Chapter 3 Tendon Friction, Lubrication, and Biomechanics of Motion
Outline
Tendon Friction
Tendon Friction in Physiological Conditions
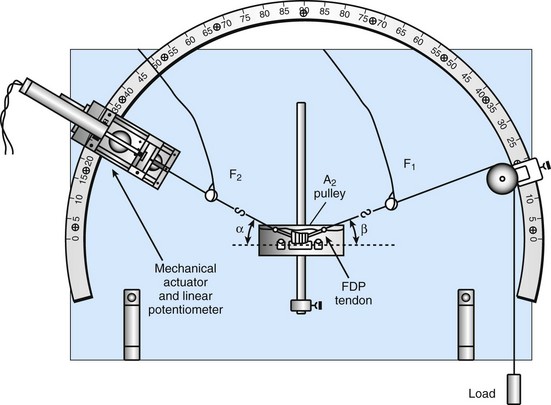
When tendons glide against surrounding tissue, especially when passing through a series of pulleys in the fingers, frictional force must be encountered. An et al1 developed a tendon/pulley gliding model to measure the frictional force and calculate the frictional coefficient (Figure 3-1). If the impending motion of the cable is from F1 to F2, then F2 is greater than F1 due to the friction f, and f = F2 − F1. F2 is also related to F1 as F2 = F1eµø, where µ is the frictional coefficient. If a logarithm is taken, LnF2/F1 = µø. If the values of F2, F1, and ø are known and natural logarithms of F2/F1 are plotted against angles in radians, the frictional coefficient can be calculated as the slope of a line designed according to the least-squares method.2
The assessment of frictional force at the tendon–pulley interface with this method is an ideal model. However, tendon gliding is far more complicated. In classical theory, for friction without a lubricant, three laws have been postulated3: (1) The frictional force is directly proportional to the applied load; (2) frictional force is independent of the apparent area of contact; and (3) the kinetic frictional force is independent of the sliding speed. However, these rules must be modified in tendon, for several reasons. First, the tendon is a viscoelastic tissue. Its properties are affected by the velocity of tendon motion, and its surface deforms in response to contact pressure. In addition, tendon is lubricated, at least normally.
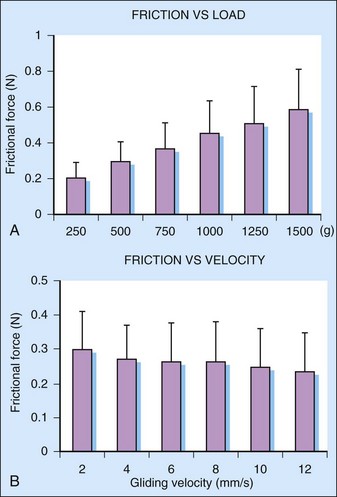
Moriya et al4 investigated three parameters that may relate to tendon friction: temperature (4°C, 23°C, and 36°C), gliding velocity (2, 4, 6, 8, or 12 mm/sec), and load (250, 500, 750, 1000, 1250, and 1500 g) applied to the tendon using a flexor digitorum profundus tendon and A2 pulley model. They found that the tendon friction was proportional to load, but not, within the ranges studied, to gliding velocity (Figure 3-2A and B). The temperature also affected the tendon friction; the friction at 4°C was significantly higher than that at body temperature, 36°C. This information is useful to guide the experiments that relate to tendon frictional testing. Some studies have also demonstrated that tendon frictional force is dependent on joint position or the direction of motion. Zhao et al5 found that the friction at the flexor tendon–transverse carpal ligament interface was significantly higher in wrist flexion compared to the neutral position. Heers et al6 studied the frictional force of the long head of the biceps tendon during shoulder motion and found that the frictional force during abduction was significantly higher than that of adduction.
Tendon Friction in Pathological Conditions
The normal tendon frictional force is small. The frictional coefficient of flexor tendon in zone 2, where two flexor tendons are enveloped by flexor sheath with synovial fluid between, is comparable to that of cartilage.7–9 However, the frictional force after tendon injury and repair dramatically increases, which impairs tendon function. Sutures create roughness of the tendon surface and increase friction. Sutures also increase the volume of the tendon, and postinjury edema can increase friction as well. Afterward, the biological healing between tendons and surrounding tissue forms adhesions, which increase the frictional force and may in some cases totally impede tendon gliding.
Strategies to reduce the fictional force after tendon repair have been studied.7,10–12 Surface friction of a repaired tendon can be reduced by burying knots between tendon ends, or locating the knots away from the anterior tendon surface, choosing low friction suture materials, and using fewer suture loops and strands.13,14 Using a canine in vivo model, Zhao et al15 found that a lower friction repair technique, the modified Kessler repair, had fewer adhesions after 6 weeks compared to a higher friction technique, the modified Becker repair. However, these positive adhesion outcomes were combined with higher rates of gap formation and rupture. To balance the tensile strength and friction, several studies have studied suture techniques with higher tensile strength and lower friction. Momose et al16 used a looped suture with a modified Kessler suture technique to repair flexor tendons and achieved high tensile strength with relative low friction. Later, Tanaka et al17 demonstrated that the modified Pennington technique possesses low friction and high strength.
Some alternative surgical techniques have been developed to minimize bulk after tendon repair. Resection of one slip of the flexor digitorum superficialis (FDS) tendon decreased the repaired flexor digitorum profundus (FDP) tendon gliding resistance.18 Pulley plasty also reduces friction.19 Trimming the pulley edge on an oblique, rather than perpendicular to the long axis of the bone, may also help the repaired tendon pass through with less risk of triggering.20
The frictional force of a repaired tendon with a gap has also been studied. The friction of repaired tendons without gap mainly comes from surface roughness. However, with gap formation, plowing friction, related to surface shape, becomes dominant, which dramatically increases the resistance. If a repaired tendon has a 3-mm or larger gap, the plowing frictional force may increase sharply due to the trapping of the repaired tendon edge on the pulley, eventually leading to repair failure if the applied load exceeds the repair strength.21
The tendon frictional force may also increase in circumstances not related to tendon injury or repair. Joint deformities that cause the tendon pulley gliding angle to increase, as in rheumatoid arthritis, also increase frictional force.22 Trigger finger is another example where increased bulk and decreased lubrication hamper tendon gliding through the pulley. The integrity of the flexor pulley system is also important to maintain normal frictional force during finger motion. Resection of the A3 pulley increases the gliding resistance between tendon and A2 pulley.23 Increased carpal tunnel pressure also increases tendon frictional force.24
Tendon Friction in Different Tendon Surroundings
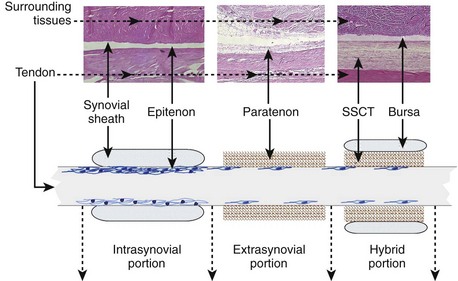
Tendons can be classified as intrasynovial and extrasynovial tendons based on their surrounding environment.25 Intrasynovial tendons are defined as tendons, or parts of tendons, enclosed within a synovial sheath. These tendons are lubricated by synovial fluid, and the tendon surface is covered by a thin visceral synovial membrane, the epitenon (Figure 3-3). The epitenon cells are similar to synovial cells and secrete lubricants. This unique structure effectively decreases friction, reduces abrasion, and eliminates wear. Flexor tendons in zone 2 area are typical intrasynovial tendons. Extensor tendons in the dorsal wrist area, the long head of the biceps brachii tendon, and the posterior tibial tendon at the medial malleolus are other examples of intrasynovial tendons. In contrast, the tendons located within subcutaneous soft tissues are extrasynovial tendons. These tendons are covered by loose connective tissue, called paratenon (see Figure 3-3). In addition, some tendons have a hybrid type. Ettema et al26 reported that flexor tendons in zone 4 (within the carpal tunnel) have a unique structure, in which the subsynovial connective tissue (SSCT), a paratenon-like structure, covers each flexor tendon. The SSCT and tendon are in turn encased in a synovialized bursa. Therefore, the flexor tendons in this region include both intrasynovial and extrasynovial gliding mechanisms (see Figure 3-3).
Although the gliding ability of the paratenon is not as durable as the epitenon, it serves as a cushion and sliding sleeve to protect the tendons from surrounding tissues, such as muscle, bone, and neurovascular structures. It also serves as a network to protect the vessels and nerves that provide the nutritional supply of tendons.27
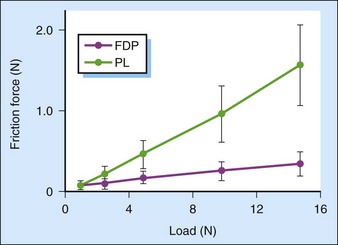
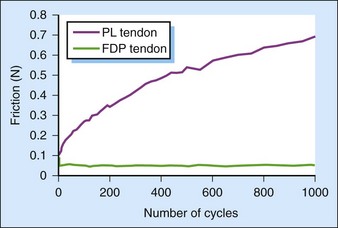
Due to the differences of anatomy and structure between intrasynovial and extrasynovial tendons, the frictional force of extrasynovial tendons is much higher than that of intrasynovial tendons.28,29 Uchiyama et al found that the frictional force of the palmaris longus tendon increased with increasing loads. In contrast, the frictional force of FDP tendon was nearly independent of the load applied to the tendon (Figure 3-4). Several studies have demonstrated that the frictional force of extrasynovial tendons increases rapidly with cyclic motion,29–31 while intrasynovial tendons maintain a constant frictional force even after 1000 cycles of tendon motion (Figure 3-5).
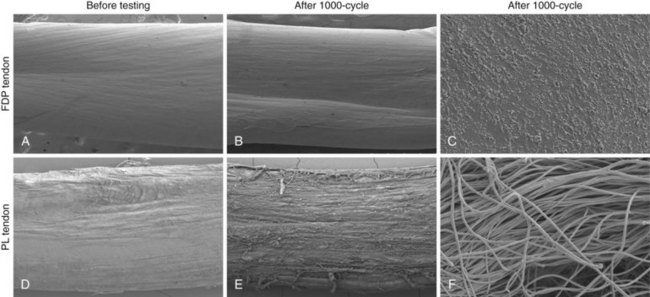
Tendon surface morphology has been studied with the use of electron microscopy. These studies show that the intrasynovial tendon surface has a smooth surface, with no collagen fibrils exposed on the surface. After cyclic motion, this smooth surface is maintained. In contrast, the paratenon on the extrasynovial tendon surface wears off with cyclic motion, exposing increasing amounts of collagen fibrils with increasing number of motion cycles (Figure 3-6). One could argue that extrasynovial tendon rarely glides against a pulley, but this is only true normally. When an extrasynovial tendon is used as a graft to reconstruct an intrasynovial tendon, which is a common clinical situation, then the tendon does glide against a pulley. While there are many reasons why tendons may form adhesions, increased friction is certainly one of the major factors to consider, which can be ameliorated if an intrasynovial graft is available. Unfortunately, there are few intrasynovial tendons that can be sacrificed for the purpose of tendon grafting. The development of a tissue-engineered intrasynovial graft is one object of our research.
Tendon Lubrication
Lubrication has been the focus of intense study in articular cartilage, since cartilage degeneration is associated with mechanical abrasion and wear.32–34 Although tendon does not bear as much compressive loading as cartilage, the number of motion cycles experienced by tendons is comparable to that of joints and was estimated at over 1 million cycles per year.35,36 Therefore, tendon lubrication is very important, especially for the intrasynovial tendons in the hand, which experience the most cyclic motion. Since the gliding structure of the intrasynovial and extrasynovial tendon structure is different, the lubrication mechanism is also totally different.