Photo 21.1 3D computerized tomography of a patient with pelvic support osteotomy
At the end of the treatment, the limb length discrepancy is eliminated and a normal alignment of the knee joint is obtained.
The aesthetic aspect of PSO is very satisfactory because the soft tissue of the thigh hides the double angulation of the femur and the proximal valgus correction of the subtrochanteric osteotomy moves laterally the gluteal region offering a better clinical aspect with respect to the one before surgery (hypotonic hip). In the end, a better abduction of the hip improves personal hygiene and sexual activity.
21.4 Preoperative Planning
To determine the right position of proximal osteotomy is necessary to perform both static and dynamic hip x-rays:
1.
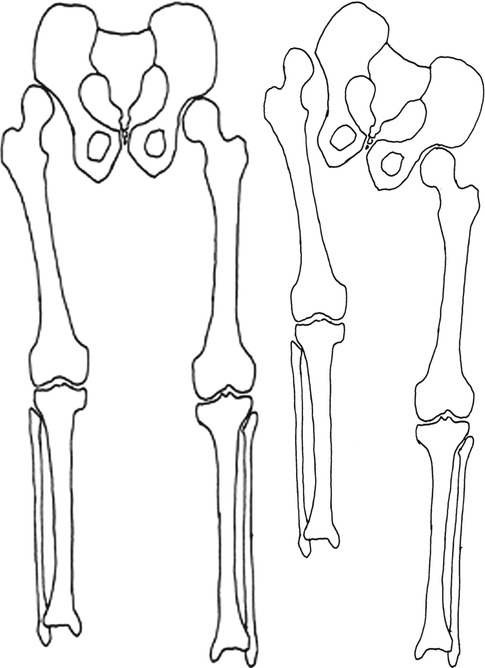
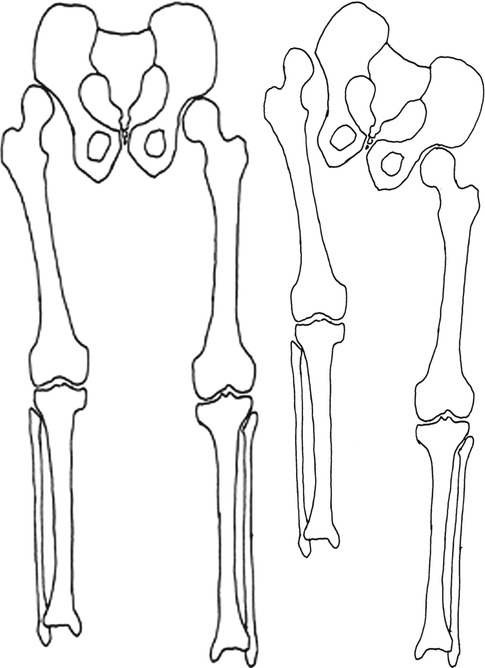
Orthostatic x-rays in bipodalic weight bearing – to evaluate the static axis of the lower limbs (Fig. 21.1).
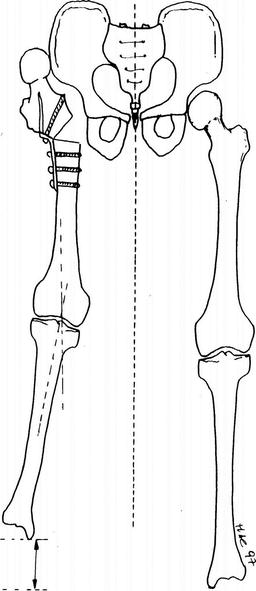
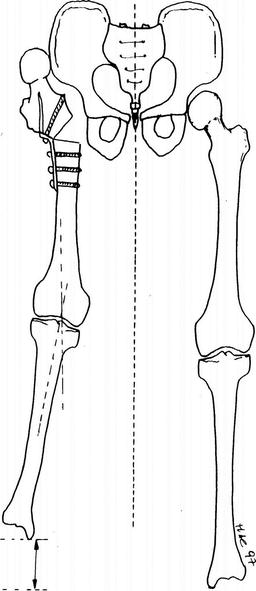
Fig. 21.1
Osteotomy planning in standing position
2.
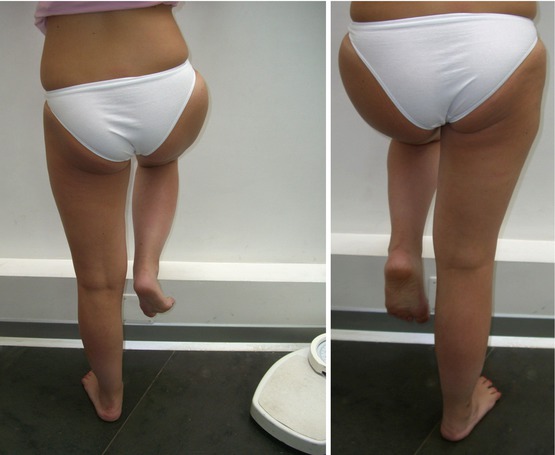
Dynamic x-rays with monopodalic bearing on the pathological limb – to evaluate Trendelenburg sign and the shortening of the proximal femur during weight bearing (Fig. 21.2); a second dynamic x-ray is taken in maximum adduction with patient in the supine position.
Figs. 21.2 and 21.3
Dynamic planning with monopodalic bearing on the pathological limb
With these x-rays, we can plan the level of the osteotomy (distal part of the obturator foramen) and the correction’s angle.
The planning is completed with the evaluation of the varus and lengthening correction of the distal femur. A transparent copy of the x-ray with monopodalic bearing is used, and a subtrochanteric cut is made (>20–30° with respect to the pelvis projection in the monopodalic bearing x-ray); then two lines are drawn: one passing by the medial part of the osteotomy and the centre of the knee and a second one passing by the tibia’s axis; the angle obtained corresponds to the one necessary to obtain the alignment of the mechanical axis of the lower limb (Figs. 21.3 and 21.4). This preoperative planning could be helpful, but the final decisions of the various corrections are performed during treatment.
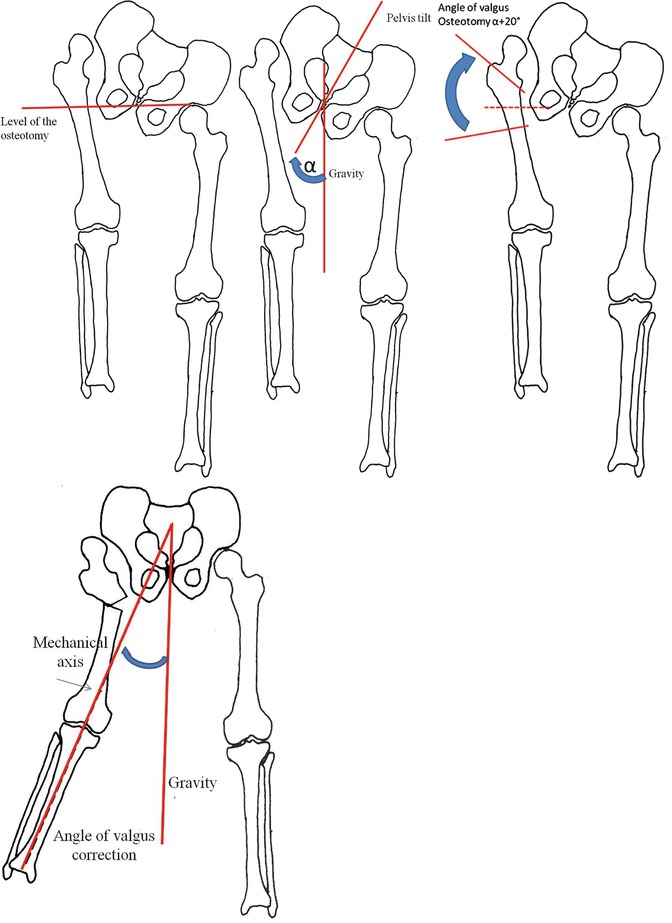
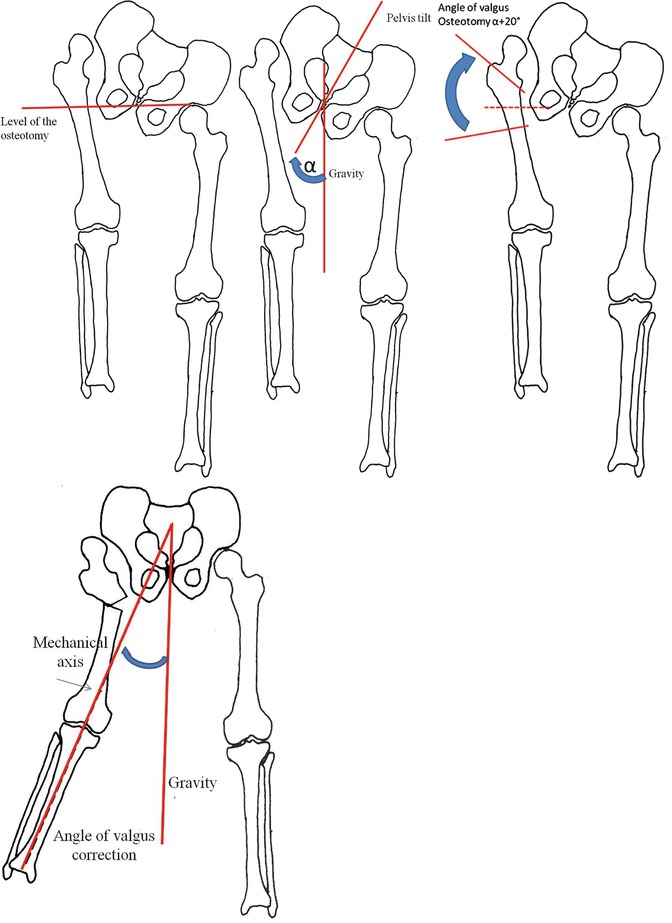
Figs. 21.4, 21.5, 21.6, and 21.7
With these x-rays, we can plan the level of the osteotomy
21.5 Operative Technique
In the original operative technique described by Ilizarov, the whole fixation was performed with K-wires connected to half rings in the proximal part of the femur and full rings in the distal part.
In 1986 this fixation was modified using new arches (type Catagni-Cattaneo) (Catagni et al. 1996) and pin fixation (Fig. 21.5).
Thanks to these modifications, specific beds were no more used and patients could sit normally (impossible with the original fixation).
Transfixion of femoral artery and sciatic nerve is also avoided, as wire track infections are also reduced.
The use of pin instead of K-wires reduces pain in patients and permits a complete ROM of the hip, avoiding flexion contractions that where often seen using the original apparatus. These contractions in flexion prevent correct evaluation of the mechanic axis because patients could not have a normal full weight-bearing stand.
Also only a pin-based fixation is used on the distal part, with the exception of a single K-wire (Fig. 21.6).
21.6 Operation
The pre-assembled frame consists of two 90° arches proximally set at the estimated angle of valgus osteotomy, a floating ring and two full rings distal to hinges to allow lengthening and varus rotation of the distal femur. Generally the arches and rings will be parallel at the end of the procedure, although this is not necessary if the individual anatomy dictates otherwise.
The frame is pictured in Figs. 21.7 and 21.8. The patient is placed on a fracture table to allow circumferential access to the thigh and a surgical assistant access between the legs. The leg is supported just distal to the knee with the foot free, to allow full knee motion during surgery.
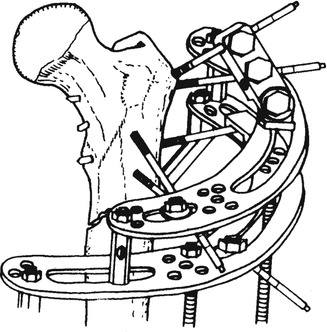
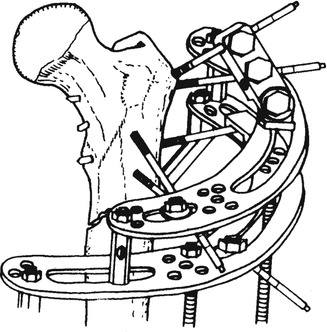
Fig. 21.8
Overview of the proximal part of the frame
Three K-wires are placed in the proximal femur corresponding to the intended level of the proximal arch, proximal osteotomy and distal arch, and an intraoperative x-ray is obtained. Such wire is used just for references and an x-ray is taken.
The proximal intertrochanteric 5 mm half-pin is placed at the predetermined angle to the skin. The leg is maximally adducted during insertion of this pin to avoid soft-tissue contact between the two arches. The frame is suspended with a transverse 1.8 mm wire in the distal ring, parallel to the knee joint. The remaining wires and half-pins are inserted. The proximal femoral osteotomy is performed through a lateral incision. Standard osteotomy technique with minimal soft-tissue disruption is used. A 4/5 cm incision is used to allow palpation of the bone ends; impaling the distal and lateral cortices of the proximal fragment into the intramedullary canal of the distal fragment can increase stability. After connecting and stabilizing the proximal arches, the distal osteotomy is performed with Gigli saw. A final intraoperative x-ray is obtained to control the fixation and alignment (Figs. 21.9, 21.10, 21.11, 21.12, and 21.13).
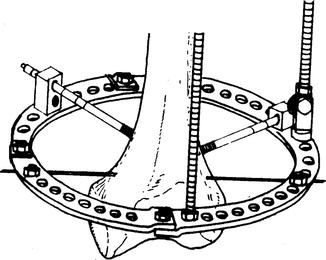
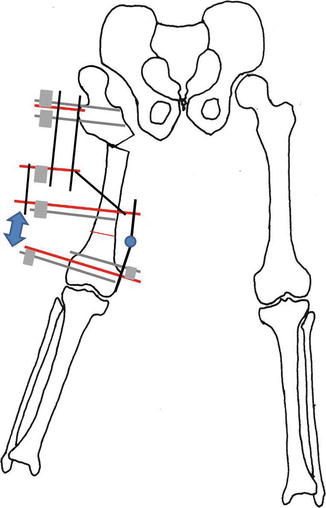

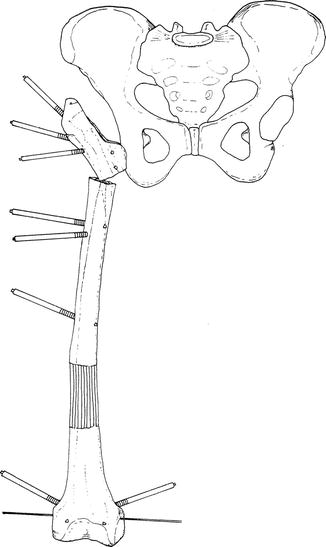
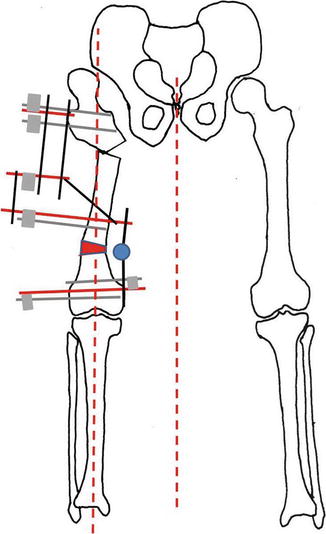
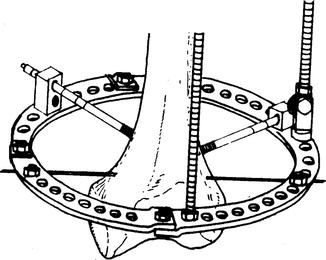
Fig. 21.9
Overview of the distal part of the frame
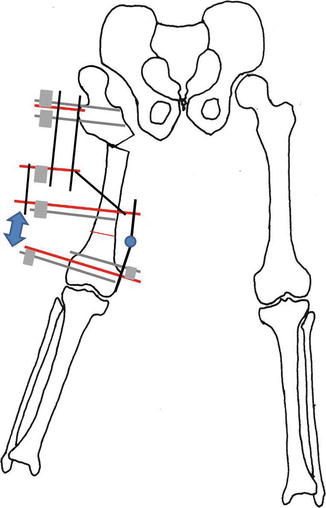
Fig. 21.10
Frame placed and correction performed

Fig. 21.11
Half-pin placement in x-ray
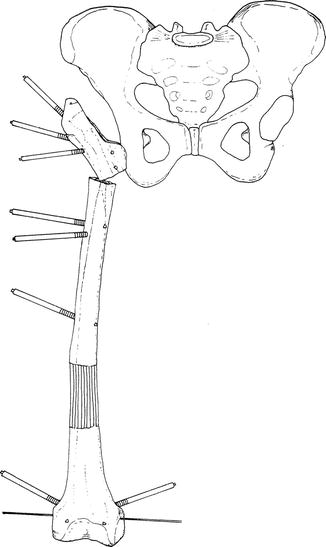
Fig. 21.12
Half-pin placement and lengthening
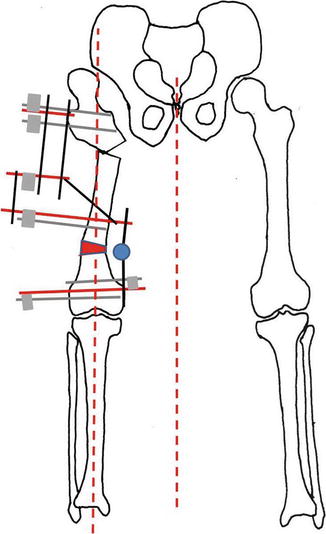
Fig. 21.13
Distal varus and proximal valgus alignment shown
21.7 Post-op Care
Weight bearing is allowed as tolerated, usually beginning partial weight bearing in 2/3 days. The dynamic nature of Ilizarov apparatus allows “fine-tuning” of proximal and distal angles. When the angle of the proximal osteotomy is satisfactory, compression is applied between the arches. Lengthening begun distally, 1/4 mm four times a day starting at the 5/7 postoperative day. Varus angulation of the distal femur is created near the end of lengthening, using the hinges between the two distal rings (Catagni and Cattaneo 1986; Cattaneo et al. 1990; Catagni 1992). Mechanical axis and leg length are “fine-tuned” after the patient has undergone weight bearing. Physical therapy is used to strengthen the hip abductors and adductors and to maintain hip and knee motion. After appropriate length and alignment are obtained, the frame is left in a static mode until satisfactory healing of the osteotomy and regenerate allows frame removal. The distal transverse wire can be removed at the end of lengthening to facilitate knee motion.
Sometimes, it is necessary to lengthen the apparatus by fixation of the tibia and use appropriate hinges to allow movements and prevent subluxation or stiffness of the knee that can occur in cases of great femoral dysmetria that leads to a great distal femoral lengthening and axial correction.
In the worst cases we apply the apparatus not only to prevent problems on the knee but also to perform tibial lengthening in the metaphyseal region to reduce:
1.
The correction forces on the femur
2.
Stiffness of the knee
3.
The time of treatment
It is proved that the healing of a trifocal lengthening is shorter than a bifocal one, and a 2\3 cm discrepancy of lengthening between knees is well tolerated both aesthetically and mechanically.
21.8 Complications
The most frequent complication is the pin’s tract infection, mostly around the distal pins and during the distraction phase. Fracture regenerate that occurred after frame removal, premature consolidation, delayed consolidation and residual limb length discrepancy are also complications.
Most of the patients had knee stiffness after frame removal due to prolonged external fixation time. We found that knee range of motion showed progressive improvement during the 6-month period following frame removal.
Tendency to knee valgus and external rotatory subluxation at the joint, during lengthening, can be observed. This complication was even expected in the poliomyelitis patients or in the patient who showed knee instability during preoperative evaluation.
21.9 Presentations
21.9.1 Case Report of Septic Arthritis

Fig. 21.14
Dynamic x-rays
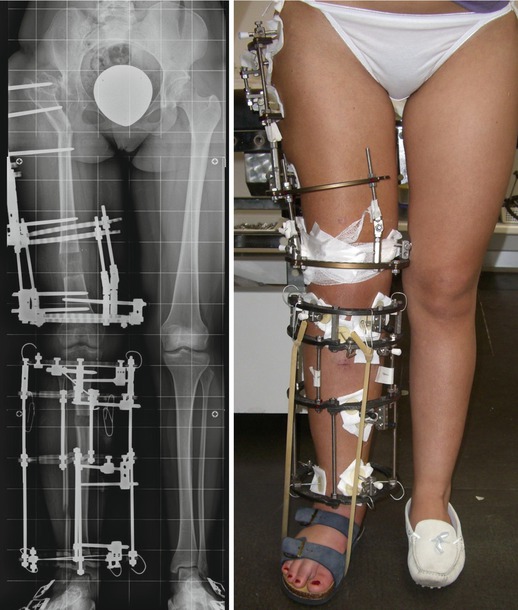
Figs. 21.15 and 21.16
X-rays during the treatment and photos of the frame
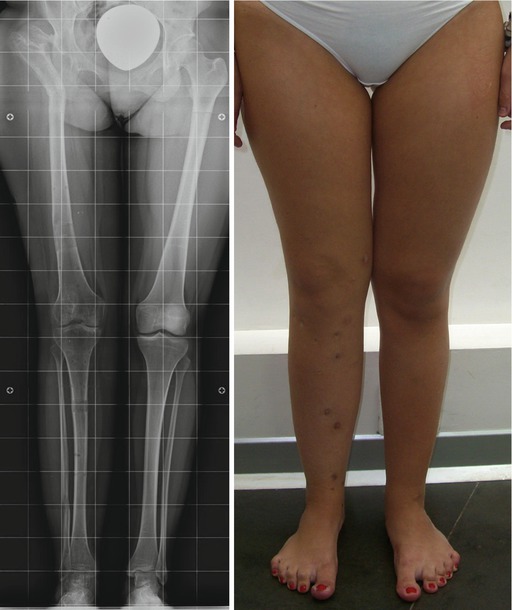
Figs. 21.17 and 21.18
X-rays after the treatment and photos of the patient

Figs. 21.19 and 21.20
Photos of the patient’s ROM of the hip and knee