Abstract
The word purpura is derived from the Latin word for “purple,” a clinical characteristic that helps to differentiate the lesion from erythema, which is red. Blanchability is the clinical sign that best distinguishes the two. Purpura is nonblanchable because the blood is extravasated outside the vessel walls.
- 1.
Purpura (Latin purple) is extravasated blood outside blood vessels and therefore does not blanch
- 2.
Distinguish palpable from nonpalpable purpura
- 3.
Palpable purpura represents vasculitis
- 4.
Always rule out infection first in a patient with purpura
Purpura is purple and nonblanchable.
Purpura is divided into two major categories: nonpalpable (macular) and palpable (papular). Nonpalpable purpura results from bleeding into the skin without inflammation of the vessels and is caused by either a bleeding disorder or blood vessel fragility. Nonpalpable purpura is divided further according to the size of the lesion. Purpuric macules smaller than 3 mm are called petechiae; those larger than 3 mm are called ecchymoses. Thrombocytopenia is manifested by petechiae. Ecchymoses are owing to blood vessel fragility. Necrotic ecchymoses are found in disseminated intravascular coagulation (DIC), in which thrombi in dermal vessels lead to infarction and hemorrhage.
Nonpalpable purpura:
- 1.
Petechiae are found in thrombocytopenia
- 2.
Ecchymoses result from fragile blood vessels
- 3.
Necrotic ecchymoses occur in DIC
Palpable purpura results from inflammatory damage of blood vessels (vasculitis). The inflammation accounts for the elevation of the lesions and allows leakage of blood through the vessel wall. Features of these disorders are outlined in Table 17.1 . Infection needs to be ruled out in patients with purpura, especially in those with accompanying fever. Most causes of purpura, except for actinic purpura, are uncommon. Other uncommon causes of purpura are highlighted in the differential diagnosis sections.
Palpable purpura represents vasculitis in the skin.
| Frequency (%) a | Etiology | History | Physical Examination | Differential Diagnosis | Laboratory Test | |
|---|---|---|---|---|---|---|
| Thrombocytopenic purpura | Uncommon | Drugs Malignancy “Autoimmune” | Drugs Fever | Petechiae, often on legs Mucosal bleeding | Identify cause Pigmented purpura disease Scurvy | Complete blood count with platelet count |
| Actinic purpura | Uncommon | Blood vessel fragility from sun and aging | Sun exposure Steroid use | Ecchymoses confined to hands and arms | Steroid purpura Amyloidosis | Skin biopsy if amyloid is suspected |
| Disseminated intravascular coagulation (DIC) | Rare | Sepsis Malignancy Obstetric complications Idiopathic Warfarin | Fever (sepsis) Antecedent viral or streptococcal infection | Necrotic ecchymoses and/or: Petechiae Acral cyanosis Palpable purpura Mucosal bleeding Bleeding from venipuncture site | Vasculitis | Coagulation studies Protein C levels |
| Vasculitis | 0.3 b | Sepsis Collagen vascular disease Cryoglobulinemia Drugs Malignancy | – | Purpuric papules, nodules, or bullae Legs most commonly affected | DIC | Skin biopsy Screening tests for systemic involvement |
a Percentage of new dermatology outpatients with this diagnosis seen in the Hershey Medical Center Dermatology Clinic, Hershey, PA.
b Of inpatient dermatology consultations, 2% are for vasculitis.
Actinic Purpura
- 1.
Incidental finding in the elderly
- 2.
Appears as purpuric macules on forearms secondary to minor trauma
- 3.
Caused by dermal atrophy from sun exposure and age
- 4.
There is no specific treatment
Definition
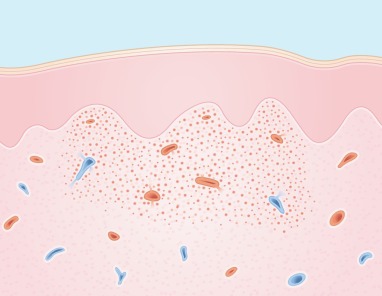
Purpura resulting from blood vessel fragility appears clinically as ecchymoses, that is, purpuric macules of more than 3 mm in diameter ( Fig. 17.1 ). Dermal tissue atrophy resulting from sun exposure and aging is the most common cause. Blood thinners such as low-dose aspirin also lead to additive susceptibility.

Incidence
Actinic purpura is extremely common in elderly people, in whom it is usually noted only as an incidental finding.
History
The trauma that induces the purpura is often so minor that it is not remembered by the patient. The patient has no symptoms, and health is unaffected.
Physical Findings
Ecchymoses are usually round or oval macules. In actinic purpura, they are characteristically confined to the dorsa of the hands and forearms. The skin itself in these areas may also be more fragile and may tear easily ( Fig. 17.2 ).
Actinic purpura occurs only on the hands and forearms.

Another clinical finding is the development of stellate pseudoscars ( Fig. 17.3 ). These thin line scars result from the healing of the skin tears.

Differential Diagnosis
The diagnosis of actinic purpura is relatively straightforward, thereby making a differential not necessary. Other causes of blood vessel fragility, in declining order of frequency, are corticosteroid use, amyloidosis, and Ehlers–Danlos syndrome. Steroid purpura with skin atrophy can result from topically or systemically administered corticosteroids. Patients with excessive systemic steroids also have a moon facies, a “buffalo hump” on the upper back, purple striae, and, in younger patients, steroid acne.
Causes of blood vessel fragility:
- 1.
Actinic damage
- 2.
Steroid use
- 3.
Amyloidosis
- 4.
Ehlers–Danlos syndrome
In patients with amyloidosis, the amyloid may infiltrate the skin and result in papules and nodules, which are most often present on the face, particularly the eyelids. These characteristically bleed easily. Purpura also occurs in the absence of papules and can be precipitated by minor trauma or the Valsalva maneuver, referred to as “pinch” purpura ( Fig. 17.4 ). The tongue may also be enlarged.

Ehlers–Danlos syndrome is the least common cause of blood vessel fragility. Several variants of this syndrome are known, in which joint hyperextensibility, skin hyperelasticity, increased fragility of the skin, and increased tendency to bruise occur in varying combinations. Ecchymoses resulting from blood vessel fragility are distinguished from vasculitis by being macular and from the ecchymoses in DIC by their usually smooth rather than ragged contour and by the absence of necrosis.
- ●
Steroid purpura
- ●
Amyloidosis (rare)
- ●
Ehlers-Danlos (rare )
Ecchymoses resulting from fragile blood vessels have a smooth border and are not necrotic.
Laboratory and Biopsy
Because the diagnosis of actinic purpura is obvious clinically, a biopsy is not required. If a biopsy is done, hemorrhage without inflammation will be noted in the dermis, along with actinically damaged collagen, which appears disorganized, smudged, fragmented, and more basophilic than normal collagen on routine hematoxylin and eosin staining ( Fig. 17.5 ).
Therapy
No therapy exists for actinic purpura. Protection against sun exposure with sunscreens is advisable to prevent further damage. Avoidance of prolonged topical steroid use is recommended. It is important to offer reassurance that the condition is benign.
Course and Complications
Ecchymoses slowly fade, leaving brown macules from residual hemosiderin. New ecchymoses, however, continue to develop. Scars frequently occur after tearing of the skin, and are referred to as stellate pseudoscars.
Pathogenesis
The diseases of blood vessel fragility have in common the problem of defective collagen, which weakens the vessels and makes them more susceptible to bleeding from minor trauma. In actinic purpura, blood vessel fragility results from both aging and the damaging effect of sunlight on connective tissue support to blood vessels in sun-exposed skin. Steroid purpura results from inhibition of collagen metabolism by high-dose corticosteroids. In amyloidosis, amyloid material infiltrates and weakens the vessel walls. In Ehlers–Danlos syndrome, fragility of blood vessels results from an intrinsic abnormality in collagen biosynthesis.
Disseminated Intravascular Coagulation
- 1.
Life-threatening
- 2.
Seen in bacterial sepsis (meningococcemia)
- 3.
Stellate purpura with central necrosis is characteristic
- 4.
Treat underlying condition
Definition
Disseminated intravascular coagulation is a condition in which uncontrolled clotting results in diffuse thrombus formation. The skin is frequently affected, with thrombosed vessels causing skin necrosis. Hemorrhage from these vessels appears as ecchymoses ( Fig. 17.6 ). Petechiae also occur as a result of the thrombocytopenia from platelet consumption. Purpura fulminans can be confused with the term DIC. Purpura fulminans is the cutaneous marker of DIC, characterized by the sudden appearance of ecchymosis, symmetrically distributed mainly on the extremities. Skin necrosis often develops in purpura fulminans in the setting of DIC and is most commonly associated with an infection ( Fig. 17.7 ).


Incidence
An uncommon, life-threatening disease, DIC usually occurs in the setting of bacterial sepsis (particularly meningococcemia). DIC may also be associated with malignancy, particularly prostatic carcinoma and acute promyelocytic leukemia. It can also be precipitated by massive trauma. Occasionally, it may result from amniotic fluid embolism, or it may occur as an idiopathic or “postinfection” phenomenon. Localized intravascular coagulation occurs in patients with protein C deficiency who are given warfarin (Coumadin necrosis).
Causes of DIC:
- 1.
Bacterial sepsis
- 2.
Malignancy
- 3.
Amniotic fluid embolism
- 4.
Trauma
- 5.
Idiopathic
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








