Key Words
breast conserving therapy (BCT), oncoplastic surgery, partial breast reconstruction, local flaps, partial mastectomy, volume replacement techniques, volume displacement techniques
Introduction
Breast conserving therapy (BCT) with partial mastectomy followed by radiation therapy is the gold standard of early stage invasive breast cancer treatment, with an equivalent 5-year survival rate to that of mastectomy alone with stage I or II breast cancer.
Partial mastectomy includes both lumpectomy and quadrantectomy. Oncoplastic surgery, the combination of partial mastectomy with partial breast reconstruction reduces potential breast deformities and results in aesthetic breast reshaping. The first aim of oncoplastic surgery is avoiding mastectomy with complete cancer ablation and clear surgical margins without the distortion of the natural shape of the breast. The main steps of oncoplastic approach are free margin cancer ablation, optimal scar orientation, breast tissue rearrangement and, when indicated, contralateral breast reshaping in order to achieve symmetry.
Indications and Contraindications
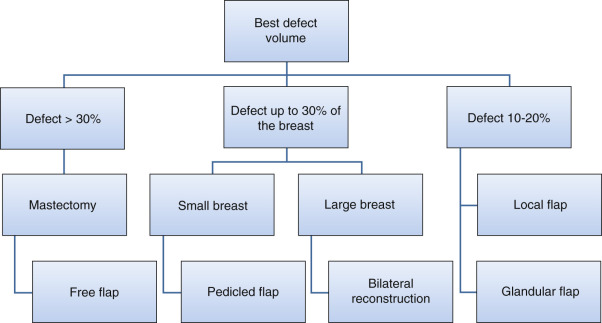
Patients often require surgery after partial mastectomy to correct volume discrepancy, contour deformity and nipple malposition. The resection of more than 15%–20% of the breast parenchyma in a small-volume (A or B cup) breast and more than 30% in larger breast will determinate volumetric deformities and bilateral asymmetries ( Fig. 15.1 ). Patients with small or non-ptotic breasts could require volume replacement. In addition, radiotherapy distorts the shape of the breast, initially causing breast edema and skin erythema and eventually causing parenchymal fibrosis, retraction, skin atrophy, hyper-/hypopigmentation, and telangiectasia. The long-term results of radiation are difficult to predict but stabilize 1–3 years after radiation. Furthermore, oncoplastic surgery extends the indications for breast conservation surgery to allow the resection of much larger tumors relative to breast size. In these patients, partial breast reconstruction with flaps could be considered as an important part of whole breast cancer treatment.
The main indication for pedicled flaps is immediate or delayed partial breast reconstruction when volume replacement is necessary. However, other conditions will require locoregional flaps in partial breast reconstruction. These flaps can be utilized as a salvage procedure after partial/total previous free flap loss for breast reconstruction. They can be combined with implants in breast reconstruction as well.
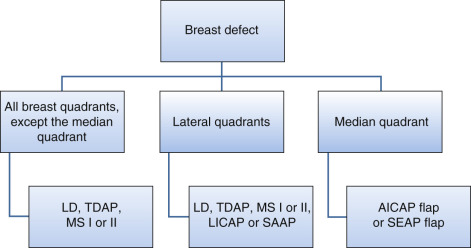
Previous axillary or thoracic surgery with damage to the thoracodorsal vessels is a contraindication for latissimus dorsi flap or thoracodorsal artery perforator (TDAP) flap; these patients may be candidates for a lateral intercostal artery perforator (LICAP) flap. Previous scars and irradiation to the area may also result in the limitation of local pedicled perforator flaps ( Fig. 15.2 ). However, when breast deformity after partial mastectomy and radiotherapy is severe, the optimal choice is to perform a complete mastectomy and autologous reconstruction with a free flap transfer.
Preoperative Evaluation and Special Considerations
Preoperative evaluation of the patient must be standardized and detailed. Any previous breast surgery should be taken into account when planning BCT. Different body types, skin laxity and fat distribution are important factors in the decision-making process. Breast physical examination must include the evaluation of breast skin elasticity and thickness, scars and any defining marks such as tattoos, stretch marks and contour irregularities. Breast shape, grade of ptosis, and size are determinants of success in surgical treatment. The base and width of the breast, the width of the nipple–areola complex (NAC), the height of the nipple and the distance from the sternal notch, midline and inframammary fold must be recorded in detail. Any natural breast asymmetry should be pointed out to the patient before surgery. Furthermore, palpation for masses or abnormalities in the breast parenchyma, nipple examination and detailed documentation of breast sensation are mandatory.
In planning the approach to treat the partial mastectomy defect, the primary decision that must be made is whether reconstructive surgery will be needed after the tumor excision. Poor cosmetic outcomes after partial mastectomies can occur from both the amount of breast tissue removed and/or the site of the cancer. Partial breast reconstruction with flaps depends on the size of the tumor, its anatomical location, and the amount of tissue resection required to achieve free margins in relation to the volume of the breast.
There are two basic types of surgical techniques in partial breast reconstruction: volume displacement and volume replacement techniques. Volume replacement techniques are the focus of this chapter. They are used in small to moderate-sized breasts or when the tumor/breast ratio is large and the residual breast tissue is insufficient for the reshaping and the replacement of the defect. Volume replacement is performed with non-breast local or distant flaps offering both tissue for the filling of the glandular defect and the skin deficiency of the reconstructed breast.
When volume replacement is necessary, the decision of which technique will be used is determined mostly by the surgeon’s experience and the size of the defect in relation to the size of the remaining breast. The non-breast locoregional flaps offer extra tissue required in large tumor excisions/quadrantectomies for the replacement of the breast volume, however they can be more demanding procedures and associated with donor-site and flap morbidity. Small lateral defects can be easily repaired with skin rotation flaps or lateral thoracic axial flaps. However, most of these fasciocutaneous flaps may be unavailable in patients who have had axillary lymph node dissection. The latissimus dorsi muscle (LD) or musculocutaneous flaps have been very popular as a method of choice in partial breast reconstruction. On the other hand, local pedicled perforator flaps have allowed surgeons to replace large defects with the minimum donor-site morbidity. Fasciocutaneous perforator flaps offer sufficient soft tissue coverage while sparing the muscle and tend to have a lower seroma rate.
Surgical Techniques
Relevant Surgical Anatomy
Breast and plastic surgeons must have a thorough understanding of breast anatomy, physiology and the standards of aesthetically pleasing breast shape. Oncoplastic surgeons should consider the aesthetic breast subunits when planning both cosmetic quadrantectomies and reconstructions ( Box 15.1 ).
- •
The breast skin to the areola
- •
The areola to the nipple
- •
The breast skin to the chest wall at the inframammary fold
- •
The anterior axillary line
- •
The breast to the sternal skin
Different aesthetic breast subunits have been proposed according to the tissue, color and texture differences.
The Latissimus Dorsi (LD) Flap
The LD flap has the advantage of having a constant anatomy. The blood supply of the latissimus dorsi comes from the thoracodorsal artery, a terminal branch of the subscapular artery. The subscapular artery runs about 5 cm before splitting into the scapular circumflex and the thoracodorsal arteries. The thoracodorsal artery is about 2–4 mm in diameter and it courses along the posterior axillary fold for about 8–14 cm before piercing the latissimus dorsi on its costal surface. The thoracodorsal artery gives off one or two branches to the serratus anterior muscle and one branch to the overlying skin. The basic pattern of the thoracodorsal bundle (artery, nerve and 1–2 venae comitantes) branches into a lateral (vertical) and a medial (horizontal) branch. The lateral branch follows a course parallel to the muscle fibers, 1–4 cm medial to the free lateral border of the muscle and gives off perforating vessels that supply the skin. The smaller medial branch diverges at an angle of 45 degrees and travels medially. Also, perforating vessels from the intercostal and lumbar arteries supply the muscle and overlying skin.
The TDAP Flap
The thoracodorsal artery perforator (TDAP) flap is based on the perforators from the descending (vertical) or horizontal branches of the thoracodorsal vessels ( ![]() ). Anatomic studies on cadavers showed the presence of 2–3 musculocutaneous perforators from the vertical branch. The proximal perforator enters in the subcutaneous plane obliquely 8–10 cm distal to the posterior axillary fold and 2–3 cm posterior to the anterior border of the muscle. The second perforator is located 2–4 cm distally to the first one. Occasionally, a direct cutaneous perforator arising from the thoracodorsal vessel passes around the anterior border of the muscle, making flap harvesting easier.
). Anatomic studies on cadavers showed the presence of 2–3 musculocutaneous perforators from the vertical branch. The proximal perforator enters in the subcutaneous plane obliquely 8–10 cm distal to the posterior axillary fold and 2–3 cm posterior to the anterior border of the muscle. The second perforator is located 2–4 cm distally to the first one. Occasionally, a direct cutaneous perforator arising from the thoracodorsal vessel passes around the anterior border of the muscle, making flap harvesting easier.
There may not be always a single reliable perforator for the TDAP flap, due to anatomical variations. In this case the surgeon must be aware and be prepared to modify the flap dissection intraoperatively into a muscle-sparing TDAP flap.
The TDAP flaps are classified as follows :
- •
Standard TDAP flap , when no muscle component is included in the flap.
- •
TDAP-MS-I , where a small cuff of muscle (4 × 2 cm) is included near the perforator vessels. The muscle segment protects the perforators from excessive tension and provides more freedom in flap positioning.
- •
TDAP-MS-II , where multiple small perforators are encountered and a larger segment, up to 5 cm wide, along the anterior border of the latissimus dorsi muscle together with the descending branch of the thoracodorsal vessels is then included within the flap in order to insure a maximal blood supply to the skin paddle ( Fig. 15.3 ).

Fig. 15.3
TDAP anatomy.
(Adapted from Hamdi M, Salgarello M, Barone-Adesi L, Van Landuyt K. Use of the thoracodorsal artery perforator (TDAP) flap with implant in breast reconstruction. Ann Plast Surg . 2008;61(2):143–146.)
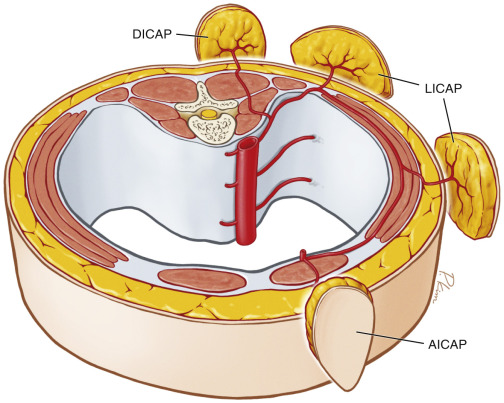
The ICAP Flap
The intercostal artery perforator (ICAP) flap is based on perforators arising from the intercostal vessels. The intercostal vessels provide an arcade between the aorta and the internal mammary vessels and are classified in four segments: vertebral, intercostal, intermuscular and rectus segments.
The ICAP flaps are classified as follows:
- •
Dorsal intercostal artery perforator (DICAP) flap : the flap is based on perforators from the vertebral segment of the intercostal vessels.
- •
The lateral intercostal artery perforator (LICAP) flap , based on perforators arising from the intercostal segment.
- •
Anterior intercostal artery perforator (AICAP) flap : the nutrient perforators of this flap arise from the muscular or rectus segment.
The AICAP flap is outlined over the upper abdomen, so that the final scar will be hidden under the bra strap. The donor site can be closed primarily if it is up to 6 cm wide (preoperative pinch test) or in a reversed abdominoplasty fashion ( Fig. 15.4 ).
Preoperative Markings
Perforator mapping simplifies flap marking and can be performed using a portable ultrasound system.
To localize the thoracodorsal perforators, a unidirectional handheld Doppler (8 Hz) ultrasonography examination is performed in the planned skin flap area. However, although this device is handy, it has the disadvantage of generating both false negative and false positive perforators and provides less detailed anatomic vessel information. This is due to the misleading background signal from the thoracodorsal vessels, which can be confusing and difficult to distinguish from the perforator signal. To avoid this, during the test, the patient is positioned in the lateral surgical position with 90 degrees of shoulder abduction and 90 degrees of elbow flexion. Preoperative, CTA scan can be also used to accurately identify the perforators. The patient is preferably marked the day before surgery. In immediate reconstruction, the breast and the tumor size and location as well as the final defect size are estimated. The skin incisions of the partial mastectomy are planned both for oncologic and aesthetic purposes. The TDAP flap, planned for the partial breast reconstruction, is designed to include the traced perforators (one or more) at the proximal part if feasible, in the directions of relaxed skin lines, under the bra line, or even horizontally according to the patient’s preference. The pinch test estimates the skin laxity and fat excess in the lateral thorax and backing area. The size of the flap is determined by the need for defect coverage and averages 20 × 8 cm. The skin marking is performed at first with the patient in an upright position and the anterior border of the LD muscle is palpated and also marked. Then the patient is placed in a lateral decubitus position, with the reconstruction side facing upwards, for the perforator mapping and the flap design. The skin island is always extended over the anterior border of the latissimus dorsi to include the premuscular perforators if present. The proximal border of the flap approximates the inframammary fold. If the defect is more medial, the flap is designed more distally, further onto the back. The LICAP flap design follows the same rules, however the flap is placed more anteriorly, towards the breast. When AICAP flaps are chosen for partial breast reconstruction, these flaps are usually designed under the IMF along the rib.
Surgical Exposure and Details of Procedure
The patient is prepped and positioned in supine position for the partial breast mastectomy. When the lumpectomy/quadrantectomy is completed, clips are placed in the wound bed in order to mark the area for radiation therapy. If the reconstructive plan provides for a TDAP or LICAP flap, the patient is positioned and prepped again in lateral position as for LD flap dissection. Otherwise, for AICAP flaps the patient remains in the supine position. The flap harvesting starts with skin incisions. A posterior approach is usually used in the TDAP flap. The surgeon continues dissection down to the LD in the suprafascial plane, while beveling the flap in order to gain as much extra tissue as possible. Harvesting proceeds from the back towards the axillary region. The dissection continues meticulously, under loupe magnification, until the perforator vessel is visualized.
If the perforator has a visible pulsation and is adequate in caliber (>0.5 mm) the dissection continues along the perforator course up to the thoracodorsal pedicle. If a longer pedicle length is required, the TD vessels can be dissected up to their subscapular vessel origin and included in the flap. If the perforator has an intramuscular course, the dissection is achieved in the direction of the muscle fibers and any nerves that come across should be carefully preserved. All the perforator side branches within the muscles fibers are either ligated or coagulated. If two perforators are found along the same row, they can both be included within the flap, without sacrificing any muscle fibers. In case of inadequate perforator size, the flap is converted to a muscle-sparing LD, preserving a small cuff of muscle attached to the posterior wall of the perforators, sacrificing only few fibers and, most important, preserving the muscle innervation. This adjustment is also useful when the flap is planned for the medial breast reconstruction, because it protects the perforators from tension. The flap harvesting carries on, with the skin incisions continued proximal to the axilla and lateral to the LD and the dissection proceeds anteriorly, until the flap is freed from the donor site and left connected only to the vascular pedicle.
The flap is tunneled in a subcutaneous tunnel in the axilla–lateral thoracic area to the recipient breast area, avoiding any injury to the pedicle. The donor site is closed in three anatomical layers, a drain is placed and the patient is returned again to the supine position. Before the final insetting, the flap can be partially or totally de-epithelialized and folded if needed to give extra projection to the reconstructed breast mound. In LICAP flap dissection, an anterior approach is performed from the breast towards the anterior-free border of LD muscle. Perforator dissection is done within the serratus muscle until reaching its origin from the costal groove. Further dissection is usually not needed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree