Key Points
- ▪
The chest radiograph is predominantly useful to detect/characterize the pulmonary vascularity as influenced by congenital shunt lesions, such as pulmonary vascular shunt plethora of larger shunts and signs of pulmonary hypertension complicating large shunts.
- ▪
Small shunt lesions are not evident on chest radiography, other than pulmonary arteriovenous malformations.
- ▪
A minority of shunt lesions are directly suggested by chest radiography, such as the vertical vein of left-sided anomalous pulmonary venous return, the “scimitar sign” of the scimitar variant of right-sided anomalous pulmonary venous return, and ductal calcification.
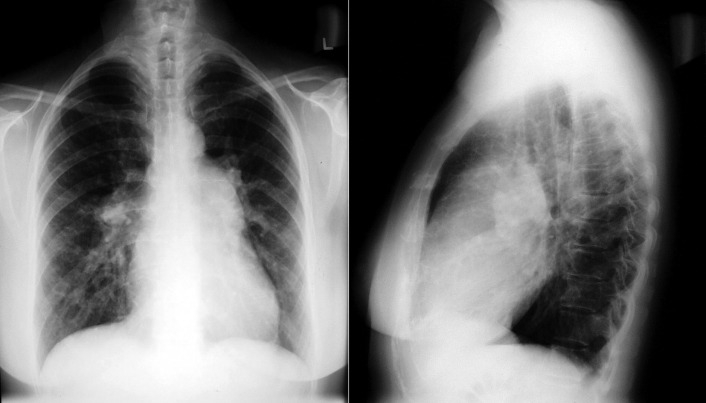
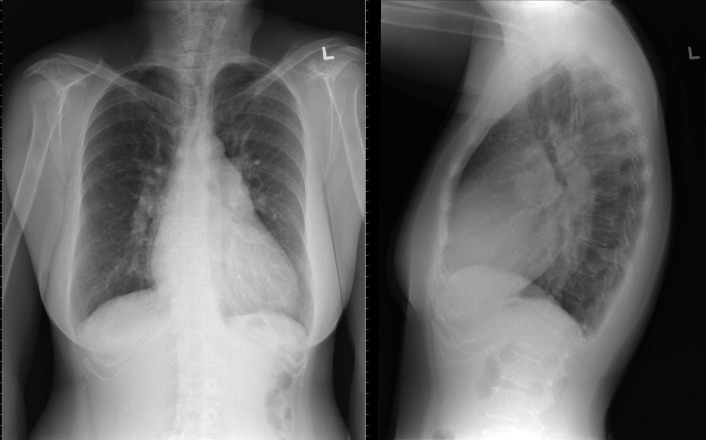
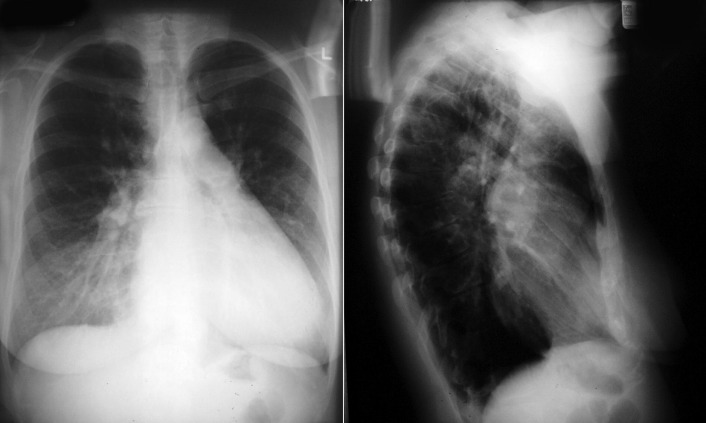
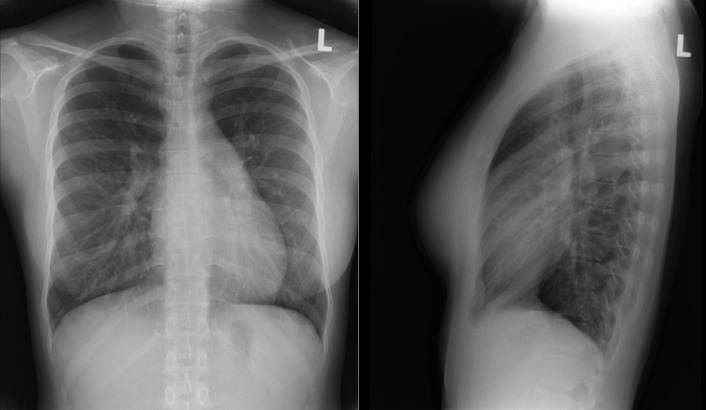
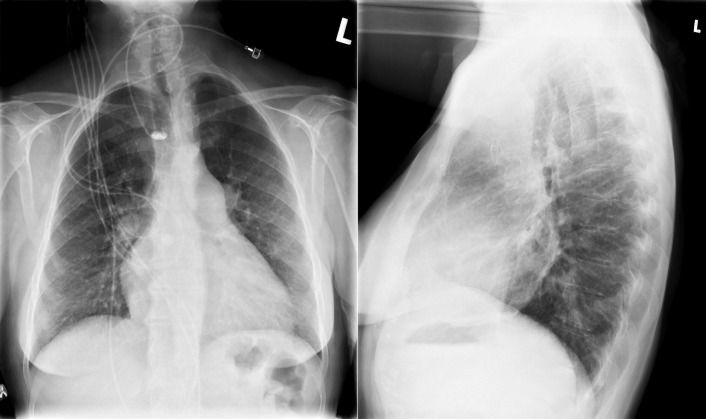
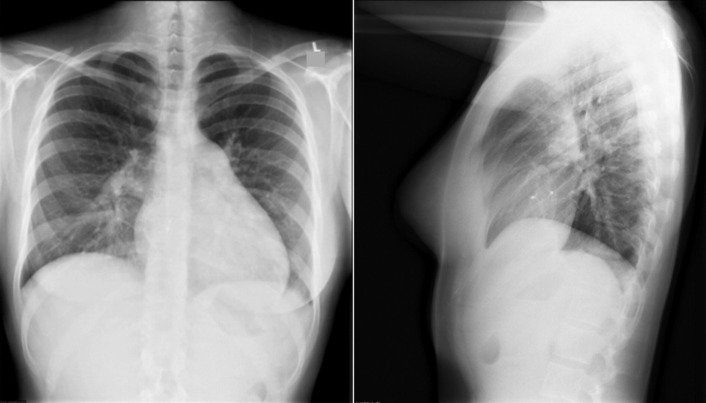
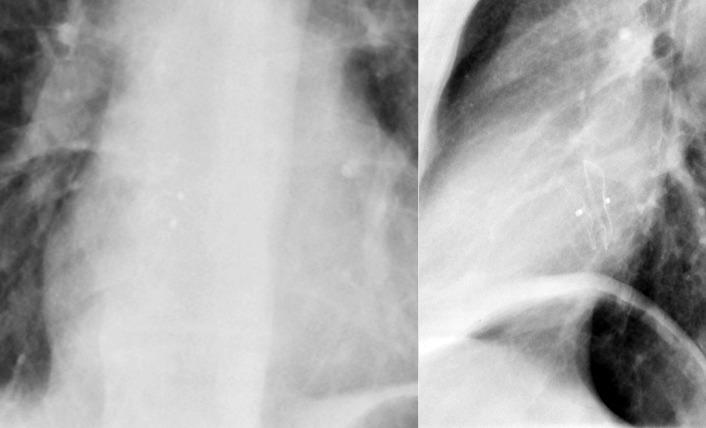
Left-to-right shunts initially result in volume overload of the chambers carrying the shunt volume, causing enlargement of the volume-overloaded chambers and an increase in pulmonary blood flow. If the amount of pulmonary blood flow is sufficiently high, obliterative disease of the pulmonary arterioles develops (“pulmonary vascular disease”), resulting in pulmonary hypertension. The chest radiographic appearance of pulmonary hypertension is one of centralization of pulmonary flow and accelerating enlargement of the right-sided chambers.
The size of a shunt is represented best by the shunt ratio (volume of blood through the pulmonary circuit vs. the systemic circuit, such as 2:1, 3:1, 4:1) and by the degree of elevation of the pulmonary pressures.
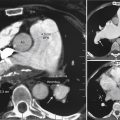
Patent Foramen Ovale
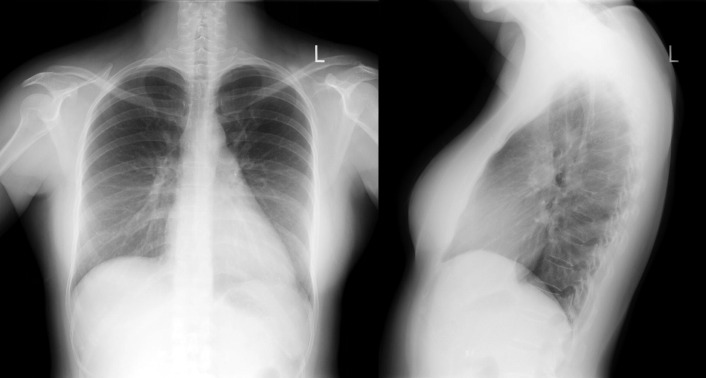
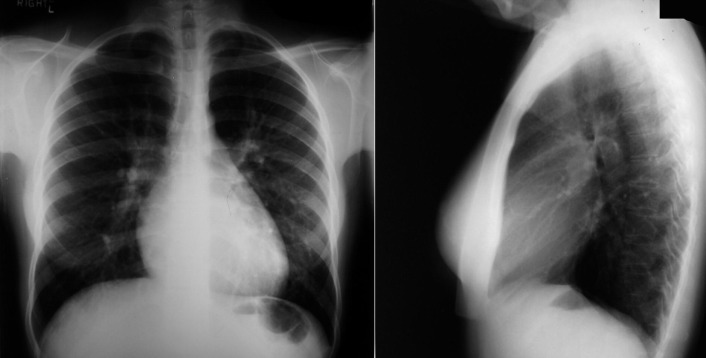
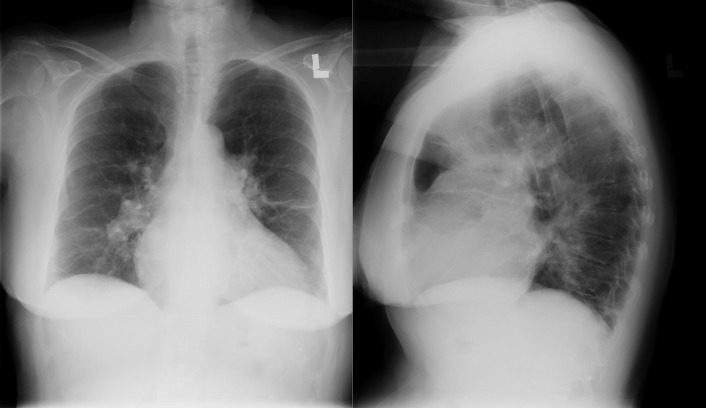
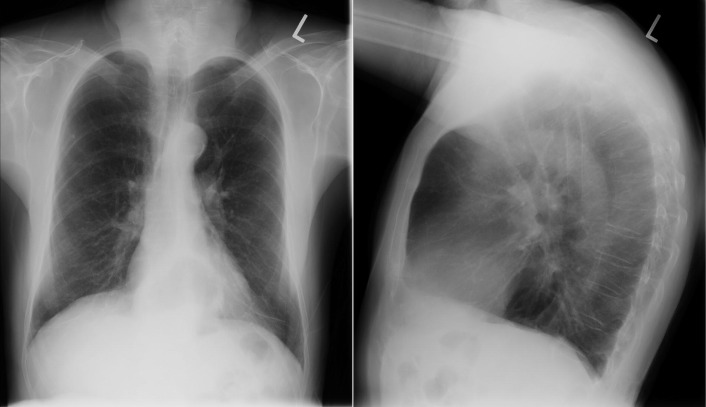
A patent foramen ovale is present in 25% to 30% of the adult population ( Figs. 18-1 to 18-4 ). Any magnitude of shunting across it in normal circumstances is undetectable radiographically. Percutaneous patent foramen ovale closure devices are fairly commonly inserted and are radiographically evident.
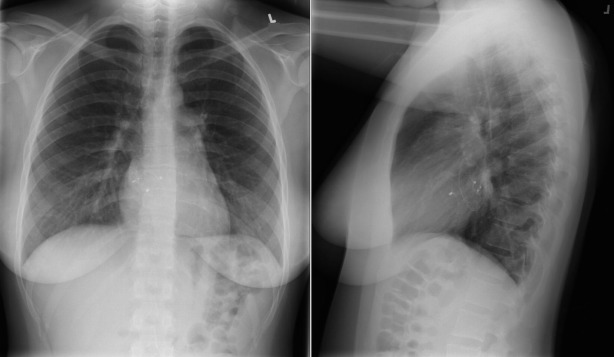
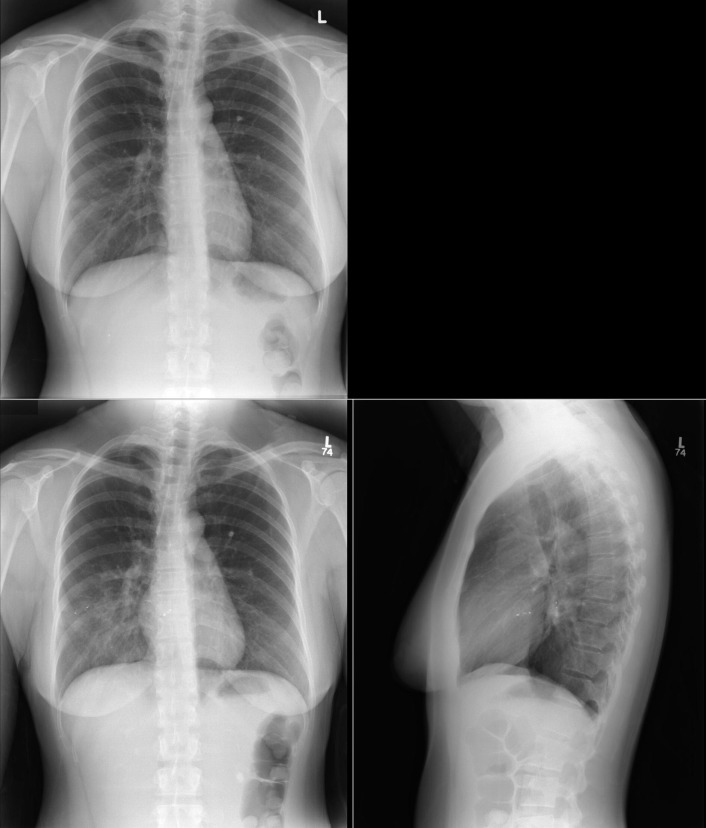
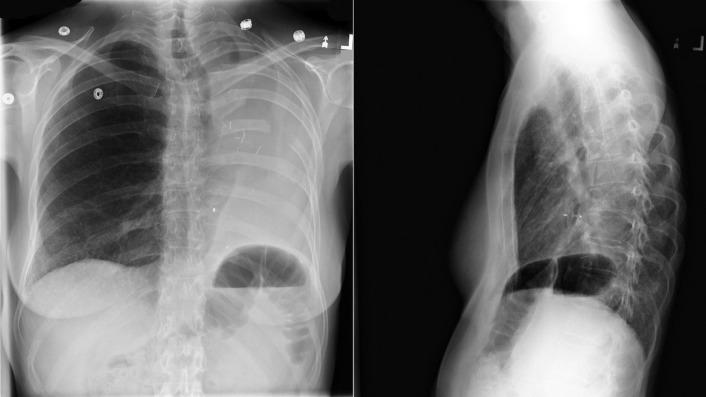
Atrial Septal Defect
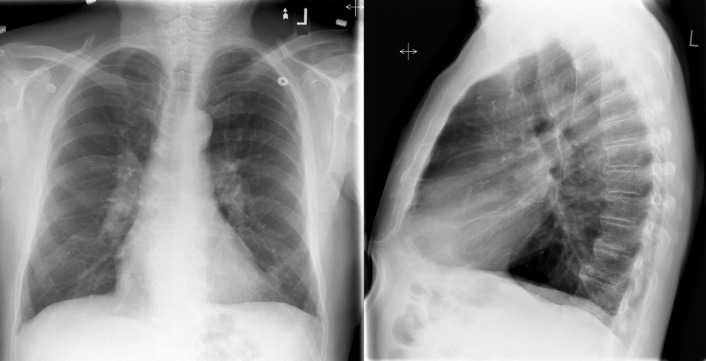
See Figures 18-5 to 18-31 . Possible findings are discussed in the following sections.