Splinting
Rebecca von der Heyde
Patricia M. Paytner
I. Chronic Pain Syndromes
Chronic Regimal Pain Syndrome (CRPS) I/II
A resting hand splint in the position of function provides support to the hand, wrist, and thumb and limits painful motion. The splint is worn as needed between exercise and functional activities. A circumferential night splint, preferably of a soft material, can provide positive pressure and facilitate pain management. When pain is controlled, low force dynamic splinting can be used to increase joint range of motion.
II. Flexor Tendons
A. Flexor Tendon Repair in Zones I to V
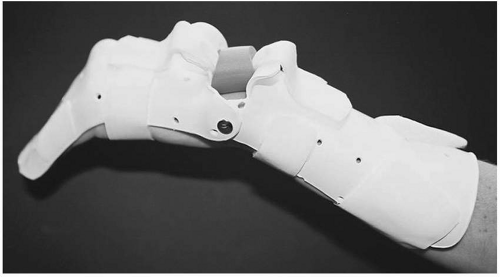
A dorsal-based synergistic wrist splint is recommended following flexor tendon repair in zones I to III (Fig. 39.1). The MP joints are positioned in more than 60 degree flexion, with the PIP and DIP joints in full extension. The wrist is immobilized in 20 degrees of flexion, but is allowed up to 30 degrees extension during place and hold exercises initiated within 2 to 3 days following surgery. The combination of wrist and digital motion as afforded by this protocol produces high excursion/low force rehabilitation. Repairs in zones IV and V are managed using a traditional, dorsal blocking splint. Splints are worn at all times for the first 4 to 6 weeks.
III. Extensor Tendons
A. Mallet Finger
A static DIP extension splint is worn at all times for 6 to 8 weeks to facilitate scarring of the terminal tendon to the distal phalanx (Fig. 39.2). The fabrication of at least two splints is suggested to allow the application of a dry splint after showering to prevent maceration.
B. Boutonniere and Pseudoboutonniere Injuries
Injuries to the central slip are managed using finger-based PIP extension splints, worn at all times for 6 to 8 weeks. The inclusion of DIP flexion exercises while in the splint will facilitate dorsal translation of the lateral bands.
C. Sagittal Band Rupture
A hand-based, MP extension splint (P1 blocking splint) immobilizes and aligns the MP joint in full extension and neutral ab/adduction (Fig. 39.3). Active motion of the PIP and DIP is allowed while in the splint. Buddy taping to the finger on the involved side is permissible for partial tears and in later stages of healing to control active motion.
D. Proximal Zones
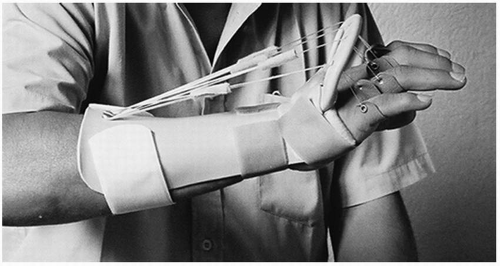
A dynamic MP extension assist splint allowing 30 degrees of active MP flexion is the preferred method of treatment following extensor tendon repairs in zones V to VII (Fig. 39.4). This protocol facilitates distal glide of the healing tendon to decrease adhesion formation. These injuries can also be treated more conservatively using a forearmbased, static MP extension splint; however, theses splints have been demonstrated as less effective in preventing extensor lags. Splints are worn at all times for the first 4 weeks.
E. Chronic Boutonniere Deformity
Dynamic PIP extension splints are utilized to increase joint mobility in the patient with a chronic boutonniere. These splints can be fabricated in various ways; however, excellent prefabricated options are also available.
F. Chronic Swan Neck Deformity
Oval splints are fabricated to decrease PIP hyperextension and reinforce the volar plate (Fig. 39.5). In addition, silver ring splints can be custom ordered for the patient to provide an attractive, long-term option.
IV. Tendinopathy
A. de Quervain Tenosynovitis
A forearm-based thumb spica splint with the IP joint free is fabricated to decrease the combined motions of thumb flexion/adduction and wrist ulnar deviation. The splint is worn for 6 to 8 weeks to decrease pain and inflammation of the first dorsal compartment. As immobilization of the thumb often decreases function, positioning of the thumb in palmar abduction to ensure opposition to the index and long will increase compliance with splint wear.
B. Trigger Finger
Hand-based P1 blocking splints (Fig. 39.3) have been suggested to control active triggering. Blocking of the MP joint should be tested to determine symptom relief prior to splint fabrication. If successful, splints are worn for 6 weeks to decrease tendon inflammation.
C. Intersection Syndrome
A forearm-based thumb spica splint with the wrist positioned in slight extension and the thumb IP joint free is fabricated to decrease irritation of the muscles of second dorsal compartment. The splint is worn for 6 to 8 weeks to decrease repetitive wrist motion and inflammation of the radial wrist extensors.
D. ECU Tendonitis
A wrist cock-up splint is recommended to decrease pain and inflammation. An ulnar gutter splint that does not encompass the fingers is an additional option if pressure over the ulnar head does not provoke pain. Splints are typically worn for 6 to 8 weeks during functional tasks.
E. FCR Tendonitis
A wrist-resting splint in a neutral position (Fig. 39.6) provides relief to the patient with FCR tendonitis. Splints are typically worn for 6 to 8 weeks during functional tasks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree