Our experience with NSM at Georgetown continues to evolve, including our increasing preference for inframammary incision placement, and a preference for permanent rather than frozen section pathologic confirmation of tumor free or clean retroareolar margins. With increasing false-positive frozen sections, we now send the tissue for permanent section only. Traditional teaching has been that if either the frozen section or permanent sample come back positive the nipple areolar complex must then be resected [3, 4].
With great technical success and oncologic safety implementing these criteria, efforts moved towards maximization of esthetic outcomes and patient satisfaction.
Early Experience with Lateral Incisions
As discussed previously our initial incision of choice for NSM was lateral radial incisions with the option of 90–180° extensions around the edge of the areola which allowed adequate access to perform a retroareolar biopsy as well as adequate oncologic resection.
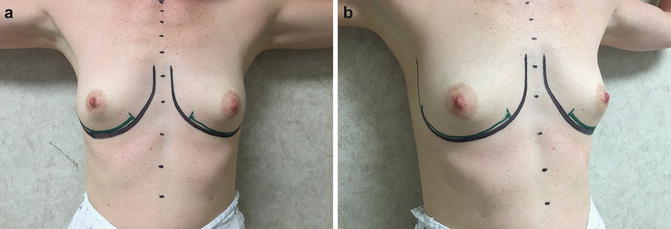
However, unlike a skin-sparing mastectomy where the NAC is actively reconstructed in a staged fashion, a nipple-sparing mastectomy retains the original NAC position passively and its final position is ironically less controllable. We found the risk of nipple malposition is increased by a lateral breast incision and especially radiation. No matter what incision is used, any incision and any mastectomy preferentially tightens the skin above the nipple and further elevates the NAC, and this was exacerbated using a lateral radial incision (Fig. 4.2).
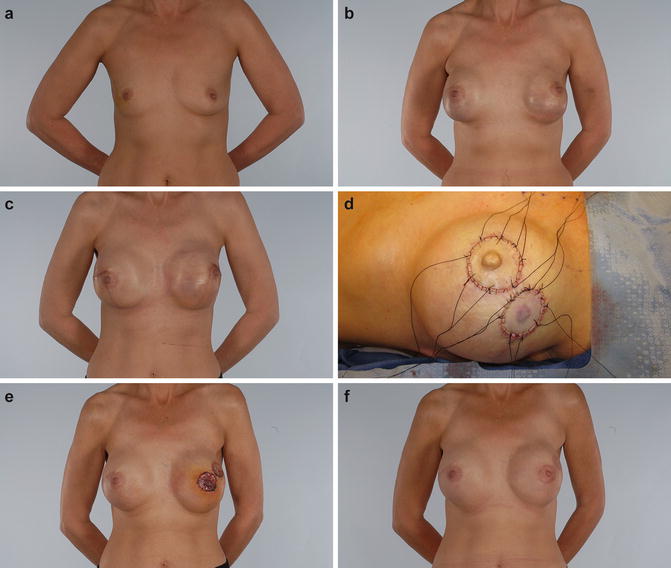
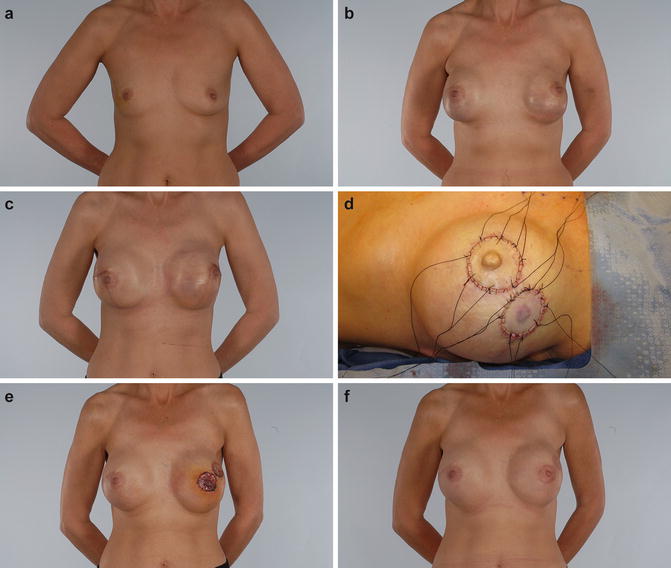
Fig. 4.2
Fifty-three-year-old female with invasive right breast cancer (a) elected to undergo bilateral nipple-sparing mastectomy through a lateral incision with superior, peri-areolar extension. She had an immediate reconstruction at the time of her mastectomies with 300 cc tissue expanders, filled to 150 mL intra-operatively, and acellular dermal matrix. The expanders were filled to a volume of 310 mL over the next several weeks and at 4 months underwent an implant exchange using high profile, smooth round 450 cc gel implants. Immediately postoperatively (b) the left nipple was noted to be displaced superiorly and laterally. This nipple malposition persisted at 6 months (c) at which point she elected to have an excision and grafting of the NAC to a more favorable location (d, e). This result is maintained at 1 year (f)
In our experience and in the experience at many other centers, the lateral breast incision with peri-areolar extension also compromises the blood supply to the nipple by bisecting the breast, directly decreasing flow through the subdermal plexus to the NAC [5]. The blood supply of the breast post-mastectomy is provided predominantly by the second intercostal perforator and the subdermal plexus. If the second intercostal perforator is violated, skin flap and NAC survival is reliant upon the collateral flow from the subdermal plexus. In light of this, it is thought that the inframammary (IMF) approach to a nipple-sparing mastectomy is superior to lateral incision in terms of blood supply to the NAC because it preserves the subdermal plexus around the entire perimeter of the nipple areolar complex . This translates clinically into a higher incidence of nipple necrosis using the lateral incision with peri-areolar extension as compared to the inframammary approach [5, 6].
Evolution of NSM: The Inframammary Approach
Patient selection for the IMF incision is critical in order to minimize the risk of wound dehiscence and delayed healing. Prior surgical scars and the expected length of the skin flaps must be assessed to determine if this surgical approach to the NSM is warranted. Specifically, patients with preoperative ptosis are at risk of postoperative delayed healing as they will have long mastectomy flaps. As the flap length increases, the likelihood of adequate tissue perfusion along the incision decreases. The relationship between flap length and thickness will help to predict success or surgical complication and should be considered preoperatively and then again assessed intra-operatively at the conclusion of the mastectomy using indocyanine green laser angiography or other accurate imaging system . Technical limitation of the IMF incision, namely difficulty visualizing and subsequently removing the superior-lateral glandular tissue, can be overcome with a combination of retraction and hand-guided dissection or when necessary a counter incision hidden in the axilla. Various techniques can facilitate surgery through the more remote IMF incision. In particular scalpel or scissor dissection without constant internal direct visualization works well as compared to trying cautery at a distance in a dark hole. Bipolar as compared to monopolar cautery is kinder to the tissues and the blood supply. And the availability of better lighted retractors such as the Invuity (Invuity Inc., San Francisco, CA) has made things easier as well, and allows for direct visualization of the superior-lateral parenchyma to ensure the mastectomy is complete and uniform over this region (Fig. 4.3).
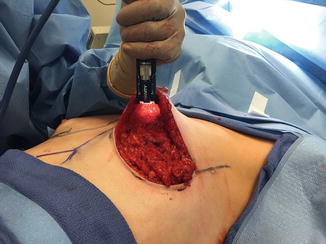
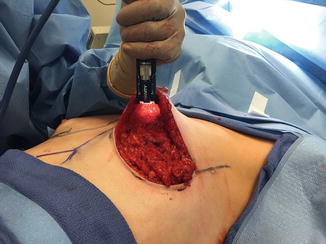
Fig. 4.3
Retraction using a lighted retractor during nipple-sparing mastectomy through an IMF incision
The IMF incision has gradually evolved into our preferred approach to NSM as our surgical team has gotten more familiar and comfortable with remote mastectomy incisions and given its decreased risk of partial or complete nipple necrosis (Fig. 4.4). When necrosis does occur using the IMF approach, it rarely involves the nipple and tends to occur instead on the hidden lower pole of the breast or at the edge of the flap which makes it easier to manage and also allows the damage to be kept more out of sight. Attempts to further improve outcomes have led us to extend this incision laterally for some select patients . In cases of predicted difficulty gaining access to the superior-lateral breast by the breast surgeon during the mastectomy, unfavorably medial preoperative NAC position, or need to better define the lateral breast the IMF incision can be extended laterally while still allowing for an inconspicuous scar (Fig. 4.5). In select cases, an extended lateral incision also allows access to the axillary lymph node basin avoiding a counter-incision.
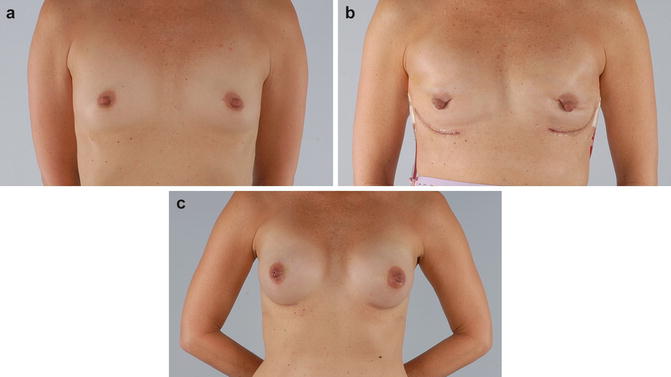
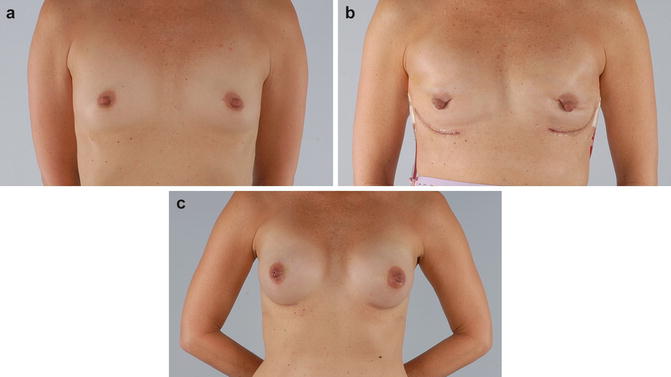
Fig. 4.4
Forty-nine-year-old female (a) with a strong family history of breast and ovarian cancer elected to undergo bilateral nipple-sparing mastectomies and immediate breast reconstruction using tissue expanders and acellular dermal matrices through an IMF incision. Three hundred and fifty milliliter tissue expanders were initially filled to 150 mL at the time of surgery. (b) Following complete expansion, she presented 3 months later for exchange to oval base, high projecting 370 cc shaped silicone implants. The 1-year result is shown here (c)
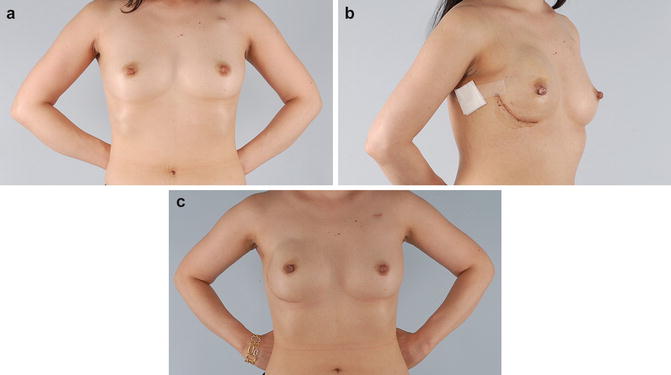
Fig. 4.5
Forty-two-year-old female with newly diagnosed invasive right breast cancer (a) seeks prosthetic reconstruction . An extended lateral IMF incision was utilized for the NSM in order to obtain easier access to the axillary tail and immediate reconstruction using a tissue expander (275 mL initially filled to 125 mL) and acellular dermal matrix. (b) Note the sentinel lymph node biopsy was also performed through this incision. Three months later, she underwent an implant exchange with 390 cc moderate plus projecting shaped gel implants. Six-month results are shown (c)
Operative Technique
Thoughtful and precise preoperative markings are necessary in order to execute a successful NSM and immediate reconstruction. Landmark identification must be highlighted with the patient in a standing position in order to correctly identify the breast footprint and in particular the true inframammary fold which may be ill-defined or mobile in the deflated or multiparous breast, In some cases where the original fold sits abnormally high and close to the nipple (N-IMF distance pre-op measured at 7 cm or less), it may be wise to plan the incision at a nipple to fold distance of 8 or 9 cm in order to accommodate the anticipated reconstructed breast size (Fig. 4.6). Immediately prior to surgery, the planned IMF incision is infiltrated with local anesthetic and epinephrine solution. The incision is sharply made and double-prong skin hooks are used to help develop a plane between the gland and subcutaneous skin flaps. The dissection proceeds by first separating the breast from the skin flaps or from the pectoralis major; however, most commonly the plane between the gland and skin flaps is approached first. In this case, dissection is carried out sequentially from the IMF using sharp scissors, keeping electrocautery (preferably using the less traumatic bipolar variety or the less thermally destructive PEAK® PlasmaBlade System—Medtronic, Minneapolis MN) to a minimum and reserved only for planned vessel cautery in an effort to balance hemostasis and flap perfusion. As the nipple areolar complex is encountered it is separated from the underlying breast with a sharp scalpel just deep to the dermis. Exposing the subareolar region, the nipple papilla is discovered and a retroareolar biopsy is taken at a point of duct confluence (Fig. 4.7). We do not recommend nor do we perform a nipple coring procedure as we deem this both unnecessary and specifically contrary to the goal of retaining a realistic facsimile of a nipple including some projection. This specimen is sent for permanent pathology sectioning. The remaining skin flap is then raised superiorly using meticulous scissor dissection aided by gentle, intermittent illuminating breast retraction. It is imperative to keep dissection true to the breast footprint and not to artificially extend the dissection beyond breast tissue simply to encounter the clavicle superiorly and the latissimus laterally. While these may serve as obvious limits of the breast not all women have breast tissue extending to these structures. Once circumferentially released, the gland is then reflected caudally as the breast is dissected from the pectoralis major using electrocautery in a superolateral to inferomedial direction or vice versa depending on which seems most practical [3].