Sarcoidosis
Elyse M. Love
Evan Rieder
BACKGROUND
Sarcoidosis is a systemic, idiopathic inflammatory condition with skin involvement in up to one-third of affected patients. Cutaneous involvement may include the skin, oral mucosa, and/or nails. Systemic involvement most commonly affects the lungs, but it may affect virtually any organ system.
PRESENTATION
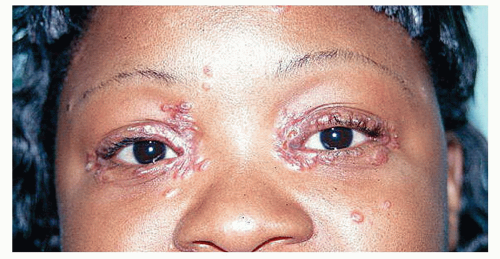
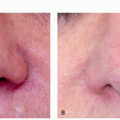
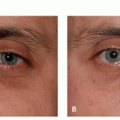
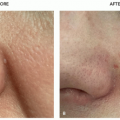
Cutaneous sarcoidosis may be the first symptom of sarcoidosis or may present after the diagnosis of systemic sarcoidosis has been established. Over 20 morphological variants of cutaneous sarcoidosis exist, including papular, psoriasiform, annular, lichenoid, plaque, atrophic, scarring, and verrucous. Classically, sarcoidal lesions are red-brown symmetric papules and plaques, with a predilection for the face, especially the nasal ala, periocular, and perioral regions (Figure 14.6.1). Larger plaques may also be seen on the neck, upper trunk, and extremities. Lesions may be arcuate in distribution or follow patterns of trauma. Presentation of red-brown papules within a scar and/or tattoo is highly suspicious for sarcoidosis. Telangiectasia may be prominent.
Pressure with diascopy may turn red-brown papules into an “apple jelly” color, but this may be difficult to perceive in patients with Fitzpatrick skin types V and VI. Lesions may also appear hypopigmented, ichthyosiform, micropapular, psoriasiform, and/or ulcerative. The nails and oral mucosa may also be involved.
Sarcoidosis has a bimodal distribution with incidence peaks from 25 to 35 years of age and again from 45 to 65 years of age. In the United States, sarcoidosis has a higher incidence in individuals of African descent when compared with other races. Worldwide, sarcoidosis
has the highest incidence in Sweden and the United Kingdom.
has the highest incidence in Sweden and the United Kingdom.
More than half of patients experience remission within 3 years of diagnosis and two-thirds experience resolution within a decade of diagnosis.
DIAGNOSIS
Clinical Diagnosis
Sarcoidosis is a diagnosis of clinical exclusion, requiring clinicopathologic correlation of suspicious lesions. A thorough review of systems should be obtained in any patient with a new diagnosis of sarcoidosis, as systemic sarcoidosis can affect essentially any organ system. The most common organ systems of involvement include the lungs (90%-95% of systemically affected patients), which may present with dyspnea and/or a nonproductive cough; the bone marrow, which may present with leukopenia or anemia; and the heart (25%), which may present with arrhythmia or sudden death.
At the time of diagnosis, patients should be referred to primary care for a thorough physical examination; cardiology for electrocardiogram, echocardiogram, and possible Holter monitoring; pulmonary for chest x-ray and pulmonary function testing; and ophthalmology. Of note, ocular sarcoidosis may be asymptomatic and lead to blindness.
Appropriate laboratory testing includes complete blood count, comprehensive metabolic panel, urinalysis, and thyroid function; 25-hydroxyvitamin D, 1,25-dihydroxyvitamin D3, and angiotensin-converting enzyme (ACE) levels; as well as tuberculin skin testing or QuantiFERON gold.
ACE levels are elevated in approximately 60% of patients and correlate with disease activity. Despite correlation, ACE levels should not be used to make diagnosis owing to the high prevalence of elevated ACE levels in nonaffected control populations. Instead, this serological marker may be used to monitor disease activity.
Histopathology
Diagnostic biopsy can be performed on cutaneous or internal lesions. For cutaneous biopsy, a punch biopsy should be performed when sarcoidosis is suspected. A shave biopsy is of limited clinical utility owing to the deep dermal nature of sarcoidosis and its differential diagnostic entities.
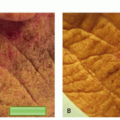
Pathology classically shows superficial and deep epithelioid granulomas without a surrounding inflammatory infiltrate (“naked granulomas”). Because sarcoidal granulomas can also be seen in infection and foreign body granulomas, stains should be performed to rule out infection and polarizable material. However, the presence of polarizable material does not rule out sarcoidosis, as up to 20% of sarcoid lesions contain birefringent material on histopathology.1
Subtypes
Lesion morphology may hint to systemic disease.
Lupus Pernio
Lupus pernio describes erythematous to violaceous, scaly papulous nodules and plaques that occur on the cheeks, lips, forehead, nose, and ears. About 75% of patients with lupus pernio have lung involvement; 50% have involvement of the upper respiratory tract.
Darier-Roussy
Darier-Roussy describes sarcoidosis limited to the subcutaneous fat (panniculitis) and is often associated with systemic disease. It presents with asymptomatic, subcutaneous nodules or plaques without overlying epidermal changes.
Lofgren Syndrome
Lofgren syndrome is the acute presentation of sarcoidal lesions, erythema nodosum, fevers, hilar adenopathy, and arthralgias. When presenting concurrently with sarcoidosis, erythema nodosum portends an acute, transient, and more favorable course. Lofgren syndrome is associated with spontaneous resolution in 1 to 2 years.
Differential Diagnosis
The polymorphous presentation of sarcoidosis lends itself to a broad differential diagnosis depending on the primary morphology of the lesions.
Other Annular Dermatoses
Granuloma annulare
Annular lichen planus
Annular elastolytic giant cell granuloma
Annular mycosis fungoides
Erythema annulare centrifugum
Interstitial granulomatous dermatitis
Nodular tertiary syphilis
Borderline leprosy
Foreign Body Granulomatous Reactions
Zirconium
Beryllium
Silica
Tattoo ink
Soft-tissue filler
Of note, up to 20% of sarcoid lesions contain birefringent material on histopathology; therefore, this should not exclude the diagnosis of sarcoidosis.
Infectious Granulomatous Diseases
Mycoplasma
Deep fungal infections
Other Inflammatory Granulomatous Dermatoses
Granulomatous rosacea
Cutaneous Crohn disease
Granulomatous mycosis fungoides
Hodgkin disease
Blau syndrome
Cheilitis granulomatosa
Sarcoidal reaction to underlying lymphoma
PATHOGENESIS
It is postulated that disease development occurs in genetically susceptible individuals after exposure to an unknown triggering antigen. Debate continues as to whether the triggering antigen is created from autoimmune mechanisms or an external exposure, such as infection.
TREATMENT
The primary treatment of sarcoidosis involves localized or systemic corticosteroids; however, procedural modalities have been employed. Algorithm 14.6.1 outlines the treatment of sarcoidosis.
Medical
Corticosteroids
Topical, intralesional, and systemic corticosteroids are the primary medical treatment of sarcoidosis, depending on the number and severity of organ involvement. When systemic involvement is present, therapy will require multidisciplinary coordination with the most affected organ system driving therapy course.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree