Numerous times a day the average cosmetic surgeon will deal with patients who are unhappy with their aging. I tell these patients that “aging is a privilege denied to many.” What is equally important is how the patient is “handling” their aging. A 60-year-old patient who wants to look 30 is unreasonable, while a 60-year-old patient who wants to look as good as they can for 60, is very reasonable. A big part in a surgeon having good outcomes is picking the right patients. Cosmetic facial surgery is very popular in our culture and body dysmorphic disorder (BDD) is very prevalent. A normal and balanced cosmetic surgery patient can be a pleasure to work with. However, a patient with BDD can be a nightmare both clinically and legally. This type of patient cannot accept aging and their entire psyche revolves around narcissism and pathologic body image and wellbeing. Acquiring the ability to avoid this type of patient is a true skill.
Aging is a physiologic process of the body in the response to the passage of time. Since the beginning of time, people have sought treatments to retard or reverse aging, to no avail. Aging can be accelerated by both intrinsic and extrinsic factors and it cannot be stopped or reversed, but it effects can be mitigated.
It is imperative that cosmetic surgeons fully understand the pathophysiology of aging, and educating patients about aging helps them appreciate the process and basis for rejuvenation. Although we do know much about aging, in reality, we know relatively little. Most textbook descriptions of facial aging are very mechanical and relate to loss of volume and support. Although these are factors and important to aging reversal through cosmetic surgery, there are many other intrinsic factors that make aging happen.
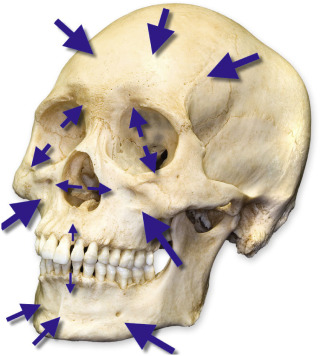
As most cosmetic facial surgery patients are female, the nuances of metabolic aging influences are significant. Menopause produces decreased estrogen levels with elevated androgen levels, which contribute to epidermal and dermal changes. The decrease in basal metabolic rates (in men and women) facilitates weight gain and fat distribution in unwanted places such as thighs, abdomen, hip, buttocks, face, and neck. Add the ravages of childbearing to the skin and muscle and it is easy to understand the aging process in females. Subcutaneous fat also decreases, which affects the support of the skin. The face and neck are rich in glandular structures, which are less frequently discussed in volume loss but are probably moderate contributors. Skeletal muscles can undergo 50% atrophy with aging, and osteoporosis plays a key role in bone resorption, as the majority of women in their fifth decade are osteoporotic. Osteoporotic changes also occur in males and in both sexes contribute to facial skeletal and dental resorption. As the facial skeleton shrinks, even more soft tissue support is lost ( Fig. 1.1 ). Bone in the aging face is more prone to resorption in specific areas such as the orbital rims, maxilla and piriform region and anterior mandibular and pre-jowl regions ( Fig. 1.2 ). In addition to this, ligamentous attachments from bone to soft tissue tether the overlying soft tissue and contribute to hollowing when bone loss drags down the soft tissue anatomy.

One unique factor to facial aging is that in most cultures the face is exposed. Clothes can masquerade somatic aging but the face, neck, and hands give it all away.
As with all other theories or processes, surgeons and anatomists argue about what exactly happens during aging. While most surgeons agree that atrophy, ligamentous laxity, and ptosis are causative factors, others argue against this. It is universally agreed, however, that aging is a gradual process of structural weakening and its clinical effects begin in the third decade and progress throughout an individual’s lifetime. Aging is basically a process of deflation similar in the transition from the grape to the raisin ( Fig. 1.3 ).

Babies and toddlers have full rounded faces with full convex contours. This is, in part, from the small skeleton supporting the generous fat compartments in infancy. Adolescence includes rapid but disharmonious growth of bone, cartilage, muscle, and fat, which produces a sometimes awkward appearance in the preteen years. Through the teen years, puberty produces secondary sexual characteristics including rapid growth phases, which produce hereditary but predictable and distinguishable facial changes. Middle age brings the onset of aging changes that progress until death (see below). The cycle of aging is such that infants have large orbits and smaller maxillae, which make their midfacial characteristics resemble an aged person. As the midfacial skeleton grows, the infant takes on the midface of youth. Continued aging produces widening of the orbits and maxillary and piriform resorption, which makes the aged person resemble an infant. Truly the cycle of life. While some parts of the facial skeleton resorb with age, some areas such as the mandible enlarge, underlining the multifactorial and dynamic changes that contribute to the aging facial skeleton.
The youthful face is tapered like an upside down egg, due to the distinct volume and tight tissue retention ( Fig. 1.4A ). The aging face is more of a reverse taper, similar to a right-side up egg, due to the descent of volume and fat compartment changes ( Fig. 1.4B ).

Aging changes are not only from volume loss and support changes but also due to intrinsic and extrinsic factors ( Box 1.1 ). It is interesting that biologic aging can sometimes exceed chronologic aging, and we all know 45-year-olds who look 60 or the inverse. Fig. 1.5A shows a career truck driver with obvious accelerated actinic damage on the driver’s side that is exposed to more sun and wind and Fig. 1.5B shows a 65-year-old female with both hereditary and acquired aging (intrinsic and extrinsic).
| Intrinsic aging factors | Extrinsic aging factors |
|---|---|
| Cellular senescence Decreased proliferative capacity Decreased cellular DNA repair capacity Chromosomal abnormalities Hormone reductions Gene mutation Hard, soft, and dental structure loss | Ultraviolet radiation Environmental factors (ozone, etc.) Tobacco use Ethanol abuse Gravitational effects Elasticity changes Emotional stress |

Lifestyle and hereditary factors are significant contributors to the aging equation. Some aging factors are controllable, while others are not. Studies of monozygotic twins have revealed that aging is affected greatly by environmental and lifestyle factors, as measured by physical appearance. The factors that exert the greatest influence seem to be substance or alcohol abuse, sun exposure, and emotional distress. These aging changes are shown with supporting images in the various procedure chapters. An excellent description of cutaneous aging is presented in Chapter 12 .
In the first textbook I wrote, Dr. Tom Faerber contributed a chapter on facial aging and performed an interesting study where he obtained computed tomography (CT) scans on his 9-year-old daughter, 42-year-old wife, and 75-year-old mother-in-law, to compare aging changes. Of particular note is that the youthful face is convex, while the aging face is concave due to fat atrophy, muscle atrophy, gravitational and ptotic changes ( Figs. 1.6–1.8 ). A pattern of muscle atrophy was demonstrated in the masseter and buccinators muscles in the oldest family member. The parotid gland maintained its volume, whereas the surrounding perimuscular and subcutaneous fat showed atrophy. Fat and muscle atrophy in the temporal, buccal, and malar regions were also seen and contribute to the concavities in those regions that develop with age, as evidenced in the progressive CT scans. This is evidence-based data that shows facial aging transformations from convex to concave. Although osseous volume loss is a big component of midfacial aging, some studies show osseous volume increases in the lower face.



Regional Facial Aging
The most logical means of addressing facial aging and rejuvenation is to start at the top and work downward in an orderly progression during the consultation, and discuss the diagnosis and treatment of each unit.
Skin
The most plentiful facial tissue is skin. The facial skin, like the exposed hands, rarely gets respite from the ravaging effects of the environment. Photodamage from sun exposure is especially harmful and, coupled with extrinsic factors such smoking, can accelerate the effects of aging.
Photodamage describes aging changes of the skin from chronic ultraviolet (UV) light exposure. Cumulative photodamage can be seen in almost every patient by comparing the sun-exposed and sun-protected areas of skin. The most obvious clinical cutaneous aging changes include markedly increased skin roughness, mottled hyperpigmentation, loss of elasticity, wrinkling, and sallowness.
Genetic contributions to skin aging result in numerous biochemical, histologic, and physiologic changes. These changes include a reduction of vascularity, increased dermal/epidermal thickness, collagen changes, proteoglycan and dermal cellularity, and loss of elastic fibers.
Photoaging causes functional and anatomic modifications in the exposed regions. Ultraviolet B (UVB) radiation produces direct damage on the DNA of skin cells and also modulates the activity of cytokines and adhesion molecules. Ultraviolet A (UVA) radiation initiates the formation of reactive oxygen species (ROS), which also damages nuclear and mitochondrial DNA and activates matrix metalloproteinases (MMPs).
Histologically, the effects of skin photoaging include epidermal thickening, keratinocyte atypia, loss of polarity, and increased melanogenesis ( Box 1.2 and Fig. 1.9 ). A fragmented and disorganized dermal fibrillar network is present and forms amorphous groups. Collagenous changes occur in the appearance of fragmented collagen fibrils, senescent fibroblasts, loss of function of glycosaminoglycans, and alterations in the cutaneous microvasculature.
- •
Thickened more basket-woven stratum corneum
- •
Thinner more atrophic epidermis
- •
Epidermal atypia
- •
Irregular melanin dispersion in the epidermis
- •
Decreased glycosaminoglycans in the dermis
- •
Abnormal-appearing elastic fibers in the dermis

Contributing to exogenous skin aging is the decrease in skin functions that occur with age. These include decreases in cell replacement, injury response, barrier function, sensory perception, immune and vascular responsiveness, thermoregulation, sweat production, sebum production, and vitamin D production. The dermis is thicker on areas of the face that are less mobile (e.g., forehead and nose) and thinner on areas of the face with increased movement (e.g., lower eyelids).
Upper Facial Aging
Hair
Aging in the scalp manifests as the pigment changes of graying, thinning, hair shaft fragility, pattern baldness, and recession. These changes are largely genetically controlled and less at the mercy of the environment compared with the skin. Additionally, “hair aging” is less of an indicator of age, as some 20-year-olds lose their hair, while some 70-year-olds have a full head of thick hair.
The aging scalp is treated surgically with follicular grafts, flaps, etc. More recently, robotic-assisted transplantation has become popular and is eliminating the need for large occipital scalp scars from harvest. The medical treatment of hair loss, although in its infancy, may overcome surgical treatments in the lifetime of many of the readers of this text. Bimatoprost (Latisse, Allergan Inc., Irvine, CA) is a glaucoma medication that has been scientifically shown to make eyelashes thicker, darker, and longer, and at the time of this writing, is in clinical trials for scalp hair growth. Minoxidil is a topical alopecia treatment drug that produces vasodilation of the hair follicle. Patients taking this drug for blood pressure developed increased hair growth as a side-effect and this was eventually accepted by the Food and Drug Administration (FDA) for pattern baldness. Finasteride is a medication taken in tablet form originally used to treat benign prostatic hypertrophy. It is a 5-alpha (5α)-reductase inhibitor, which blocks the conversion of testosterone to dihydrotestosterone, the latter being toxic to hair. This drug is FDA approved for male pattern baldness only and causes birth defects in pregnant females.
Forehead and Brow
Younger people have smooth foreheads. Photodamage with the resultant skin changes, tissue ptosis, osseous changes, and gravity contribute to brow and forehead changes.
Although some people, even in youth, never have elevated or arched brows, many do. Most youthful females have brows that arch at the junction of the central and lateral brow (which corresponds to the lateral pupillary limbus). The youthful male brow lies at or slightly above the superior orbital rim. Due to the aging changes, coupled with the atrophic changes in the brow fat and upper periorbital complex, the brows descend in many people. This manifests as lateral hooding and or generalized ptosis, which gives the appearance of smaller eyes ( Fig. 1.10 ). In severe cases, the eyebrow sits on the lashes. A ptotic brow associated with the upper periorbital changes produces a sad and tired appearance. Due to this, many females go through their waking hours subconsciously raising their brows, which further compounds the problem of flexed muscles and brow skin wrinkling. Any surgeon who performs browlift surgery can attest to the difficulty of getting some females to relax their brow for a preoperative photograph, or when looking in a mirror.











