Chapter 11 The Omega “Ω” Flexor Pulley Plasty
Outline
The conservative camp proposed the concomitant repair of the digital fibrous tube with the primary suture of the flexor tendon injuries to restore the sheath integrity and avoid the formation of adhesions.1,2 However, the failure of the fibrous sheath to heal and, more dramatically, the risk of creating a constriction to tendon gliding have led several surgeons to abandon this approach.3–8
The repair of injured digital flexor tendons, either primarily or secondarily, is accompanied by an increase in the diameter of the tendon where sutures are placed, increasing resistance to movement.9 To avoid this risk, several authors10–12 prefer to deal with the fibrous sheath structure and propose a partial or a complete resection of the A2 or A4 annular pulleys.
Enlarging the digital fibrous sheath by “venting” the pulley is attractive theoretically.12 However, even if it does improve the local mechanical conditions around the tendon repair site, incision into the pulley structures may decrease digital flexion to a certain degree. Anatomic work has showed that the most remarkable loss of function is caused by resection of the annular pulleys A2 and A4.13 We thus began to imagine technical innovations that would resolve this conflict more specifically without affecting the integrity of the annular pulleys.
Methods and Outcomes
Anatomy of the Fibrous Digital Sheath Tunnel
Though the anatomy of the digital fibrous sheath is familiar, we review some points that are important for explaining the Omega (“Ω”) pulley plasty. The pulleys segmentally distributed along the synovial sheath differ by their sites of insertion and their plasticity.14 The annular pulleys A1, A3, and A5 (also called articular pulleys), are attached to the palmar joint plates of the metacarpophalangeal (MP), the proximal interphalangeal (PIP), and the distal interphalangeal (DIP) joints, respectively. The lengths of these pulleys change during digital motion, with an approximate 50% retraction after full digital flexion,13,15 whereas the A2 and A4 pulleys (bone pulleys) insert on the lateral phalangeal crests in continuity with the lateral periosteum and with the floor of the digital fibrous sheath tunnel. The A2 pulley is situated in the middle and proximal part of the proximal phalanx, and the A4 pulley in the middle third of the middle phalanx. The lengths of the A2 and A4 pulleys change somewhat (less than 25%) during digital flexion.
All the relevant biomechanical studies to date agree, giving functional priority in finger flexion to the A2 and A4 pulleys.13,16 It is on these two pulleys that the pulley plasty is performed during tendon repair in zone 2,17 more precisely in zones 2B and 2C.18
Operative Techniques
Omega Plasty of the A4 Pulley
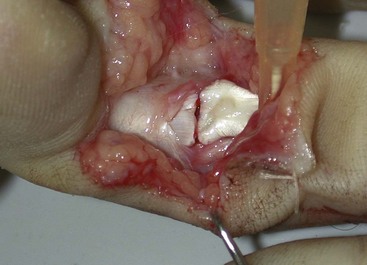
If the finger is in an extended position, the distal tendon stump is retracted and hidden completely under the A4 pulley. It is necessary to flex the DIP joint to expose the tendon and to place the two stumps in the operative field (Figure 11-1).
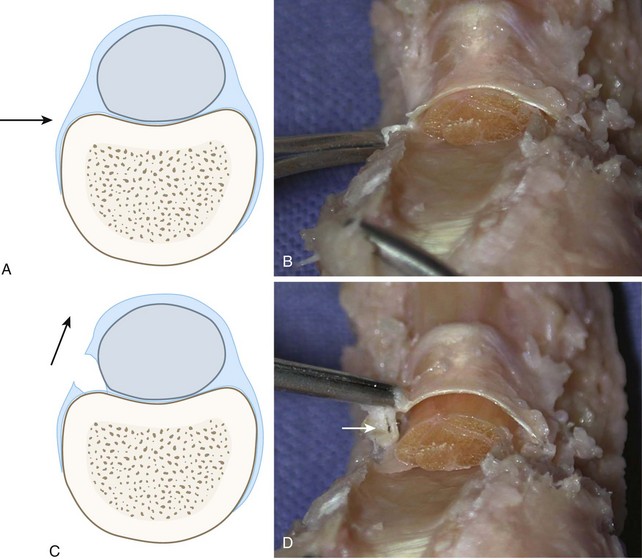
The ulnar digital neurovascular bundle is retracted and the entire ulnar phalangeal bone attachment of the A4 pulley is exposed. The ulnar periosteum is sharply incised along the body of the middle phalanx and freed progressively from dorsal to palmar. The ulnar pulley attachment is then reached and freed from the ulnar phalangeal crest until it has been totally liberated (Figure 11-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree