adequately plan preoperatively (FIG 1).

 Computed tomography (CT) scans may be used to assess the remaining bone stock.
Computed tomography (CT) scans may be used to assess the remaining bone stock.
This is especially important in cases of superior or posterior bone loss that may require allograft reconstruction.
The CT scan can help determine the need to have allograft bone available to reconstruct the defect and may help dictate the approach if a posterior column reconstruction or plating is necessary.
 CT scans with intravascular contrast are useful in situations in which a prior implant is medial to Kohler line and proximity of the implant to the vessels and intra-abdominal contents is unknown.
CT scans with intravascular contrast are useful in situations in which a prior implant is medial to Kohler line and proximity of the implant to the vessels and intra-abdominal contents is unknown.
 Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are useful screening tools to detect infection.
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are useful screening tools to detect infection.
 Aspiration of the hip to assess for infection is valuable if the ESR, CRP, or clinical suspicion is elevated.
Aspiration of the hip to assess for infection is valuable if the ESR, CRP, or clinical suspicion is elevated.
 Nuclear medicine studies such as technetium 99 methylene diphosphonate in combination with gallium citrate, indium 111–labeled leukocyte scans, positron emission tomographic scans with 18Ffluorodeoxyglucose, and sulfur colloid scans may help differentiate aseptic from septic loosening.
Nuclear medicine studies such as technetium 99 methylene diphosphonate in combination with gallium citrate, indium 111–labeled leukocyte scans, positron emission tomographic scans with 18Ffluorodeoxyglucose, and sulfur colloid scans may help differentiate aseptic from septic loosening.
DIFFERENTIAL DIAGNOSIS
 The following conditions may contribute to pain and may be the cause of continued pain after the surgery:
The following conditions may contribute to pain and may be the cause of continued pain after the surgery:
Lumbar radiculopathy
Spinal stenosis
Sacroiliac degenerative joint disease
Intra-abdominal pathology
Intrapelvic pathology
Neuropathy
Meralgia paresthetica
Complex regional pain syndrome
Vascular claudication
Primary bone tumors
Metastasis
NONOPERATIVE MANAGEMENT
 Nonoperative management of severe acetabular bone loss is reserved for those patients in whom surgical management is contraindicated. This includes patients with substantial medical comorbidities and those with active infection.
Nonoperative management of severe acetabular bone loss is reserved for those patients in whom surgical management is contraindicated. This includes patients with substantial medical comorbidities and those with active infection.
SURGICAL MANAGEMENT
 Surgical management begins with preoperative planning.
Surgical management begins with preoperative planning.
 The radiographs are assessed and it is determined whether the defect can be reconstructed with a cementless acetabular component or will require an antiprotrusio cage.
The radiographs are assessed and it is determined whether the defect can be reconstructed with a cementless acetabular component or will require an antiprotrusio cage.
 The surgical approach is planned.
The surgical approach is planned.
If posterior column plating is anticipated, a posterior approach is indicated.
If this is not required, a direct lateral or posterior approach may be used, according to the surgeon’s preference.
 The acetabulum is exposed, bone loss is assessed, and determination about the appropriate reconstructive choice is made.
The acetabulum is exposed, bone loss is assessed, and determination about the appropriate reconstructive choice is made.
Preoperative Planning
 Planning for the antiprotrusio cage begins with appropriate radiographs.
Planning for the antiprotrusio cage begins with appropriate radiographs.
The radiographs allow for classification of the defect and aid in planning for the reconstruction.
 We have found the Paprosky classification to be helpful in defining bone deficiency and predicting the method of reconstruction3 (FIG 2).
We have found the Paprosky classification to be helpful in defining bone deficiency and predicting the method of reconstruction3 (FIG 2).
Paprosky type 1 acetabular defects have minimal bone loss and can usually be reconstructed using only a cementless component.
Type 2A defects have an intact superior rim and the acetabulum is oval in shape. The anterior and posterior columns are intact. The implant has migrated less than 2 cm. These defects may be reconstructed with so-called jumbo cups or cementless reconstruction with additional bone grafting or trabecular metal augments. The socket may also be placed in a more superior position to attain greater contact with host bone.
Type 2B defects are similar to type 2A defects, with the exception of loss of the superior rim. The implant has migrated less than 2 cm. The superior rim can be reconstructed with an uncemented socket in association with bone grafting or trabecular metal augments.
Type 2C defects involve medial bone loss with intact anterior and posterior columns. Medial bone loss may be reconstructed with bone graft or trabecular metal augments.
Type 3A defects generally migrate more than 2 cm superolaterally. The medial wall and ischium usually are still present but damaged. These defects can be reconstructed with bone grafting or trabecular metal augments and an uncemented socket.
Type 3B defects generally migrate more than 2 cm superomedially. There is loss of the teardrop and severe damage to the ischium. Pelvic discontinuity should be suspected. These defects can be reconstructed with bulk allograft, trabecular metal, an antiprotrusio cage, or a combination. Posterior column plating may be needed in cases of acute discontinuity. If this is a possibility, then a posterior approach should be selected.
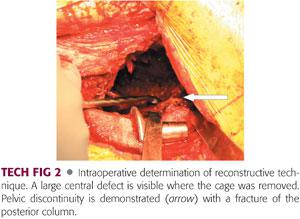
 Pelvic discontinuity should be suspected if a fracture is noted that involves both the anterior and posterior columns, the inferior hemipelvis has migrated medial to the superior hemipelvis, or the inferior hemipelvis is rotated in relation to the superior hemipelvis.
Pelvic discontinuity should be suspected if a fracture is noted that involves both the anterior and posterior columns, the inferior hemipelvis has migrated medial to the superior hemipelvis, or the inferior hemipelvis is rotated in relation to the superior hemipelvis.
 Large posterior column defects may predispose to cage failure and reconstruction of the defect should be included in preoperative planning.
Large posterior column defects may predispose to cage failure and reconstruction of the defect should be included in preoperative planning.
 An appropriate device should be selected.
An appropriate device should be selected.
The flanges should be malleable to allow the cage to be shaped to the bone.
The implant must have sufficient strength.
We believe that an inferior flange that gains fixation in or on the ischium is superior to a hook that gains fixation on the teardrop.
Positioning
 The patient is positioned according to surgeon preference and as dictated by the surgical approach. The hip should be draped to allow wide surgical exposure.
The patient is positioned according to surgeon preference and as dictated by the surgical approach. The hip should be draped to allow wide surgical exposure.
Approach
 The surgeon should select a posterior approach if he or she anticipates the need for posterior column plating or reconstruction. Otherwise, the surgeon should select the approach that is most familiar and comfortable.
The surgeon should select a posterior approach if he or she anticipates the need for posterior column plating or reconstruction. Otherwise, the surgeon should select the approach that is most familiar and comfortable.
 A trochanteric osteotomy, either conventional or extended, may improve exposure of the acetabulum and pelvis.
A trochanteric osteotomy, either conventional or extended, may improve exposure of the acetabulum and pelvis.
 Exposure of the sciatic nerve (posterior approach) is left to the judgment of the surgeon.
Exposure of the sciatic nerve (posterior approach) is left to the judgment of the surgeon.
TECHNIQUES
 Acetabular Exposure
Acetabular Exposure
The acetabulum is exposed and the failed construct and any soft tissue that interferes with visualization should be retracted or removed (TECH FIG 1A–E).
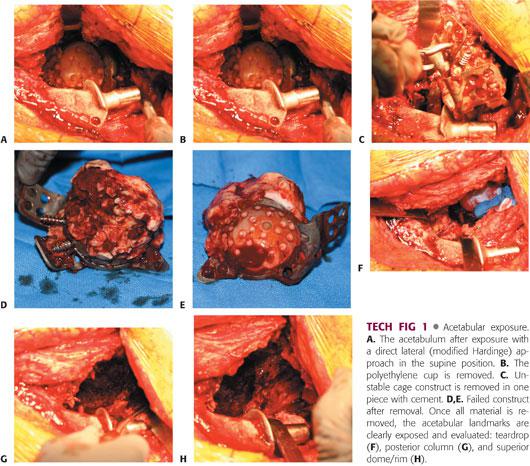
The anterior and posterior walls/columns, superior dome/rim, medial wall, teardrop, and ischium are identified and bone loss is noted (TECH FIG 1F–H).
 Intraoperative Determination of Reconstructive Technique
Intraoperative Determination of Reconstructive Technique
The remaining bone stock is assessed and corroborated with the preoperative assessment of bone loss.
Paprosky types 1, 2A, 2B, 2C, and 3A defects can usually be reconstructed with an uncemented acetabular component with or without bone grafting or trabecular metal augments.
All acetabuli, especially Paprosky type 3B defects, should be tested for pelvic discontinuity.
If pelvic discontinuity exists (TECH FIG 2), the surgeon may elect to use an antiprotrusio cage with or without posterior column plating or additional bone grafting.
Alternatively, the surgeon may elect to distract the discontinuity with an uncemented socket and bridge the defect in this manner.
The acetabulum should be assessed for the remaining bone’s ability to support an uncemented component. To support an uncemented cup, the remaining bone stock should allow for at least partial inherent stability of the reamer or trial.
Reamers or trials that are inherently unstable may not be appropriate for cementless reconstruction.
The reamers are not used initially to shape the acetabulum but are used to assess the ability of the remaining bone to support a socket.
If it is determined that the remaining bone stock cannot support a socket, then an antiprotrusio cage should be used.
 Bone Preparation
Bone Preparation
The ilium must be exposed with care to avoid the superior gluteal neurovascular bundle (TECH FIG 3A).

The size of the defect can be assessed with a standard acetabular reamer. The reamer can then be used to remove small amounts of bone that may prevent complete seating of the cage (TECH FIG 3B).
It should not be necessary to remove significant bone because the indication for use of this device is severe bone loss.
The outer diameter of the reamer that best fits the acetabulum determines the outer diameter of the cage.
The trial cage or the actual implant can be used to determine the removal of small amounts of bone that interfere with complete seating of the cage (TECH FIG 3C).
 Bone Graft and Trabecular Metal Augmentation
Bone Graft and Trabecular Metal Augmentation
The cage may not be stable in situations with severe superior dome or posterior bone loss.
It may be necessary to augment the acetabulum with either structural or particulate bone graft (TECH FIG 4) or trabecular metal to provide the cage with support.
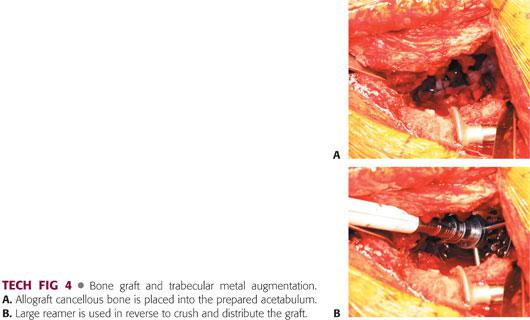
Severe superior dome or posterior wall or column bone loss may be reconstructed with structural allograft fashioned from a distal femur, proximal tibia, or acetabular allograft.
Trabecular metal acetabular components can be used in the cup–cage construct.
It may be necessary to support the trabecular metal acetabular component with a cage if native host bone contact is less than 50%. However, this technique is beyond the scope of this chapter.
 Cage Implantation
Cage Implantation
The ischial flange can be placed on or in the ischium (TECH FIG 5A,B).
The advantage of placing the flange on the ischium is that screws can be used to fix the cage to the ischium (TECH FIG 5C,D).
The advantage of blade-plating the flange in the ischium is avoidance of the sciatic nerve (TECH FIG 5E).
Both methods allow for stable fixation.
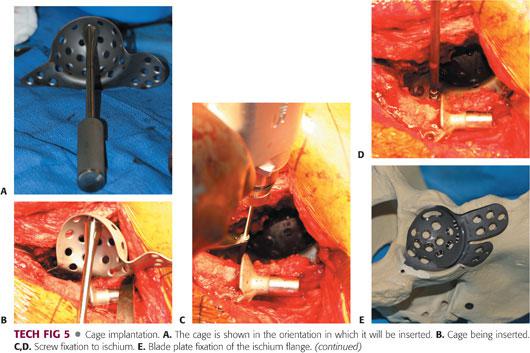
The cage is shaped to the contour of the ilium and ischium while allowing for seating of the socket portion of the cage into the remaining acetabulum. Usually, the ischial flange must be bent laterally to follow the contour of the ischium.
The ischial flange is fixed to or in the ischium using the surgeon’s preferred method.
The socket portion of the cage must be fully seated within the acetabulum to maximize the stability of the construct.
The flange must be contoured to the ilium to minimize cage motion. Usually, this requires the flange to be bent medially with some rotation.
Once the cage is appropriately contoured to the ischium, ilium, and acetabulum and fixed to the ischium, it is fixed with screws through the dome of the cage.
Fixation usually can be obtained in the posterior and anterior columns, with care to stay within the recognized safe zones.
Additional screws should then be passed through the superior flange into the ilium (TECH FIG 5F,G). The number of screws is limited by the amount of bone that can safely provide fixation.
A polyethylene liner is then cemented into the cage construct.
The cement is placed in the socket and pressurized (TECH FIG 5H–K).
A liner designed for cementation or a liner appropriately modified for cementation is then cemented into place in the appropriate position (TECH FIG 5L).
A 2-mm cement mantle is desirable.
Care must be taken not to leave large areas of the liner uncovered.
PEARLS AND PITFALLS | |
Preoperative planning |
|
| |
Preoperative workup |
|
| |
| |
Intraoperative bone assessment |
|
Bone preparation |
|
Cage fixation |
|
| |
| |
| |
| |
POSTOPERATIVE CARE
 Radiographs are taken to confirm appropriate cage positioning (FIG 3). Intraoperative radiographs may be beneficial to confirm cage positioning prior to final fixation of the device.
Radiographs are taken to confirm appropriate cage positioning (FIG 3). Intraoperative radiographs may be beneficial to confirm cage positioning prior to final fixation of the device.

 The patient is allowed protected weight bearing as tolerated if bone augmentation was not necessary.
The patient is allowed protected weight bearing as tolerated if bone augmentation was not necessary.
 The patient is restricted to toe-touch weight bearing for 6 to 12 weeks if bone augmentation was necessary. He or she is then allowed to increase weight bearing progressively on a schedule that is individualized to each patient.
The patient is restricted to toe-touch weight bearing for 6 to 12 weeks if bone augmentation was necessary. He or she is then allowed to increase weight bearing progressively on a schedule that is individualized to each patient.
OUTCOMES
 The survivorship of antiprotrusio cages has been acceptable in short- to midterm follow-up.
The survivorship of antiprotrusio cages has been acceptable in short- to midterm follow-up.
Several series have shown 100% survivorship at both 5 and 7.3 years1,7 and 93.4% survivorship at 10.9 years.3
However, because most of these devices cannot achieve biologic fixation, it is assumed that they will loosen over time. Long-term results have been mixed, with one series reporting 92% survivorship at 21 years,6 whereas another more recent study demonstrating a 61.75% survivorship at 14 years.5
 The success of these devices depends on the environment in which they are placed.
The success of these devices depends on the environment in which they are placed.
Most surgeons in North America use these devices only in cases of severe acetabular deficiency in which a press-fit uncemented socket is not appropriate. This may predispose these devices to failure.
One study on the use of the cage in the setting of discontinuity revealed a 31% revision rate at 46 months.2
A more recent, long-term study in patients with discontinuity has shown similar results with a 72.2% survival rate at 16.6 years.4
COMPLICATIONS
 The use of antiprotrusio cages is accompanied by the complications inherent to significant revision surgery:
The use of antiprotrusio cages is accompanied by the complications inherent to significant revision surgery:
Blood loss
Infection
Neurovascular injury
Construct failure
Anesthetic and medical complications
REFERENCES
1. Lamo-Espinosa J, Duart Clemente J, Diaz-Rada P, et al. The Burch-Schneider antiprotrusio cage: medium follow-up results. Musculoskelet Surg 2013;97:31–37.
2. Paprosky WG, Sporer S, O’Rourke MR. The treatment of pelvic discontinuity with acetabular cages. Clin Orthop Relat Res 2006;453:183–187.
3. Pieringer H, Auersperg V, Bohler N. Reconstruction of severe acetabular bone-deficiency: the Burch-Schneider antiprotrusio cage in primary and revision total hip arthroplasty. J Arthroplasty 2006;21:489–496.
4. Regis D, Sandri A, Bonetti I, et al. A Minimum of 10-year follow-up of the Burch-Schneider cage and bulk allografts for the revision of pelvic discontinuity. J Arthroplasty 2012;27(6):1057–1063.
5. Symeonides PP, Petsatodes GE, Pournaras JD, et al. The effectiveness of the Burch-Schneider antiprotrusio cage for acetabular bony deficiency. J Arthroplasty 2009;24(2):168–174.
6. Wachtl SW, Jung M, Jakob RP, et al. The Burch-Schneider antiprotrusio cage in acetabular revision surgery: a mean follow-up of 12 years. J Arthroplasty 2000;15(8):959–963.
7. Winter E, Piert M, Volkmann R, et al. Allogeneic cancellous bone graft and a Burch-Schneider ring for acetabular reconstruction in revision hip arthroplasty. J Bone Joint Surg Am 2001;83A:862–867.
< div class='tao-gold-member'>
















