Key points
• The visible surgical result is related to the soft tissue envelope and not the underlying skeletal structures that support the facial surfaces and volumes.
• Predicting how a procedure will change the skeletal framework is simple; forecasting how it will affect the soft tissues is hard.
• Biological soft tissues are anisotropic—that is, the mechanical properties are not the same in all directions.
• Viscoelasticity of the facial soft tissues is not linear, meaning that it does not show constant deformation for a given change in stress.
• New finite element models speed the model preparation by using a generic mesh that can be rapidly adapted to any patient improving prediction of soft tissue responses to skeletal movements.
• The ultimate goal is the ability to reverse engineer the result, whereby the surgical planning begins with the desired final facial form. The patient and surgeon determine the optimal soft tissue facial result, and then the surgeon repositions the skeletal elements to achieve the desired predicted result.
Introduction
The shape of the human face is determined by its skeleton and soft tissue cover. A good analogy is a sofa, whose shape is determined by its frame and padding. As the look of a sofa can be changed by modifying its structural frame, a face can be altered by reshaping its underlying skeletal framework.
Surgeons who move the facial bones know that their operations change their patients’ appearances. Predicting how a surgery will change the skeletal framework is simple; forecasting how it will affect the soft tissues is hard. Bone is a solid material that undergoes minimal distortion when it takes force. The skin, fat, fascia, and muscle are soft materials that deform easily. How the facial envelope will be altered when the underlying skeleton is changed depends on the overall structure of the soft tissues and the mechanical properties of each of its elements.
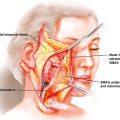
Unlike the padding of a sofa, the soft tissue cover of the face is elaborate. Its five layers are made of different types of tissues, each with its own biomechanical properties. The top mantle is made of skin. Underneath, one finds fat—subcutaneous. Lower, a fibro-muscular layer includes most of the muscles of facial expression. Deeper, one finds a thick layer, whose composition varies across the face. In front of the ears, the layer contains the masseter muscles and the parotid gland. In the malar region, the layer has fat pads. And in the labial and buccal spaces, one finds the deep muscles of facial expression (mentalis and buccinator). The deepest layer is made of the periosteum and the mucosa. The periosteum covers bone; the mucosa lines the inner aspects of the cheeks, lips, nose, and eyelids.
Adding to the complexity is the fact that the soft tissue envelope anchors itself to the skeleton in some areas (e.g., malar and masseteric region), while it is free in others (e.g., lips and cheek).
As mentioned earlier, how the soft tissue cover of the face will be deformed when the skeleton is altered also depends on the mechanical properties of each of its elements. Biologic soft tissues are viscoelastic, meaning that they have both viscous and elastic properties. Viscosity is resistance to flow. Honey is viscous compared with water because it flows slower than water when poured. Elasticity is the ability of a material to return to its original shape once a deforming force has been removed. A rubber band is elastic because it quickly regains its shape when the pulling force is let go.
When we press a viscoelastic body with one of our fingers, it deforms slowly with time, like viscous matter. When we lift our finger, however, the body recovers its shape, like an elastic material, but slower.
Another reason why predicting soft tissue deformation is hard is that biologic soft tissues are anisotropic —that is, the mechanical properties are not the same in all directions. For example, the skin has a different stiffness when it is stretched parallel to the Langer lines than when it is stretched perpendicular to them. Moreover, the viscoelasticity of the facial soft tissues is not linear, meaning that it does not show constant deformation for a given change in stress.
Soft tissue simulation methods
Over the years, experts have formulated different ways of predicting how skeletal surgeries will change soft tissues. Some predictions use rules of thumb derived from observations, some use statistical models, and some use the laws of physics.
Ultimately, the soft tissue predication utilizes historical data to drive algorithms with varying degrees of sophistication. The simplest algorithm is the two-dimensional (2D) historical approach of comparing postoperative lateral cephalograms with preoperative cephalograms. The changes in soft tissue anatomic landmarks are then expressed as ratios based on changes in the skeletal landmarks. There is a wide variation in the literature that is reported in the soft tissue response, depending on the quality of the historical records and variation in the population studies. , The experienced surgeon will typically consider these as quality changes in a particular patient with the understanding that such variability can be applied. These rules of thumb are summarized in Box 9.1 . However, when one applies a similar approach with today’s capabilities in capturing the changes in three-dimensions (3D) as with orthognathic surgery, the simplistic ratio-based approach becomes difficult because of the bewildering array of ratios that can describe the change in each landmark. Simplistic sagittal and vertical changes that can be measured in two-dimensional cephalograms now require vectors in the 3D space. Thus changes in surface area and volume are more accurate descriptors of the effect of the skeletal surgery in 3D space and require a more sophisticated approach.
Rules of thumb ,
With chin advancement
The labial sulcus deepens
Soft tissue pogonion moves forward at a nearly 1:1 ratio with the skeletal pogonion
With mandible sagittal advancement
The labial sulcus becomes shallower
The lower lip becomes less prominent
The labial sulcus at the B point moves forward at a ratio of 1:1
The soft tissue pogonion moves forward at a ratio of 1:1
The lower lip and vermilion border move forward at a ratio of 0.6–0.8:1
With maxillary sagittal advancement
the upper lip pout is decreased
the vermilion thins
the vermilion advances at a ratio of 0.40-1:1
the subnasale advances at a ratio of 0.20-0.70:1
the nasal tip advances at a ratio of 0.15-0.30:1
the nasolabial angle becomes more acute
the alar bases widen
the perialar region becomes fuller
Simulation systems that use physics divide the whole soft tissue volume into many smaller volumes of simple geometry, creating a soft tissue mesh. The smaller volumes are usually polyhedrons (3D solids with flat faces, straight edges, and sharp corners). Some systems divide the soft tissue envelope into polyhedrons that look like pyramids (tetrahedron) or into polyhedrons that look like cubes (hexahedron) ( Fig. 9.1 ). Within the soft tissue mesh, neighboring elements (polyhedrons) share faces, edges, and corners. The corners are key features because they are the nodes for which the algorithms calculate the soft tissue changes (displacement). The deepest nodes of the mesh represent either the periosteum or the oral mucosa. The most superficial nodes make the surface of the skin. In between nodes are different tissues layers.
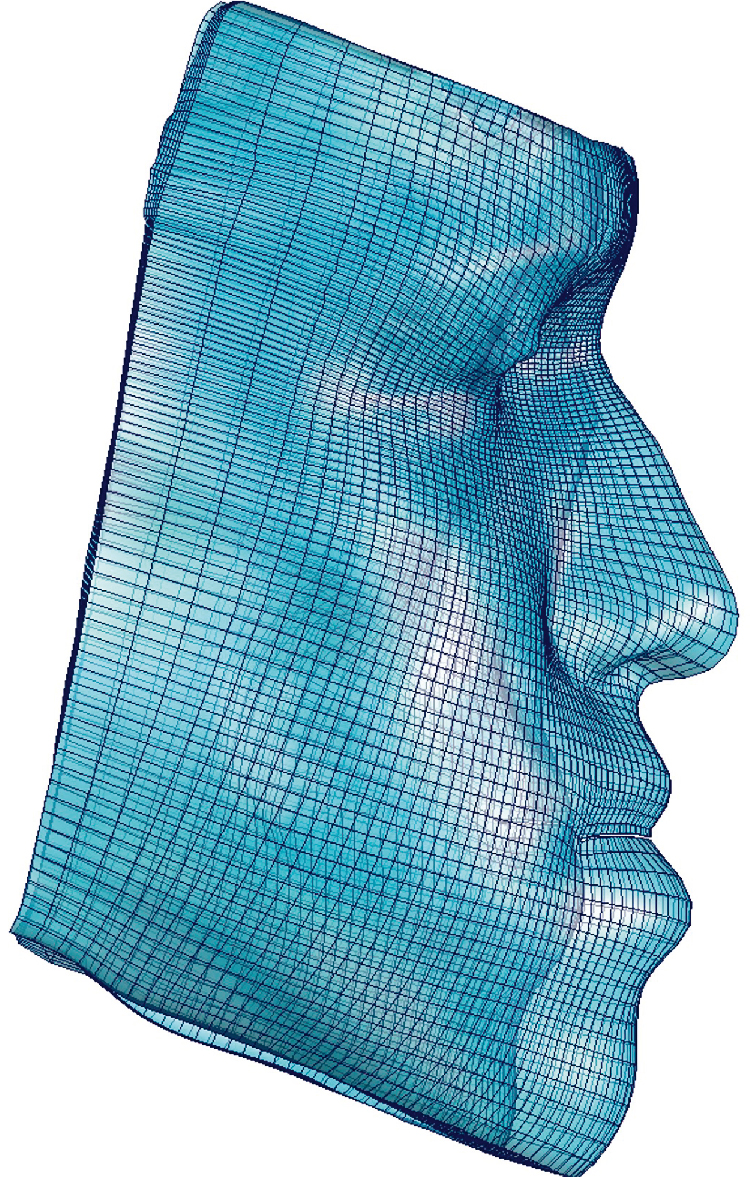
After a mesh has been created, a system of mathematical equations is added to the mesh to estimate how each soft tissue node will move given a certain amount of bone displacement. Three different physical models have been used: (1) mass-spring models, (2) mass-tensor models, and (3) finite-element models.
Mass-spring model
In a mass-spring model, the corners (nodes) of the polyhedra are connected to each other by virtual springs. Springs are selected because their actions obey a very simple mathematical equation:
displacement=forcespring stiffness
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree