Abstract
Complications in dermatologic surgery range from inconsequential to life-threatening and from unpredictable to entirely avoidable. Bleeding, infection and poor wound healing are of particular concern. Thorough preoperative assessment, careful pre- and postoperative planning, and meticulous technique increase the probability of a successful procedure.
Keywords
surgical complications, wound healing, postoperative infection, postoperative bleeding, hypertrophic scar, prophylactic antibiotics
- ▪
A thorough preoperative assessment of the patient is required to increase the probability of a successful outcome for any surgical procedure
- ▪
Attention to detail, selection of the simplest procedures that will produce the desired result, and meticulous intraoperative technique will prevent many complications
- ▪
Anticipation of avoidable complications and careful management of unavoidable ones optimize results
- ▪
Clear communication between patient and surgeon must begin before the start of the procedure and continue through every stage, including the recovery and healing phases
- ▪
Because many complications do not manifest until several days to months postoperatively, patients must be monitored periodically to ensure that all parties are satisfied with the final outcome
Introduction
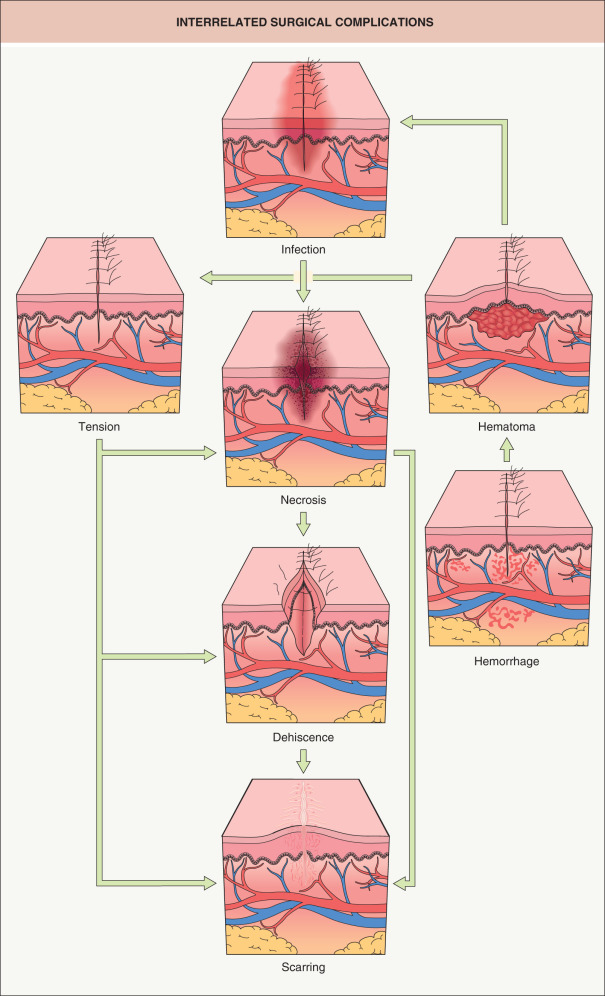
“To complicate” means to make intricate and/or difficult. Surgical complications are deviations from the original planned outcome, usually occurring as the result of multiple interrelated events ( Fig. 151.1 ) . Complications in dermatologic surgery are uncommon , but they do occur. However, with careful planning and meticulous attention to technique, many potential complications can be avoided or minimized.
Complications vary, from threatening a patient’s life to worsening their cosmetic appearance. Life-threatening emergencies in cutaneous surgery are rare, but the surgeon must be prepared to deal with such problems as cardiac arrhythmias and anaphylaxis. Proper, well-maintained resuscitation equipment must be readily available, and the staff should maintain Basic Life Support training, including the use of an automated external defibrillator (AED). Physicians in offices where extensive cutaneous surgery is performed should also have Advanced Cardiac Life Support training .
The surgeon should conduct a thorough preoperative assessment, including history and directed physical examination, to identify pre-existing conditions that may affect the patient’s ability to heal. Informed consent obtained at this time, and again just prior to the procedure, ensures that the patient has realistic expectations. This education may minimize future misunderstandings regarding known risks of the procedure.
Prevention of an unsatisfactory outcome starts during the planning stage, then continues with good intraoperative surgical technique and careful postoperative care. Anticipation of avoidable complications and management of unavoidable ones optimize the results. Throughout the process, it is essential to involve the patient in his or her own care.
Discussion
Preoperative Assessment
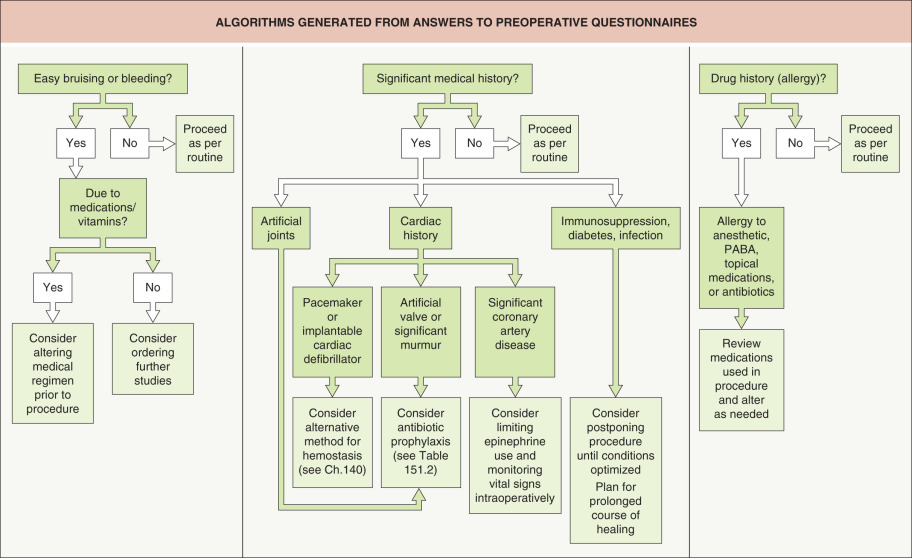
A thorough preoperative assessment is an invaluable tool for identifying conditions that could lead to surgical complications. A simple one-page preoperative questionnaire can be completed by the patient, with help from the medical staff as needed, at the time of the initial evaluation. “Yes” or “no” answers to specific questions can indicate a need for further evaluation or for a change in the operative plan ( Fig. 151.2 ).
Potential for bleeding
Although some bleeding is expected during any surgical procedure, excessive bleeding is a common complication. The discovery of a bleeding disorder prior to surgery allows for correction of the condition if it is reversible, or changing plans for surgery if it is not. The bleeding disorder may be due to abnormalities in the coagulation cascade (inherited deficiencies in coagulation factors, as in hemophilia), platelets , or both . Platelet issues can be subdivided into problems with production (leukemia, myelosuppressive drugs), survival (idiopathic thrombocytopenic purpura, disseminated intravascular coagulation), or function (drugs, Hermansky–Pudlak syndrome).
Laboratory evaluation
If the history does not suggest a bleeding disorder, and the patient is otherwise well, laboratory testing is usually unnecessary. Appropriate screening tests should be checked if there is a suspicion of a hereditary or acquired bleeding disorder. A platelet count identifies only a quantitative problem. The bleeding-time test measures platelet function, but determining the time it takes for small cuts on the forearm to cease bleeding is operator-dependent. An in vitro bleeding-time assay, the platelet function analyzer 100 (PFA-100), provides an easy method for rapidly assessing platelet function. Unlike the bleeding time, the PFA-100 can be performed on a collected blood specimen. It is useful in detecting platelet defects, most cases of von Willebrand disease, and the effects of aspirin and other antiplatelet agents . Additional standard screening tests include a PT (prothrombin time) test, which can determine a defect in the extrinsic clotting pathway, and an aPTT (activated partial thromboplastin time) test, which can determine a defect in the intrinsic pathway . The international normalization ratio (INR) is discussed in the next section.
Medications and supplements
A review of medications and nutritional supplements should be a part of the preoperative assessment. Antiplatelet and anticoagulant medications are of particular importance. When they are prescribed for cardiac or neurologic indications, their discontinuation can potentially lead to serious events (e.g. coronary artery stent thrombosis). In general, surgeons should not discontinue these medications but should instead focus on intraoperative precautions, such as meticulous hemostasis and minimal undermining . For complex cases, consultation with the prescribing physician and/or a hematologist can be considered, especially if patients are taking newer agents where less information may be available.
Aspirin and aspirin-containing products are well-documented sources of bleeding problems. Platelet aggregation is irreversibly affected when the aspirin acetylates cyclooxygenase. One aspirin affects a platelet throughout its 6- to 10-day lifespan. If patients are taking aspirin for general health benefits, rather than specific medical indications, then they may discontinue the aspirin from ≥10 days before until 5–7 days after surgery. Nonsteroidal anti-inflammatory drugs affect the same enzyme, though the block is not as severe or irreversible . If possible, the patient should stop these medications 1–4 days prior to surgery, depending on the half-life of the drug.
Dipyridamole suppresses platelet aggregation by inhibiting phosphodiesterase and increasing cyclic adenosine monophosphate (cAMP) levels within platelets. It is used in combination with aspirin for secondary prevention of thromboembolic events. The antiplatelet effect of dipyridamole is less than that of aspirin, and it does not appear to increase bleeding complications .
Thienopyridines (e.g. clopidogrel , ticlopidine , prasugrel ) irreversibly inhibit platelet aggregation via inhibition of P2Y 12 , a platelet ADP receptor. Cilostazol is a selective type 3 phosphodiesterase inhibitor with weaker P2Y 12 inhibition; it is typically used for claudication. Normal platelet function usually returns 5–7 days after discontinuing these medications. Although there is a slightly increased risk of complications in patients receiving P2Y 12 inhibitors, these medications can typically be continued without significant issues .
Warfarin is a commonly used anticoagulant. Several studies have been published in the vascular, oral, orthopedic and dermatologic surgery literature supporting the viewpoint that surgery can be performed without stopping warfarin. An international normalization ratio (INR) should be checked just prior to surgery. Most authors advocate an upper limit of 3 or 3.5 . The safety of dermatologic surgery with INRs >3.5 has not been well studied, though one study found a poor correlation between bleeding complications and INR levels, with complications also occurring in the setting of in-range INRs . If warfarin is discontinued, in consultation with the prescribing physician, it should be held for 4–5 days preoperatively. Bridging with low-molecular-weight heparin should be considered. If a patient on warfarin develops significant postoperative bleeding, the anticoagulation can be reversed with one or more of the following: oral or intravenous vitamin K, fresh frozen plasma, and four-factor prothrombin complex concentrate.
The oral direct thrombin inhibitor dabigatran , as well as the factor Xa inhibitors apixaban and rivaroxaban , are increasingly being used as alternatives to warfarin and are referred to as NOACs (novel oral anticoagulants; see Table 22.8 ) . Literature remains sparse regarding these agents in dermatologic surgery. One large randomized trial of invasive, non-dermatologic procedures found similar rates of bleeding complications with warfarin versus dabigatran, but both medications were held preoperatively . The authors would take similar intraoperative precautions with these medications (see above). Idarucizumab is an approved therapy for reversing dabigatran and andexanet is a specific antidote for apixaban and rivaroxaban, but this is less of an issue because of their shorter half-lives of ≤12 hours.
Heparin is given parenterally and acts as an antithrombin factor. When administered intravenously, unfractionated heparin has a short half-life of approximately 1 hour and can be rapidly reversed by intravenous protamine sulfate. Low-molecular-weight heparin (LMWH) has a half-life of 3–5 hours and is administered subcutaneously, typically in an outpatient setting. Either form can be used to bridge patients in whom discontinuing warfarin preoperatively has been deemed necessary. LMWH is discontinued 24 hours prior to surgery, whereas unfractionated heparin is stopped five hours preoperatively. Either form of heparin is then restarted, together with warfarin, 24 hours post-procedure, with the heparin discontinued after a therapeutic INR has been attained .
Studies have shown that vitamin E in doses of 200–400 IU per day reduces platelet adhesion. Patients with abnormal platelets, such as diabetics and renal dialysis patients, who are treated with vitamin E have decreased platelet aggregation. The effect is synergistic when vitamin E is taken with other antiplatelet agents. Garlic decreases platelet aggregation and significantly increases fibrinolytic activity at a dose of 900 mg/day. Eicosapentaenoic acid (fish oil) decreases platelet aggregation and adhesion and increases bleeding time. Many other dietary supplements such as dong quai, licorice, devil’s claw, and danshen have effects on coagulation (see Table 133.3 ) . Patients should discontinue these supplements prior to surgery.
Ethanol is a potent vasodilator. It also inhibits platelet aggregation and platelet granule release as well as accentuating the increase in bleeding time caused by aspirin . In addition, excessive alcohol consumption may decrease the patient’s attention to optimal wound protection. Patients should be advised to avoid alcohol consumption during the immediate perioperative period.
Wound healing
The principles of wound healing are covered in detail in Chapter 141 . To forestall complications due to poor wound healing, close attention should be paid to pre-existing medical conditions and medications that affect wound healing. If the patient is a brittle diabetic, is suffering acutely from congestive heart failure, has uncontrolled hypertension, or has a myriad of other severe conditions, postponing surgery may be a wise decision. If the procedure cannot be postponed, the patient should be forewarned that the postoperative healing phase could be prolonged. In addition, any chronic debilitating illness may predispose patients to secondary infections.
Medications such as systemic corticosteroids may also delay healing and predispose the patient to secondary infections. Patients on other immunosuppressive medications such as cyclosporine may also be prone to infections and prolonged healing. Inhibitors of vascular endothelial growth factor (VEGF), including monoclonal antibodies (e.g. bevacizumab ) as well as oral tyrosine kinase inhibitors (e.g. sorafenib ) have been associated with delayed healing and wound dehiscence. These agents should be held for at least 4–6 weeks prior to surgical procedures .
Cigarette smoking interferes with wound healing, and flaps or grafts are particularly susceptible. This effect is dose-dependent, with heavier smokers having an increased risk of postoperative necrosis compared to lighter- and non-smokers . Ideally, patients should avoid all smoking for at least 3 weeks before surgery, but one study found that over 85% of smokers continued smoking preoperatively despite instructions to stop. At a minimum, patients should be strongly encouraged to decrease consumption to less than half a pack per day or switch to nicotine replacement patches for at least 2 weeks preoperatively and 1 week postoperatively . Compared to cigarettes, the patches do not result in the high peak blood nicotine levels that can lead to peripheral vasoconstriction and reduced wound tissue oxygen tension.
There is literature to support delaying procedures in patients who are currently receiving or have recently completed isotretinoin therapy, because of poor wound healing and the formation of excessive granulation tissue. In keloid fibroblast cultures, retinoids were observed to modulate connective tissue metabolism. Most reported problems have been individual case reports involving resurfacing procedures after courses of isotretinoin for acne therapy. It may be prudent to postpone cosmetic procedures in such patients for up to 1 year after the cessation of isotretinoin . However, more recent data from larger cohort studies suggest that procedures, including laser hair removal, dermabrasion, and laser resurfacing for acne scars, may be safe to perform during or shortly after a course of isotretinoin therapy .
Reactivation of a herpes simplex virus (HSV) infection can dramatically interfere with the postoperative course. Patients with a history of herpes labialis or other facial herpetic infections should receive prophylactic antiviral therapy prior to dermabrasion, laser resurfacing, chemical peels or surgery involving known trigger area(s). Antiviral therapy, such as oral acyclovir 200 mg five times a day, should start 2–5 days prior to the procedure and continue for 5 days postoperatively or until the skin has re-epithelialized . Regimens consisting of oral famciclovir 250 mg three times daily or oral valacyclovir 1 g twice daily can also be utilized, as they have more convenient dosing which can increase compliance.
The shoulders, central chest, upper arms and upper back are more prone to the development of hypertrophic scars, keloids, and spread scars. The patient should be counseled before surgery about the increased risk of scarring in these areas.
Prophylactic antibiotics
Antibiotic prophylaxis is administered to prevent surgical site wound infection, bacterial endocarditis, or infection in implanted prosthetic devices. The risk and consequences of infection must be weighed against the risk and cost of the antibiotic.
Wounds are placed into four general categories ( Table 151.1 ). The majority of dermatologic surgical procedures are clean or clean-contaminated and do not need prophylaxis. However, prophylactic antibiotics may be helpful in certain clean-contaminated wounds. For example, antibiotics should be considered for procedures involving the oronasal mucosa, axilla, or genitourinary and gastrointestinal tissues. In addition, procedures that approach the ear canal may be at higher risk for infection with Gram-negative organisms. Long procedures are also more likely to develop wound infections: the infection rate almost doubles with each hour of operation. Prophylactic antibiotics should be considered for procedures involving the lower extremities as well as more complicated procedures such as wedge excisions of the lip or ear, flaps on the nose, and all grafts . Antibiotics are therapeutic, not prophylactic, for contaminated and infected wounds; in such cases, a bacterial culture is helpful to guide the antibiotic regimen.
| WOUND CLASSIFICATION | ||
|---|---|---|
| Class | Attributes | % that develop infections |
| Clean | Immaculate technique Non-inflammatory | 1–4 |
| Clean-contaminated | Small breaks in technique Gastrointestinal, respiratory or genitourinary tracts entered without gross contamination | 5–15 |
| Contaminated | Major breaks in technique Gross contamination from gastrointestinal, genitourinary or respiratory tracts | 6–25 |
| Dirty and/or infected | Wound with acute bacterial infection ± pus | >25 |
When considering antibiotic prophylaxis, two special patient groups should be addressed: (1) those at risk for infective endocarditis; and (2) those at risk for bloodborne infection of total joint replacements ( Table 151.2 ) . In patients with total joint replacements or specific cardiac diseases, no antibiotic prophylaxis is indicated if the surgical procedure, along with an uncomplicated repair, is in a non-infected cutaneous site. In general, prophylactic antibiotics are no longer recommended by the American Academy of Orthopedic Surgeons and American Dental Association for patients with prosthetic joint replacements undergoing dental procedures; possible exceptions, including mucosal incision in a patient with a history of joint surgery complications, are outlined in Table 151.2 . However, to date, recommendations specific to dermatologic procedures are lacking. Table 151.3 summarizes suggestions for antibiotic prophylaxis regimens. If any question arises, consultation with the patient’s cardiologist, internist or orthopedic surgeon may prove helpful.
| ANTIBIOTIC PROPHYLAXIS FOR DERMATOLOGIC SURGERY – PATIENT GROUPS AT RISK FOR INFECTIVE ENDOCARDITIS AND INFECTION OF TOTAL JOINT REPLACEMENTS |
| High-risk cardiac conditions (infected skin or breach of oral mucosa) |
|
| Prosthetic joint replacements (infected skin, breach of oral mucosa ** ; non-infected site at high risk of surgical site infection ** ) |
|
* First 6 months after procedure (surgical or catheter intervention).
** The American Academy of Orthopedic Surgeons (AAOS) and American Dental Association no longer recommend the general use of prophylactic antibiotics in patients with prosthetic joints undergoing dental procedures, but they can be considered for patients with a history of complications associated with their joint replacement surgery who are undergoing procedures such as gingival manipulation or mucosal incision ; however, to date, there are no AAOS recommendations specific to non-infected, high-risk sites.
| RECOMMENDATIONS FOR ANTIBIOTIC PROPHYLAXIS IN PATIENTS AT RISK FOR INFECTIVE ENDOCARDITIS AND INFECTION OF TOTAL JOINT REPLACEMENTS | |||
|---|---|---|---|
| Surgical site/procedure | Allergy | Antibiotic | Dose † |
| Non-oral – wedge excisions of lip or ear, nasal flaps, all grafts | None | Cephalexin * or dicloxacillin * | 2 g PO |
| – or – | |||
| cefazolin/ceftriaxone * | 1 g IM/IV | ||
| Non-oral – wedge excisions of lip or ear, nasal flaps, all grafts | Penicillin | Clindamycin or azithromycin/clarithromycin * | 600 mg PO 500 mg PO |
| – or – | |||
| clindamycin | 600 mg IM/IV | ||
| Oral mucosa breached | None | Amoxicillin | 2 g PO |
| – or – | |||
| cefazolin/ceftriaxone or ampicillin | 1 g IV/IM 2 g IV/IM | ||
| Oral mucosa breached | Penicillin | Clindamycin or azithromycin/clarithromycin | 600 mg PO 500 mg PO |
| – or – | |||
| clindamycin | 600 mg IM/IV | ||
| Lesions in the groin or on the legs | None | Cephalexin * or TMP–SMX DS | 2 g PO 1 tablet PO |
| – or – | |||
| ceftriaxone * | 1–2 g IV | ||
| Lesions in the groin or on the legs | Penicillin | TMP–SMX DS or levofloxacin * | 1 tablet PO 500 mg PO |
| – or – | |||
| clindamycin and gentamicin | 600 mg and 2 mg/kg IV | ||
* In communities with increased risk for methicillin-resistant Staphylococcus aureus , consider prophylaxis with TMP–SMX DS (1 tab PO) or clindamycin (600 mg PO).
† Give single dose (PO, IM or IV) 30–60 minutes before procedure.
Defibrillators and pacemakers
The electrosurgical instruments often used in cutaneous procedures have the potential to interfere with the function of pacemakers and implantable cardioverter-defibrillators (ICDs), though the risk is quite low with modern devices (see Ch. 140 ) . In patients with these devices, alternatives to electrosurgery may be considered. Battery-operated and AC-powered thermal cautery units have been used successfully in dermatologic surgery. They do not produce high-frequency electromagnetic interference or electrical currents traversing the body. Bipolar instruments concentrate the current across the tips, minimizing the chance of interference. If conventional electrosurgery is used, the active tip should not be applied within 15 cm of the implanted device whenever possible. Electrocoagulation should also be kept at as low a setting as possible, and it should be delivered in bursts lasting <5 seconds in order to minimize the chance of prolonged inhibition .
In consultation with the patient’s cardiologist, the ICD can be deactivated for the duration of the procedure. The pacemaker can also be placed in a fixed rate, rather than sensing, mode to minimize the possibility of interference. During the procedure, if conventional electrosurgery is used, continuous cardiac monitoring with an ECG and pulse oximeter can be considered. A contingency plan should be in place to deal with an arrhythmia should it occur, and an AED should be immediately available. If the device is deactivated or its function altered for the procedure, it is the surgeon’s responsibility to ensure that the patient returns to his or her cardiologist within a reasonable time period for readjustment and evaluation. Electrical equipment should be properly grounded during the procedure. If bipolar forceps or true electrocautery are used, intraoperative monitoring, cardiology consultation, and postoperative evaluation are unnecessary for most patients .
Allergies
True allergic reactions to local anesthetics may be type I (immediate) or type IV (delayed-type hypersensitivity) (see Ch. 143 ). Patients who have a type IV sensitivity to one major group of local anesthetics (ester or amide) are usually not allergic to members of the other group. Type I reactions are more commonly associated with the ester anesthetics and their para-aminobenzoic acid (PABA) metabolite. Although the lack of cross-reactivity between ester and amide anesthetics is true for type IV sensitivity, it has not been adequately studied for anaphylaxis. If there is a possible history of a type I amide allergy, referral to an allergist for a progressive challenge protocol can be considered to identify a suitable amide anesthetic . It is also important to consider the possibility that the allergic reaction is due to the preservative (e.g. methylparaben, metabisulfite) and the use of preservative-free anesthetics can resolve this problem.
Epinephrine (adrenaline) is a vasoconstrictive agent commonly added to local anesthetics because it lessens bleeding and prolongs the duration of anesthesia. Patients will occasionally report a history of an “allergy” to local anesthetic, describing their symptoms as palpitations, headache, tachycardia, tachypnea, or tremor (see Ch. 143 ). Such reports likely represent reactions to epinephrine given in high dosages or inadvertently injected intravascularly. Since the half-life of epinephrine in serum is short, specific therapy for these reactions is usually not necessary. In order to avoid them, the lowest dosage and concentration of epinephrine (<1 : 100 000) should be used, and injection of significant amounts intravascularly should be avoided using proper infiltration technique .
Another commonly encountered systemic side effect often mistaken as an allergic reaction is the vasovagal reaction. The patient recalls becoming pale, sweaty and lightheaded, perhaps even fainting. He or she can become hypotensive, but in contrast to a true toxic or allergic reaction, the pulse is slow and regular ( Table 143.2 ). No loss of bowel or bladder control or prolonged tonic–clonic movements occur unless the patient has a seizure secondary to brain hypoxia during the vasovagal reaction. Treatment consists of keeping the patient supine or in the Trendelenburg position and giving reassurance. Once the patients have recovered, they can gradually sit up and ambulate .
Chlorhexidine gluconate is a frequently utilized surgical skin preparation (see Table 146.6 ). It is a broad-spectrum antibacterial of the halogenated phenol class. Though it has a very weak sensitizing potential, it has been reported to cause allergic contact dermatitis . Similar reactions have also occurred with the iodophor povidone-iodine (Betadine ® ) . Both compounds can also be skin irritants, especially when occluded. Care must be taken to remove all traces of the skin cleanser prior to application of the dressing.
Topical antibiotics can cause allergic contact dermatitis. Although neomycin is the most common sensitizer, bacitracin can also cause sensitization. Co-reactivity against both neomycin and bacitracin is common. Cross-sensitivity between neomycin and gentamicin, kanamycin, streptomycin and tobramycin can also occur. Mupirocin or erythromycin ointment are alternatives if the patient is allergic to both neomycin and bacitracin. As there is no convincing evidence that topical antibiotic ointments prevent infection, plain petrolatum ointment may be the best agent for wound dressing.
Informed consent
The lines of communication should be open between the surgeon and the patient before the procedure begins. The physician should make the patient aware of his or her condition, how it affects overall health, if treatment is imperative, and what treatment options are available. Pros and cons of surgery as well as alternative therapies should be discussed in a language the patient can easily understand. To assess how much the patient understands, it helps to ask the patient to describe the procedure in his or her own words. The patient should also be informed about the risks of the procedure and the reasonably expected results. Common complications (e.g. bleeding, infection, allergic reactions, scarring) should be addressed and strategies for dealing with them discussed. In turn, the patient must accept responsibility for preoperative preparation and postoperative wound care.
It is the surgeon’s responsibility to provide oral and written, clear, detailed information delineating the indications for the procedure and describing the procedure, the risks involved, and the postoperative care necessary to ensure the best outcome possible. Should complications arise, as they inevitably will, the surgeon should be honest with the patient about treatment options and outcome.
Intraoperative Considerations
Contamination
The risk of infection in cutaneous surgery is very low. Two often-cited studies estimated the risk at 2.3–2.4% , but more recent data suggest the rate is likely <1% . The indications for prophylactic antibiotics were discussed previously. Although wound infections usually do not become evident until 4–8 days postoperatively, in most cases the infection truly begins at the time of surgery. The surgical team should prepare the skin and the surgical field, prepare the instruments, and wear the correct protective equipment to reduce the incidence of infection and protect both the patient and caregivers.
The skin cannot be sterilized, but the majority of the resident flora and pathogenic bacteria can be removed by using mechanical cleansing and antiseptic agents. The extent of skin preparation varies with the invasiveness and complexity of the proposed surgical procedure. A 2-second wipe with 70% isopropyl alcohol or a 10-second cleansing with an iodophor swab may be adequate for superficial biopsies . Chlorhexidine is the most frequently utilized preoperative preparation for skin surgery. It produces rapid bacterial destruction, is effective against a wide range of Gram-positive and Gram-negative bacteria, and binds with the protein of the stratum corneum, providing residual action. However, chlorhexidine is irritating to the conjunctiva, and it may be toxic to the cornea or tympanic membrane and middle ear; caution must be exercised in these areas. Iodophors are another excellent antiseptic; one advantage is that the prepared area is readily apparent because of the brownish-orange color. They are effective against Gram-positive and Gram-negative bacteria and some fungal spores, but iodophors have a slower and shorter duration of action than chlorhexidine. Also, as noted earlier, they can cause irritant or allergic contact dermatitis.
The preparation and sterilization of surgical instruments is covered in Chapter 144 . Use of a surgical mask may help protect the patient from surgical personnel with active upper respiratory tract infections. The mask protects the surgical team from contamination by saliva droplets or blood from the patient. It is also essential to protect the eyes from accidental splashes of body fluid. Appropriate surgical attire and glove use is advocated in all surgical situations as part of universal precautions. In cases where sterility is not essential, such as superficial shave biopsies and electrodesiccation and curettage, non-sterile examination gloves can be used. Recent data suggest that Mohs surgery can be performed as a clean procedure with low infection rates .
For all surgical procedures, proper handling of sharps is essential. Needles should never be recapped and blades should not be changed by hand. Despite best intentions, needlestick injuries may still occur, and surgeons must have a plan for testing and treatment when appropriate ( Table 151.4 ). The current recommendations for treating needlestick injuries are available online from the National Institute for Occupational Safety and Health or from the Clinicians’ Post-Exposure Prophylaxis Hotline (PEPline) at 1-888-448-4911.