Brachial Plexus
Donald A. Bae
Terry Myckatyn
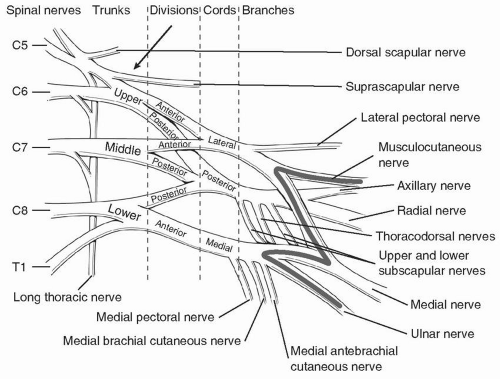
I. Anatomy (Fig. 18.1)
The brachial plexus typically arises from the C5 to T1 nerve roots, though anatomic variations are frequent. “Prefixed cords,” in which there is contribution of C4 to the plexus, occur in up to 40% of cases. “Postfixed cords,” in which there is contribution from the T2 nerve root, may be seen in up to 4% of patients.
The brachial plexus is divided into five segments: roots, trunks, divisions, cords, and nerves. (The pneumonic “red trucks drive cats nuts” may be useful.) The C5 and C6 nerve roots join to form the upper trunk. The C7 root continues as the middle trunk. The C8 and T1 roots join to form the lower trunk. Each trunk then divides to form the anterior and posterior divisions. The anterior divisions of the upper and middle trunks coalesce to form the lateral cord. The anterior division of the lower trunk continues on as the medial cord. The posterior divisions of all trunks join to form the posterior cord. The terminal nerve branches arise from these cords. The lateral cord becomes the musculocutaneous nerve. The posterior cord gives rise to the axillary and radial nerves. The medial cord becomes the ulnar nerve. The median nerve arises from branches off the medial and lateral cord (the so-called M of the brachial plexus).
Other nerve branches arise more proximally from the brachial plexus. Notably, the long thoracic nerve arises from the C5 to C7 nerve roots. The suprascapular nerve arises from the upper trunk. The lateral pectoral nerve arises from the lateral cord. The medial pectoral, medial brachial cutaneous, and medial antebrachial cutaneous nerves arise from the medial cord. The thoracodorsal nerve as well as the upper and lower subscapular nerves arise from the posterior cord.
During surgical approaches, the brachial plexus may be explored in the posterior triangle of the neck (borders are sternoclidomastoid, the trapezius and the clavicle) between to the anterior and middle scalene muscle bellies. After dissection through the skin, platysma, and underlying fascia, the scalene muscles may be found just posterior to the sternocleidomastoid muscle. The phrenic nerve, typically found on the anterior surface of the anterior scalene, serves as the “lighthouse to the brachial plexus” and may be traced proximally to its origin from the C3 to C5 nerve roots, leading the surgeon to the C5 nerve root and brachial plexus. The inferior belly of the omohyoid muscle is another useful anatomic landmark; the upper and middle trunks lie superior to the omohyoid, and the inferior trunk and subclavian vessels lie inferiorly. As the divisions, cords, and terminal branches lie inferior to the clavicle, clavicular osteotomy or mobilization may be needed to expose the entire plexus.
The ganglia lie close to the spinal cord, though the motor neuron cell body lies within the cord itself. Therefore, “preganglionic” lesions refer to ruptures or avulsions of the neural elements from the spinal cord. Several nerves arise in close proximity to this area, including the sympathetic chain, phrenic nerve,
long thoracic nerve, and dorsal scapular nerve, which are assessed in the evaluation of these patients.
The brachial plexus is intimately associated with the subclavian and axillary artery and vein throughout. The cords are named according to their location with respect to the second portion of the axillary artery posterior to pectoralis minor.
Congenital Brachial Plexus
I. Definition
Brachial plexus birth palsy (BPBP) refers to traction or compression injury to the brachial plexus sustained during birth resulting in neurological impairment and upper extremity paralysis.
II. Epidemiology
The incidence of BPBP is estimated to be 1 per 1,000 live births. Despite advances in obstetrics, prenatal medicine, and rising Caesarian section delivery rates, the incidence may be increasing in more developed nations.
Risk factors include
Macrosomia (>4,500 g)
Difficult or prolonged labor
Shoulder dystocia
Multiparous pregnancy
Vacuum or forceps assisted delivery
History of prior delivery resulting in BPBP
III. Classification
BPBP may be classified according to the character of the neurological injury or anatomic pattern of plexus involvement. The Seddon and Sunderland classifications (e.g., neurapraxia, axonotmesis, and neurotmesis) may be used. Neurotmesis injuries may be described as nerve root avulsions from the spinal cord or “preganglionic” injuries versus extraforaminal or “postganglionic” ruptures at the root or trunk level.
BPBP may also be characterized based upon the nerve roots involved.
Classic Erb palsy refers to C5-6 involvement, typically at the level of the upper trunk at “Erb point.”
A Klumpke paralysis denotes C8-T1 involvement. Total plexus involvement may also be seen.
The Narakas classification system has been used to categorize typical patterns of involvement.
Group I refers to C5-6 palsies (˜46% of patients).
Group II refers to C5-6-7 involvement (˜29%).
Group III denotes a flail upper extremity (total plexus involvement) without an associated Horner syndrome.
Group IV refers to a flail extremity with Horner syndrome.
IV. Natural History
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree