The Global Impact of Scars
Mayer Tenenhaus
Hans-Oliver Rennenkampff
Bruce Potenza
KEY POINTS
Teleology of scars. The process of scar formation is an extension of the reparative wound healing process. On one end of the spectrum, scar tissue aids in wound closure by assisting in wound contracture and reepithelialization and contributing to wound strength. There is little doubt that the ability to form a scar, the inevitable consequence of injury, directly and efficiently incurs survival benefit to the individual. The ability to rapidly and effectively close one’s wounds protects the individual from further injury and insult, the importance of which cannot be overstated. From an evolutionary standpoint, delays in wound healing may have rendered an organism vulnerable. As a consequence, optimal healing represents a compromise between slower and more energy-intensive scarless healing and a quicker healing time with some degree of long-term scar sequelae.
Characterization and classification of scars. There are three commonly described types of scars. They include simple, atrophic, and hypertrophic/pathologic (inclusive of hypertrophic scars [HTS] and keloids). Their histopathology, presentation, patterns of distribution, evolution, and involution are distinct.
Consequences globally and to the individual. Significant consequences are associated with and result from scars. Individual, cultural, psychological, and societal influences, prejudices, and interpretations certainly play a major role in conceptualizing scars both for the individual and for society. Socioeconomic and financial challenges both as causative influences and as costs to the patient and society can similarly not be overstated.
There is little doubt that the ability to form a scar, the inevitable consequence of injury, directly and efficiently incurs survival benefit to the individual. The ability to rapidly and effectively close one’s wounds protects the individual from further injury and insult, the importance of which cannot be overstated. From an evolutionary standpoint, delays in wound healing may have rendered an organism vulnerable. As a consequence, optimal healing represents a compromise between slower and more energy-intensive scarless healing and a quicker healing time, with some degree of long-term scar sequelae.
Scar formation positively impacts biologic organisms when a balance is established optimizing the functional and aesthetic result in effecting wound closure. It is perhaps here that scarring affords its greatest and most significant global and biologic impact. One can argue that pure regenerative healing represents the highest quality reparative effort. Although it remains a potential therapeutic endeavor, tragically this potential is rarely realized by higher life forms. Wound healing is a function of genetic efficiency, energy requirements, cost, benefit, and evolutionary direction.
The Global Burden of Scarring
The composite effect of the global burden of scarring as a pathologic condition remains ill defined. Reports tend to focus on subsets of patients, generally describing the complication of scarring as it relates to a specific disease entity such as burns and trauma, or scarring complicating elective surgical procedures. These reports are usually bound by single or multiple institutions and by a geopolitically similar socioeconomic area. Composite descriptions of the problems associated with scarring are estimates and at best extrapolations based on limited data. Burns represent one of the most significant contributors to trauma-related scarring. In higher income nations, data collected on the incidence of burn injuries have improved markedly with the establishment of formal databases, but middle and lower-income countries, unfortunately, can provide only limited epidemiologic data on this subject. As a result, even in this well-represented population, the true incidence of the global burden of burn injuries relies on extrapolation from limited clinical data. To further complicate matters, all burns and
the associated wound care may differ greatly. Patients from higher socioeconomic countries generally receive prompt burn wound care with comparatively early excision and autografting of deep partial and full thickness injuries. Particular attention in established treatment algorithms is afforded to key areas of mobility, durability, and cosmesis for these patients. Progressive and better-funded regions generally provide adjunctive physical and occupational therapy to patients who have suffered thermal injuries, whether conservatively or surgically managed, to ensure patients have the best long-term outcome.
the associated wound care may differ greatly. Patients from higher socioeconomic countries generally receive prompt burn wound care with comparatively early excision and autografting of deep partial and full thickness injuries. Particular attention in established treatment algorithms is afforded to key areas of mobility, durability, and cosmesis for these patients. Progressive and better-funded regions generally provide adjunctive physical and occupational therapy to patients who have suffered thermal injuries, whether conservatively or surgically managed, to ensure patients have the best long-term outcome.
Patients from lower economic countries struggle with these critical care issues on many levels. Care may be delayed as the patient seeks referral from the local primary care system. They often begin a long journey up the echelons of care to a facility capable of providing care for burn injuries while awaiting safe disposition, transportation, and stabilization. Such delays and barriers to care often result in longer times for the wounds to heal, or nonoperative strategies for patients who would have benefited from an operative approach to their burn injury. This prolonged inflammatory phase of ill-treated wounds results in slow and impaired healing—both considered major contributors to the development of pathologic scar formation. In many burn patients, a nonoperative approach to deeper burns, especially over the joints, neck, and digits, may lead to scarring, contracture, and a loss of function. Scars are long-standing and tend to be a chronic problem for each patient. Unless a scar is medically modified or surgically corrected, it may leave the patient with a lifelong disability ranging from purely cosmetic to ulceration, contracture, and loss of function.
The prevalence of scarring (cumulative total of all the individuals currently affected) is a more accurate method of discussing the scope of this problem than merely the incidence of new cases of scarring. As we have seen with burn data, scar data derived from higher socioeconomic countries are reasonably reported, whereas data from middle and lower socioeconomic countries remain sparse. In the developed world, it is estimated that 100 million people develop scars resulting from surgical procedures, burns, and injury.1 A total of 11 million patients developed cutaneous scar tissue resulting from elective operative procedures, whereas 25 million resulted from operations resulting from trauma. About 91% of postoperative patients reported a desire for improvement in the quality of wound healing along their surgical incisions,2 and 15% experience dissatisfaction with the healing of their wound resulting from an excessive or unaesthetic scar.
Scars are a heterogeneous group of problems affecting multiple human systems. The most obvious are cutaneous scars, but there are also internal counterparts that cause a significant portion of scar-related pathologic consequences (see Chapter 3). Scar tissue that forms after abdominal surgery leads to adhesions, complications of which include bowel obstruction, infertility in women, and chronic pain. A number of important facts emerged from a large meta-analysis, by Van Goor et al.,3 of the burden of adhesions in abdominal and pelvic surgery. The reported incidence of adhesive small bowel obstruction (SBO) was 2.4% overall, with a 4.2% incidence in pediatric patients, a 3.2% incidence in patients following lower gastrointestinal tract surgery, a 1.2% incidence following upper gastrointestinal tract surgery, a 1.5% incidence following urologic surgery, and a 1.4% incidence following laparoscopic surgery. The mean length of hospitalization for SBO was 7.8 days with a pooled hospital mortality of 2.5%. The incidence of chronic abdominal pain was 40%, with adhesions determined to be the etiologic agent of pain in 57% of the patients who underwent abdominal re-exploration.
Fibrosis adjacent to neural tissue may lead to alterations in sensory or motor function. Orthopedic joint injuries may result in scarring (arthrofibrosis), leading to decreased mobility and pain. Chronic scars may transform into a squamous cell cancer called Marjolin ulcer.4 This may be associated with any chronic inflammatory process including burns, venous stasis, trauma, pressure sores, and pilonidal abscesses.5 In addition to the physical problems caused by scar tissue, secondary problems may afflict the patient. These include pain, inflammation, pruritus, ulceration, and diminished range of motion. Contractures may physically limit the range of motion, or they may cause pain with motion, resulting in a decrease in the patient’s voluntary efforts to perform therapy and exercise (see Chapter 19). Scars may ulcerate along tension lines and form chronic wounds. The cosmetic appearance of the scar will affect the patient to varying degrees depending on scar location and the patient’s ability to cope with the scarring, the importance of which cannot be overstated.
In an ideal world, wound repair would more closely resemble a regenerative than reparative paradigm (see Chapter 27). Organisms that are able to accomplish regenerative wound healing are not hampered by scarring or even the loss of a limb; instead, they have the ability to grow new tissue that is equivalent functionally and aesthetically to the preinjured tissue. Regenerative healing is best demonstrated in lower vertebrates and early mammalian embryonic organisms. The sustained ability to maintain regenerative healing is lost with the progression to higher vertebrates. Examples of this include the salamander (tail regeneration), the newt (limb regeneration), or the zebra fish, which can heal wounds without evidence of scar tissue or loss of function.6 In the human species, there is documented scarless fetal healing that to an extent resembles this regenerative process (see Chapter 27). Unfortunately, near the end of the second trimester, regenerative healing is lost, and normal wound healing with the potential to form a scar commences.
The process of scar formation is an extension of the reparative wound healing process. On one end of the spectrum, scar tissue aids in wound closure by assisting in wound contracture and reepithelialization and contributing to wound strength. This wound bed has the capacity to amplify the inflammatory host response to accelerate closure, but it has the downside effect of readily forming aberrant scar tissue as a consequence (see Chapter 6). Perhaps, in order to increase the speed of wound healing, we have achieved a new equilibrium between regenerative and reparative wound healing whereby the compromise for quicker healing is a less-than-normal wound matrix.
The psychosocial aspects of scarring are multifactorial and may include symptoms of anxiety, fear of socialization and stigmatization, depression, and posttraumatic stress disorder (PTSD) (see Chapter 24). These symptoms are
difficult to quantify and treat, and may vary from patient to patient with similar physical manifestations of their scar tissue. Patient adaptability and coping are variables that help to mitigate psychosocial problems generated by scarring. Many consider the more highly visible scars as particularly problematic for the afflicted patient.
difficult to quantify and treat, and may vary from patient to patient with similar physical manifestations of their scar tissue. Patient adaptability and coping are variables that help to mitigate psychosocial problems generated by scarring. Many consider the more highly visible scars as particularly problematic for the afflicted patient.
Wound Healing
Understanding the normal wound healing process is critical to our understanding of the development of scar tissue, and is extensively discussed in subsequent chapters. Briefly, wound healing is a complex process classically described as consisting of a continuum. Three distinct, yet overlapping, healing phases are defined by (1) inflammation, (2) proliferation, and (3) maturation or remodeling.7 The inflammatory phase is characterized by two distinct processes: hemostasis and local wound debridement. Hemostasis in the wound bed is established by vasoconstriction and activation of the clotting cascade culminating in the formation of a fibrin clot. The subsequent release of cytokines and chemotactic factors recruits macrophages and neutrophils into the wound bed to phagocytize necrotic tissue, and generally occurs on days 3 to 4 postinjury.
The maturation of the wound bed to a more sterile environment is followed by the proliferative (second) phase of wound healing, which if unencumbered lasts approximately 10 days. Numerous stimulating growth factors, including vascular endothelial growth factor, platelet-derived growth factor, and transforming growth factor β, are released. As a result, there is replacement of the fibrin-based extracellular matrix (ECM) with neovascularization through angiogenesis and the establishment and deposition of granulation tissue. Migration and activation of fibroblasts facilitate the creation of new ECM composed of glycosaminoglycan, proteoglycans, and collagen in the wound bed. The ECM functions not only as a structural support but also as a critical element in cellular migration, integration, and promotion. Reepithelialization is traditionally thought to result from the migration of adjacent keratinocytes from both wound edges and adnexa such as follicular dermal buds. Normal physiologic wound contraction for closure is mediated by myofibroblasts. Wound edges of linear injuries are drawn together, while larger injuries are contracted circumferentially.
The final phase of wound healing, maturation and remodeling, is characterized by ECM alignment, remodeling of the collagen composition favoring type III, and apoptosis of senescent cells. At 4 months, the strength of a mature scar is approximately 80% of baseline, with most remodeling completed between 12 and 18 months after injury. This normal healing process is undertaken by a predominantly reparative rather than regenerative mechanism. Alterations of the wound bed may alter this process, leading to nonregulated healing, which may result in proliferative scarring. Factors such as severity of the wound, bacterial colonization counts, time to reepithelialization, and mechanical stress vectors may all play a role in the development of scarring (see Chapters 7, 8, and 9).8
Scar Characterization
How then to begin to objectively and comprehensively characterize the presence and effect of scar? Is it merely the histologic presence of scar that should be considered? Should one only consider visually evident scar formations—being raised and discolored—as significant? Scars can prove painful and dysaesthetic but may not be raised, tethered, or easily visualized. Certainly these all merit inclusion. Functional consequences should likely carry import: consider, for example, tendon adhesions resulting from closed fracture or infection. Certainly, scars are not merely a cutaneous manifestation or problem. One must merely consider the dire consequences of a postoperative uterine scar and its inherent risk of catastrophic rupture or ectopic pregnancy, or the formation of postmyocardial infarction scar and aneurysm formation to appreciate the holistic challenges and consequences of physiologic scar formation.
Disfigurement, or perhaps even enhancement, as characterized by the individual, culture, or the observer should be considered. How then to weigh these effects? Do certain populations figure differently in our assessment? Does one rate children more significantly? Do some cultures or individuals of a particular sex or economic status suffer more or less from deformity or functional loss? Economic, political, and social factors come into play. Access to medical, reconstructive, and rehabilitative care incurs its own cost-benefit analysis.
If we have difficulty defining what constitutes a scar and understanding when a scar is to be considered clinically, psychologically, economically, culturally, and physically relevant, then it is easy to appreciate how difficult it is to accurately assess its global impact. There is little doubt that countless individuals suffer worldwide from wounds of varied etiologic presentations. They may be related to diabetes and vascular disease; posttraumatic or surgical in origin; malignancy; radiation; associated with autoimmune disease; resulting from pressure; infection; idiopathic or genetic in origin. The costs to both society and the individual are staggering.
The history and challenge of problem scars is not a recent one (see Chapter 1). War, infection, and trauma have all tragically been experienced by all cultures and civilizations. Perhaps the earliest documentation available to us derives from Egyptian hieroglyphics with records of attempts to improve wound healing noted in both Mesopotamian and Egyptian texts. Biblical references abound with modern treatises well described by Linares, Pare, Lister, and many others.9
Scar Classification
The presentation of scars is highly variable, ranging from a simple, soft, flat, pale, asymptomatic linear scar seen some time after an uncomplicated laceration or surgical excision to a raised, firm, hyperpigmented, erythematous tumor associated with symptoms such as pain and itch (see Chapter 5). The simple flat linear scar in its best appearance will have the normal pigmentation of the host and represent the nearly perfect healing process from a linear cutaneous injury. If lateral tension is exerted on this wound, the scar may widen, resulting in a stretched appearance. Hyperpigmentation may occur and thinning of the scar is commonplace. Linear scars that remain in the inflammatory phase for longer periods of time may become hypertrophic.
There are three commonly described types of scars. They include simple, atrophic, and hypertrophic/pathologic (inclusive of HTS and keloids). Their histopathology, presentation, patterns of distribution, evolution, and involution are distinct. Simple scars result from cutaneous injury that heals well and within a relatively short time frame. The inflammatory process and the fibroproliferative phase of the wound healing are shortened. These scars tend to be flattened or only mildly raised, painless, and with pigmentation similar to the surrounding skin. They regress with time and fade into the surrounding tissue in the best of circumstances. A linear scar is flat and narrow and follows the path of cutaneous injury. A widespread scar is one that is stretched either longitudinally or widened, usually by mechanical forces during remodeling.
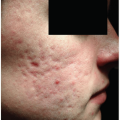
Atrophic scars occur when there is a focal loss, or loss of integrity, of the dermis and underlying subcutaneous tissue. Examples include abdominal stretch marks, or striae, that accompany trauma, obesity, or pregnancy and may occur without an epidermal injury, and depressed scars that follow significant trauma or inflammation, such as acne and varicella (chickenpox) (see Chapter 17).
HTS, as distinguished from keloids, are typically seen within the wound boundary and are associated with an accentuated or prolonged inflammatory phase. The scars are raised, widened, tender, painful, and pruritic, and follow a typical appearance pattern of erythema, violaceous, hyperpigmented, and then gradually fading toward normal color. The mean time to see the initiation of this type of scar is 4 weeks after epithelialization has occurred in the wound bed. Patients with a thermal injury have a much higher incidence of HTS than those with wounds resulting from surgery, trauma, or other etiologies. In burn patients, the mean time to initiate a HTS is 15 weeks after injury. The HTS has periods of evolution (growing and symptomatic) and periods of involution (resolution). Numerous factors act on these scars including the presence of mechanical stress, degree of inflammation, depth of injury, type of grafting and other treatment, and genetics. The final outcome of some HTS may not be known until 1.5 to 2 years after injury. HTS may become aggressive, especially if they complicate a mechanical stress line of the skin. These scars may contract and result in severe limitations of motion at specific joint areas. Efforts to control the growth of the HTS include pressure garments, silicone overlays, steroid injections, topical medication, and laser therapy (see Chapters 9, 10, and 13).10 On the cellular level, there are theoretical approaches targeting inflammatory mediators and epithelial-mesenchymal interactions and altering the physical environment.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree