Chapter 9 Treatment of the Flexor Tendon Sheath and Pulleys
Outline
The synovial sheath and segmental pulleys are a prominent feature of the flexor tendon system in the hand. Because injury to the sheath occurs in all flexor tendon lacerations in the digits and we cannot approach the tendons without violating the sheath surgically, considerable investigations have been devoted to this topic over decades.1–33 The significance of proper treatment of the sheath—the rigid and condensed annular pulleys in particular—has received great attention in efforts to optimize the outcomes of flexor tendon surgery.
Anatomy
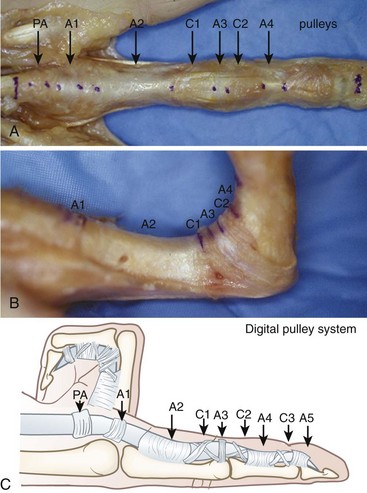
The digital flexor sheath is a closed synovial system extending from the distal part of the digits to the metacarpophalangeal (MCP) joint levels of the digits. The sheath consists of membranous portions of continuous synovial sheath (called simply the “sheath”), and condensed retinacular components (the “pulleys”). A layer of thin, smooth, and continuous membrane covers the inner surface of the entire sheath and pulleys. Pulleys are segmentally located and overlie the membranous lining. The pulleys include annular pulleys (condensed, rigid, and heavier annular bands), cruciate pulleys (filmy cruciform bands), and the transverse palmar aponeurosis pulley (Figure 9-1).1
In each of the four fingers, there are five annular pulleys (A1, A2, A3, A4, and A5), three cruciate pulleys (C1, C2, and C3), and one palmar aponeurosis (PA) pulley.1–3 The A1, A3, and A5 pulleys originate from the palmar plates of the MCP and proximal and distal interphalangeal (PIP and DIP) joints, respectively. The A2 and A4 pulleys originate from the middle portion of the proximal and middle phalanges, respectively. The broadest is the A2 pulley, which covers the proximal two-thirds of the proximal phalanx and encompasses the bifurcation of the flexor digitorum superficialis (FDS) tendon. The A4 pulley is located at the middle of the middle phalanx. The A2 and A4 pulleys are structurally the most critically located and, functionally, the most important.
Function
The synovial sheath offers a smooth gliding bed and provides synovial nutrition to the tendons. Mechanically, the pulleys serve to strengthen the sheath and hold the flexor tendons close to phalanges and their joints. The annular pulleys act as a fulcrum, optimizing the mechanical efficiency of digital flexion. The more compressible cruciate pulleys allow for digital flexion with condensation of the fibro-osseous sheath at the inner part of flexed fingers (called the “concertina effect”) (see Figure 9-1). Both forms of pulley prevent anterior displacement (i.e., bowstringing) of the tendon during finger flexion.
In the finger, the A2 pulley is the strongest in respect of preventing anterior displacement of the tendons and is at the most critical location. The A2 and A4 pulleys are most important in maintaining the biomechanics of the tendon gliding, although the other sheath components do contribute to the maintenance of tendon mechanics. Absence of a series of pulleys will affect tendon mechanics. Manske and Lesker2 investigated the roles of the A2, A1, and PA pulleys and found that absence of any two, or all three, pulleys resulted in tendon bowstringing. Tang and Xie20 investigated the roles of the A3, C1, and C2 pulleys and found that these pulleys help to restrain tendon bowstringing.
In the thumb, the proximally located A1 pulley and the oblique pulley are the most important functionally. The distally located A2 pulley of the thumb is thin and is relatively unimportant. Doyle and Blythe3 found significant decrease in motion of the distal joint of the thumb when both the A1 and the oblique pulleys were removed, but loss of either alone did not noticeably affect the motion of this joint.
Historical Review
A review of the conceptual changes regarding roles and treatments of the sheath, pulleys in particular, are provided by Elliot, together with his commentaries in the Chapter 10. Here, Box 9-1 summarizes the work of other groups that influenced our studies, the time sequence of our investigations, and evolving philosophies, leading to current treatment guidelines.4–29
Box 9-1 Some Major Steps Toward Current Treatments of Sheath and Pulleys Over the Past 25 Years
1985: Lister, in a review, advocated sheath closure and described the method to create sheath flaps to assess the tendon and accommodate surgical repairs.4 This review had a great impact on later clinical practice of sheath closure.
1985: Strauch and colleagues compared the results of sheath closure with vein grafts with sheath excision in chickens. They found improved digital motion after restoration of sheath integrity.5
1986: Peterson and Manske compared the mechanical and histologic outcomes of sheath repair and excision in a chicken model. They concluded that closure of the flexor sheath does not improve tendon gliding.6,7
1987: Saldana and colleagues compared surgical closure (42 fingers) and opening (48 fingers) of the sheath after tendon repairs in zone 2 in a comparative perspective study. There was no statistical difference between the results of the patients with the two treatments.8
1988: Manske, in a review, stated, “It should be kept in mind that a water-tight closure of the tendon sheath may in fact narrow the diameter of the fibro-osseous canal and reduce its volume.”9
1990: Tang, Ishii, and Usui compared the mechanical and histological results of sheath repair, excision, and enlargement sheath plasty by autogenous grafts using chickens. Tendon gliding was not improved after sheath closure, but was improved after enlargement plasty. They considered that the fibro-osseous digital sheath is comparable to the fibro-osseous muscle compartments in the extremities, and proposed a “digital sheath syndrome” to explain pathophysiology in the tendon after tight sheath closure.10
1990: Gelberman and colleagues compared sheath reconstruction and excision in canines treated by early motion rehabilitation, and substantiated that sheath repair—either by suture or graft—does not improve the biomechanical, biochemical or morphologic features of the tendons.11
1990: Savage measured tendon excursion, profundus tendon flexion force, and tendon bowstringing using five cadaveric hands after varying combined excisions of the annular pulleys. He stated, “In an otherwise intact digital fibrous flexor sheath, A2 and A4 pulleys were no more important mechanically than the other pulleys.”12
1994: Tang and colleagues reported that closure of the sheath did not improved tendon gliding in chickens at multiple time-points of delayed primary repair.13
1995: Tang studied the anatomy of the A2 pulley specifically, using cadaveric hands, by measuring the tendon excursion after midline incisions through part of the A2 pulley, and the vertical and horizontal diameters of distal, middle, and proximal parts of this pulley. He proposed the partial release of the pulley and stated, “To improve tendon healing and gliding, procedures for A2 pulley release, including incision of the critical portion to free tendon motion or enlargement of the A2 pulley, can be performed.”14
1996: Tang, Shi, and Zhang examined the effects of sheath narrowing and enlargement on tendon excursions, healing, and adhesions using chickens. They demonstrated that the diameter of the surgically repaired sheath exerts great influences on tendon function.15
1998: Kwi, Ben, and Elliot reported the clinical results of zone 2 flexor tendon repairs in 185 fingers in 166 patients together with lateral release of the A2 and A4 pulleys. They showed practicability of active partial release of these pulleys. They stated, “It was necessary to vent the A4 pulley between 10 and 100% of its length in 71 (56%) of the fingers and to vent the distal edge of the A2 pulley by 4 to 10 mm in 10 (8%) of the fingers.”16
1999: Tang and colleagues reported 1-year follow-up of the finger motion after simple partial release through the one-half to two-thirds portion along the midline of the A2 pulley or with enlargement pulley plasty in 16 fingers. No tendon bowstringing was noted. They advocated “partial release of the A2 pulley up to 1/2 or 2/3 lengths of the A2 pulley under the condition that other pulleys are intact.”17
1998, 1999: Tomaino, Mitsionis, and colleagues performed cadaveric studies to substantiate that partial release of the A2 and complete release of the A4 pulley do not significantly alter tendon mechanics.18,19
2001: Tang and Xie, in a cadaveric study, showed that loss of an A3 pulley does not affect tendon biomechanics, but cruciate pulleys and synovial sheath restrain tendon bowstringing. They advise not creating lengthy sheath defects, given the integrity of major annular pulleys.20
2002: Elliot, in a review, highlighted the feasibility of pulley-venting. He stated: “In reality, … as the A2 pulley is of sufficient length that one can excise any one-third of it to allow repair and free movement of the repair and still have a pulley which is one or more centimetres in length, and thus, functional.” Regarding the sheath, he stated: “It is now our practice after zone 2 repairs to simply lay the sheath back over the tendons without suturing, after adequate venting of the A2 and A4 pulleys to allow free running of the repairs.21
2002: Amadio, Zhao, Paillard, and colleagues investigated gliding resistance of the FDP tendon after resection of one slip of the FDS tendon and Kapandji pulley plasty, and found that both pulley plasty and resection of one slip of the FDS reduce gliding resistance.22
2003, 2007: Tang, Xie, Xu, and colleagues investigated tendon repairs within and proximal to a major pulley using chickens. Worse results of surgeries were noted in the pulley area.24 They compared the results of simple pulley incision, Kapandji pulley plasty, and excision of one slip of the FDS and found no improvement of tendon gliding after Kapandji pulley plasty.25
2004: Tanaka, Amadio, An, and colleagues investigated gliding resistance of the tendon and pulley strength after the A2 pulley was excised successively by 25%, 50%, and 75%. Their data support the clinical practice of partial pulley excision, up to a limit of 50%.26
2007: Tang, in a review, highlighted the critical roles of proper and sufficient release of critical annular pulleys in achieving predicable functional recovery. He outlined precisely the lengths and areas to be release in different locations of injuries. He considered that proper release of the pulley may be even more effective in reducing repair ruptures than use of a strong repair.27
2009: Cao and Tang compared the strength of the repaired tendon with the A2 pulley intact or vented at varying digital flexion. They recorded that the strength decreased significantly when the pulley was intact.29
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree