Periprosthetic fractures about a total hip arthroplasty are fractures which occur in the femur or acetabulum adjacent to either the femoral or acetabular component, respectively. These fractures can occur intraoperatively or postoperatively. The focus of this chapter will be postoperative fractures of the femur which occur adjacent to the femoral component of a total hip arthroplasty.
ANATOMY
 Fractures of the femur adjacent to the femoral component of a total hip arthroplasty are most commonly described using the Vancouver classification system which categorizes the fracture on the basis of anatomic location, stability of the femoral component, and surrounding bone stock (Table 1; FIG 1).5 This classification system is simple, reliable, and serves to guide treatment.
Fractures of the femur adjacent to the femoral component of a total hip arthroplasty are most commonly described using the Vancouver classification system which categorizes the fracture on the basis of anatomic location, stability of the femoral component, and surrounding bone stock (Table 1; FIG 1).5 This classification system is simple, reliable, and serves to guide treatment.
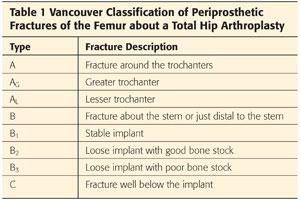
 Type A fractures occur in the trochanteric region and involve either the greater trochanter (AG) or the lesser trochanter (AL).
Type A fractures occur in the trochanteric region and involve either the greater trochanter (AG) or the lesser trochanter (AL).
 Type B fractures occur around or just distal to the stem of the femoral component and are subclassified based on the stability of the implant and the surrounding bone stock. Type B1 fractures occur around a stable implant. Type B2 fractures occur around a loose implant with adequate bone stock. Type B3 fractures occur around a loose implant with poor bone stock.
Type B fractures occur around or just distal to the stem of the femoral component and are subclassified based on the stability of the implant and the surrounding bone stock. Type B1 fractures occur around a stable implant. Type B2 fractures occur around a loose implant with adequate bone stock. Type B3 fractures occur around a loose implant with poor bone stock.
 Type C fractures occur well distal to a stable femoral component.
Type C fractures occur well distal to a stable femoral component.
PATHOGENESIS
 Postoperative periprosthetic fractures can occur in a variety of settings; however, major trauma accounts for a very small proportion.
Postoperative periprosthetic fractures can occur in a variety of settings; however, major trauma accounts for a very small proportion.
 The majority of these fractures occur with a low-energy fall and up to 25% occur without any significant trauma.
The majority of these fractures occur with a low-energy fall and up to 25% occur without any significant trauma.
 A large proportion of these patients have pathologic and osteopenic bone due to a combination of factors including localized osteopenia of the proximal femur due to stress shielding and osteolysis as well as a high prevalence of osteoporosis in this patient population.
A large proportion of these patients have pathologic and osteopenic bone due to a combination of factors including localized osteopenia of the proximal femur due to stress shielding and osteolysis as well as a high prevalence of osteoporosis in this patient population.
NATURAL HISTORY
 The vast majority of these fractures require surgical management for effective fracture healing and return of function.
The vast majority of these fractures require surgical management for effective fracture healing and return of function.
 Retrospective literature has demonstrated a 1-year mortality of 11% and morbidity/mortality very similar to hip fracture patients.1 This is an important consideration as these patients should be managed in a similar fashion to hip fracture patients by incorporating a multidisciplinary team approach (geriatrics assessment, delirium prevention etc.), carrying out early surgical intervention (<48 hours from injury), and using a surgical strategy that allows early weight bearing and mobilization.
Retrospective literature has demonstrated a 1-year mortality of 11% and morbidity/mortality very similar to hip fracture patients.1 This is an important consideration as these patients should be managed in a similar fashion to hip fracture patients by incorporating a multidisciplinary team approach (geriatrics assessment, delirium prevention etc.), carrying out early surgical intervention (<48 hours from injury), and using a surgical strategy that allows early weight bearing and mobilization.
PATIENT HISTORY AND PHYSICAL FINDINGS
 It is important to obtain information regarding the mechanism of injury and level of energy imparted as well as the cause of the fall.
It is important to obtain information regarding the mechanism of injury and level of energy imparted as well as the cause of the fall.
 Information regarding prodromal symptoms such as thigh pain with weight-bearing or start-up pain should be obtained and may indicate a preexisting loose femoral stem prior to fracture.
Information regarding prodromal symptoms such as thigh pain with weight-bearing or start-up pain should be obtained and may indicate a preexisting loose femoral stem prior to fracture.
 A history of past infections, wound healing complications, or constitutional symptoms may indicate a periprosthetic infection.
A history of past infections, wound healing complications, or constitutional symptoms may indicate a periprosthetic infection.
 A social history including the patient’s prior ambulatory status, use of walking aids, level of independence, and overall functionality is helpful for setting reasonable treatment goals.
A social history including the patient’s prior ambulatory status, use of walking aids, level of independence, and overall functionality is helpful for setting reasonable treatment goals.
 Physical examination may indicate gross deformity of the limb in a displaced fracture or the findings may be more subtle in minimally displaced fractures such as pain with range of motion or rotation of the hip, difficulty weight bearing, or weakness of the limb. Physical examination should also focus on ruling out open wounds, neurovascular injury, and associated injuries.
Physical examination may indicate gross deformity of the limb in a displaced fracture or the findings may be more subtle in minimally displaced fractures such as pain with range of motion or rotation of the hip, difficulty weight bearing, or weakness of the limb. Physical examination should also focus on ruling out open wounds, neurovascular injury, and associated injuries.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Investigation begins with anteroposterior (AP) and lateral radiographs of the affected femur and an AP pelvis. Radiographs should be carefully inspected for the location of fracture lines, fragment displacement, implant loosening, and quality of bone stock.
Investigation begins with anteroposterior (AP) and lateral radiographs of the affected femur and an AP pelvis. Radiographs should be carefully inspected for the location of fracture lines, fragment displacement, implant loosening, and quality of bone stock.
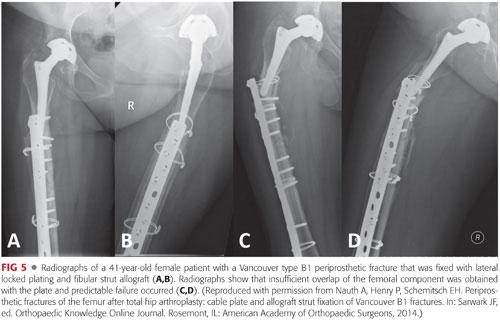
 It is critical to identify any evidence of implant loosening as the surgical management of a periprosthetic fracture with a loose femoral component (Vancouver type B2) requires revision to a long-stem component in addition to fracture fixation, whereas a fracture with a stable component (Vancouver type B1) can be readily treated with fracture fixation alone. Lindahl et al4 reported that the most common reason for treatment failure in the fixation of Vancouver type B1 fractures was loosening of the implant, presumably due to failure to recognize that the implant was loose at the time of fracture.
It is critical to identify any evidence of implant loosening as the surgical management of a periprosthetic fracture with a loose femoral component (Vancouver type B2) requires revision to a long-stem component in addition to fracture fixation, whereas a fracture with a stable component (Vancouver type B1) can be readily treated with fracture fixation alone. Lindahl et al4 reported that the most common reason for treatment failure in the fixation of Vancouver type B1 fractures was loosening of the implant, presumably due to failure to recognize that the implant was loose at the time of fracture.
 Definite signs of radiographic loosening include progressive periprosthetic or cement mantle lucency, change in position of the stem, and component or cement mantle fracture (FIG 2). Radiographic signs of probable loosening include greater than 2 mm of periprosthetic or cement mantle lucency, bead shedding, endosteal scalloping, and endosteal bone bridging at the tip of the stem.
Definite signs of radiographic loosening include progressive periprosthetic or cement mantle lucency, change in position of the stem, and component or cement mantle fracture (FIG 2). Radiographic signs of probable loosening include greater than 2 mm of periprosthetic or cement mantle lucency, bead shedding, endosteal scalloping, and endosteal bone bridging at the tip of the stem.

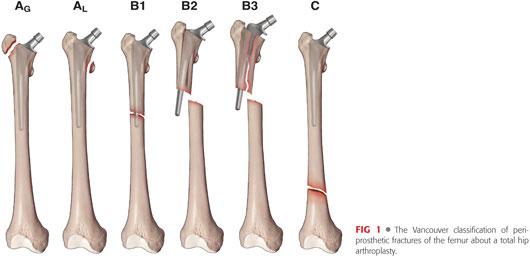
 Whenever possible, preinjury radiographs should be obtained to assess for change in component position, as this is the best indication of a loose stem. Careful comparison of implant position on injury and preinjury radiographs is required, as the findings of implant subsidence can range from noticeable to relatively subtle (FIGS 3 and 4).
Whenever possible, preinjury radiographs should be obtained to assess for change in component position, as this is the best indication of a loose stem. Careful comparison of implant position on injury and preinjury radiographs is required, as the findings of implant subsidence can range from noticeable to relatively subtle (FIGS 3 and 4).

 Efforts should be made to obtain original operative reports in case revision of the implant is required.
Efforts should be made to obtain original operative reports in case revision of the implant is required.
 Inflammatory markers such as white cell count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are often elevated in the setting of trauma, and therefore can be difficult to interpret in the setting of a fracture unless they are significantly elevated. If concern for infection exists on the basis of preinjury symptoms, a preoperative hip aspiration can be obtained or the surgeon should be prepared to proceed with a two-stage revision should infection be encountered at the time of surgery (see FIG 2).
Inflammatory markers such as white cell count, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are often elevated in the setting of trauma, and therefore can be difficult to interpret in the setting of a fracture unless they are significantly elevated. If concern for infection exists on the basis of preinjury symptoms, a preoperative hip aspiration can be obtained or the surgeon should be prepared to proceed with a two-stage revision should infection be encountered at the time of surgery (see FIG 2).
DIFFERENTIAL DIAGNOSIS
 Periprosthetic infection
Periprosthetic infection
 Aseptic loosening
Aseptic loosening
 Pathologic fracture
Pathologic fracture
NONOPERATIVE MANAGEMENT
 Operative intervention is indicated for the vast majority of periprosthetic fractures of the femur with the exception of stable fractures of the lesser trochanter without shaft extension, minimally displaced fractures of the greater trochanter, and completely undisplaced fractures around the stem of a stable implant. In addition, minimally displaced fractures about the femoral stem in patients who are poor surgical candidates can be considered for a trial of conservative management.
Operative intervention is indicated for the vast majority of periprosthetic fractures of the femur with the exception of stable fractures of the lesser trochanter without shaft extension, minimally displaced fractures of the greater trochanter, and completely undisplaced fractures around the stem of a stable implant. In addition, minimally displaced fractures about the femoral stem in patients who are poor surgical candidates can be considered for a trial of conservative management.
SURGICAL MANAGEMENT
 The surgical management of periprosthetic femur fractures about a total hip arthroplasty is guided by the Vancouver classification.
The surgical management of periprosthetic femur fractures about a total hip arthroplasty is guided by the Vancouver classification.
 Type AL fractures of the lesser trochanter are generally managed nonsurgically as are minimally displaced type AG fractures of the greater trochanter. Displaced type AG fractures are generally managed with open reduction and internal fixation (ORIF) +/− bone grafting and polyethylene liner exchange if they are associated with osteolysis and liner wear.
Type AL fractures of the lesser trochanter are generally managed nonsurgically as are minimally displaced type AG fractures of the greater trochanter. Displaced type AG fractures are generally managed with open reduction and internal fixation (ORIF) +/− bone grafting and polyethylene liner exchange if they are associated with osteolysis and liner wear.
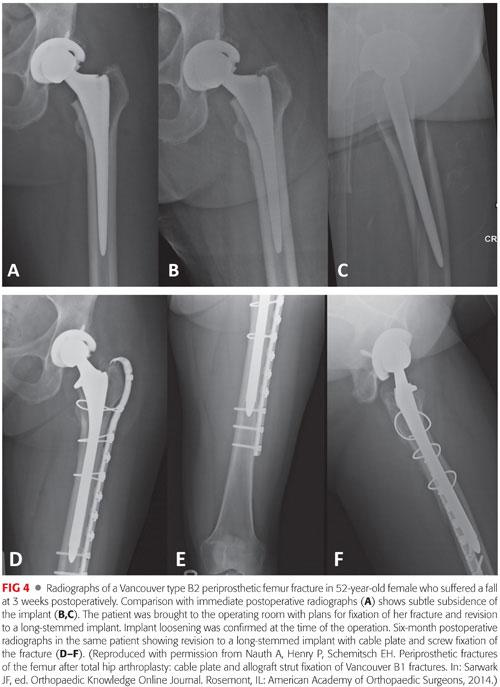
 Type B1 fractures have a stable implant and are managed with fracture fixation. The focus of this techniques chapter is on the fixation of these fracture types and techniques for type B1 fracture fixation are described below in detail. There is relative controversy in the literature regarding the optimal technique for fixation of Vancouver type B1 fractures, with the main controversy centered around the use of cable plating combined with allograft strut versus isolated lateral locked plating. The biomechanical literature suggests that the use of a lateral cable plate and screws combined with the use of an anterior allograft strut (90–90 fixation) is the optimal biomechanical construct.7 Buttaro et al2 retrospectively reviewed a 14 patient series of type B1 fractures treated with lateral locked plating +/− the use of a cortical strut. The authors reported a high rate of failure when isolated lateral locked plating was used (five of nine constructs) versus when lateral plating was combined with the use of a cortical strut (one of five constructs). In contrast, other authors have reported a very high rate of success when isolated lateral plating is combined with indirect reduction and biologically friendly techniques.6 High-level prospective evidence comparing the two techniques is lacking. Irrespective of the fixation strategy used, several biomechanical and surgical principles must be adhered to when treating these fractures. First, it is critical that the fracture is fixed without the stem in varus, as increased rates of fixation failure have been reported with varus positioning of the stem. Second, proximal fixation around the stem is best achieved with a combination of wires/cables and screws, and it is critical that sufficient overlap of the femoral prosthesis is obtained to avoid mechanical failure (FIG 5). This generally requires fixation to the level of the greater trochanter. Third, it is important to remember that these fractures commonly occur in pathologic/osteopenic bone, and the use of a plate of sufficient length to stabilize the entire length of the femur is recommended to avoid future peri-implant fracture. Finally, it is important to adhere to the principles of absolute versus relative stability depending on the type of fracture healing desired. In the setting of a simple transverse or spiral fracture, absolute stability and compression at the fracture site should be achieved using compression plating or lag screw fixation. This is in contrast to comminuted fractures which require relative stability and spaced fixation to allow for fracture healing indirectly by callus formation.
Type B1 fractures have a stable implant and are managed with fracture fixation. The focus of this techniques chapter is on the fixation of these fracture types and techniques for type B1 fracture fixation are described below in detail. There is relative controversy in the literature regarding the optimal technique for fixation of Vancouver type B1 fractures, with the main controversy centered around the use of cable plating combined with allograft strut versus isolated lateral locked plating. The biomechanical literature suggests that the use of a lateral cable plate and screws combined with the use of an anterior allograft strut (90–90 fixation) is the optimal biomechanical construct.7 Buttaro et al2 retrospectively reviewed a 14 patient series of type B1 fractures treated with lateral locked plating +/− the use of a cortical strut. The authors reported a high rate of failure when isolated lateral locked plating was used (five of nine constructs) versus when lateral plating was combined with the use of a cortical strut (one of five constructs). In contrast, other authors have reported a very high rate of success when isolated lateral plating is combined with indirect reduction and biologically friendly techniques.6 High-level prospective evidence comparing the two techniques is lacking. Irrespective of the fixation strategy used, several biomechanical and surgical principles must be adhered to when treating these fractures. First, it is critical that the fracture is fixed without the stem in varus, as increased rates of fixation failure have been reported with varus positioning of the stem. Second, proximal fixation around the stem is best achieved with a combination of wires/cables and screws, and it is critical that sufficient overlap of the femoral prosthesis is obtained to avoid mechanical failure (FIG 5). This generally requires fixation to the level of the greater trochanter. Third, it is important to remember that these fractures commonly occur in pathologic/osteopenic bone, and the use of a plate of sufficient length to stabilize the entire length of the femur is recommended to avoid future peri-implant fracture. Finally, it is important to adhere to the principles of absolute versus relative stability depending on the type of fracture healing desired. In the setting of a simple transverse or spiral fracture, absolute stability and compression at the fracture site should be achieved using compression plating or lag screw fixation. This is in contrast to comminuted fractures which require relative stability and spaced fixation to allow for fracture healing indirectly by callus formation.
 Vancouver type B2 fractures are treated with revision to a long-stemmed prosthesis and fixation of the fracture (see FIGS 3 and 4). The stem should bypass the fracture by at least two cortical diameters.
Vancouver type B2 fractures are treated with revision to a long-stemmed prosthesis and fixation of the fracture (see FIGS 3 and 4). The stem should bypass the fracture by at least two cortical diameters.
 Type B3 fractures require revision, ORIF, and possible structural allograft to restore bone stock.
Type B3 fractures require revision, ORIF, and possible structural allograft to restore bone stock.
 Vancouver type C fractures occur well below the stem and can be generally treated with isolated ORIF.
Vancouver type C fractures occur well below the stem and can be generally treated with isolated ORIF.
Preoperative Planning
 As indicated previously, multidisciplinary assessment is recommended to manage patient comorbidities and perioperative medical issues.
As indicated previously, multidisciplinary assessment is recommended to manage patient comorbidities and perioperative medical issues.
 At all times when managing periprosthetic fractures of the femur about a total hip arthroplasty, the surgeon should be prepared for the possible need for revision. This requires careful review of the initial operative report to ensure that revision implants of the appropriate type are available for possible revision of the femoral stem. Corten et al3 reported that 20% of implants judged to be stable based on preoperative radiographs were found to be loose at the time of surgery. If any doubt exists regarding the stability of the femoral component, an arthrotomy of the hip with dislocation and stressing of the implant should be performed to rule out a loose femoral component.
At all times when managing periprosthetic fractures of the femur about a total hip arthroplasty, the surgeon should be prepared for the possible need for revision. This requires careful review of the initial operative report to ensure that revision implants of the appropriate type are available for possible revision of the femoral stem. Corten et al3 reported that 20% of implants judged to be stable based on preoperative radiographs were found to be loose at the time of surgery. If any doubt exists regarding the stability of the femoral component, an arthrotomy of the hip with dislocation and stressing of the implant should be performed to rule out a loose femoral component.
Positioning
 The patient is positioned supine on a radiolucent (Jackson) table with a bump or inflated beanbag under the affected side to elevate the fractured limb (FIG 6). The limb is free-draped, and intraoperative fluoroscopy is placed on the contralateral side to the fracture.
The patient is positioned supine on a radiolucent (Jackson) table with a bump or inflated beanbag under the affected side to elevate the fractured limb (FIG 6). The limb is free-draped, and intraoperative fluoroscopy is placed on the contralateral side to the fracture.

 Alternatively, the patient can be positioned in the lateral decubitus position with the affected limb facing up and free-draped. This is the position of choice, if revision of the femoral component is planned.
Alternatively, the patient can be positioned in the lateral decubitus position with the affected limb facing up and free-draped. This is the position of choice, if revision of the femoral component is planned.
Approach
 The approach involves a lateral incision using the distal aspect of the previous total hip arthroplasty incision extended distally toward the knee.
The approach involves a lateral incision using the distal aspect of the previous total hip arthroplasty incision extended distally toward the knee.
 If an arthrotomy is required for dislocation of the hip and evaluation of femoral component stability or for femoral component revision, the proximal aspect of the total hip incision can be used as well.
If an arthrotomy is required for dislocation of the hip and evaluation of femoral component stability or for femoral component revision, the proximal aspect of the total hip incision can be used as well.
 If a minimally invasive approach and indirect reduction is being employed, then the distal aspect of the total hip incision is used to access the femur proximal to the fracture and a separate distal incision is made at the lateral aspect of the distal femur for distal plate placement.
If a minimally invasive approach and indirect reduction is being employed, then the distal aspect of the total hip incision is used to access the femur proximal to the fracture and a separate distal incision is made at the lateral aspect of the distal femur for distal plate placement.
TECHNIQUES
 Cable Plating and Allograft Strut Fixation
Cable Plating and Allograft Strut Fixation
Surgical exposure: A lateral exposure is carried out to expose the entire femur extending from the distal aspect of the previous total hip arthroplasty incision to the level of the distal femur. For deep dissection, the fascia lata is split in line with the skin incision and the vastus lateralis is elevated anteriorly with dissection carried out along the posterior fibers (TECH FIG 1C). Perforating vessels are identified and coagulated. The entire lateral aspect of the femur, including the fracture, is exposed from the level just below the greater trochanter to the level of the metaphyseal flair. The lateral and anterior aspects of the femur are exposed. Although the exposure is extensile, care is taken to avoid stripping the soft tissues on the posterior and medial aspects of the femur (TECH FIG 1D).
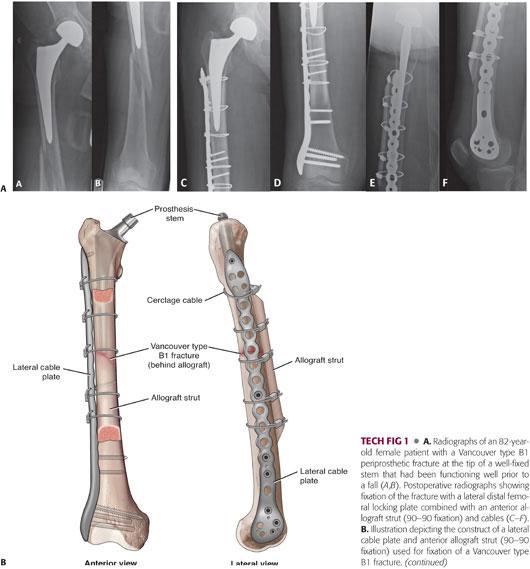
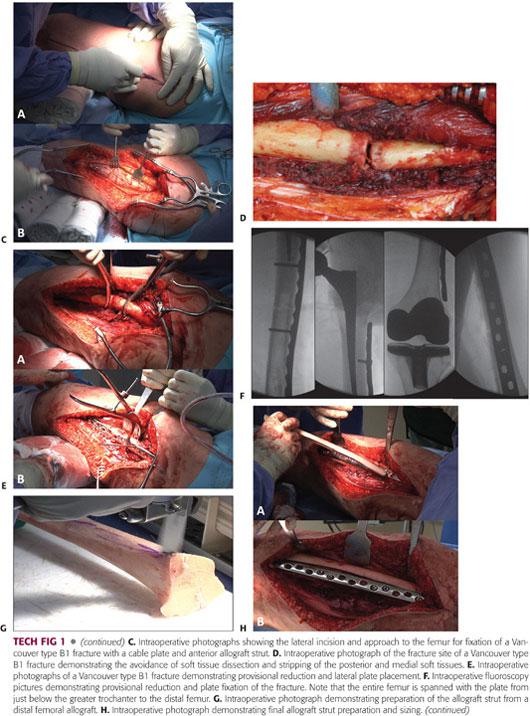
Fracture reduction and plate application: If doubt exists regarding the stability of the implant, the bone implant interface is carefully examined through the fracture site for any evidence of loosening. If loosening is suspected, proximal extension of the incision is carried out with an arthrotomy to evaluate implant stability at the level of the hip. Once implant stability is confirmed, fracture reduction is achieved with the use of reduction clamps (TECH FIG 1E). A plate of appropriate length is chosen to span the entire femur from the distal femur to the level just below the greater trochanter (it is critical to ensure adequate overlap of the plate with the femoral stem to avoid mechanical failure). Plate contouring is performed as necessary depending on the plate chosen to allow application of the plate to the lateral aspect of the femur. Newer generation precontoured locking plates have a contour to accommodate the anterior bow of the native femur. Provisional screw fixation is obtained through the plate both proximal and distal to the fracture. If the fracture pattern is amenable to absolute stability, then compression at the fracture site is obtained at this stage using the compression holes in the plate, lag screws, or an articulated tensioning device. Fluoroscopy is then used to confirm anatomic reduction and alignment as well as satisfactory positioning of the plate (TECH FIG 1F).
Allograft preparation: Allograft preparation is begun as soon as the approach to the femur is complete and both infection and implant loosening have been definitively ruled out. The authors’ preference is to use the anterior cortex of a distal femoral allograft as this provides a graft which accommodates the anterior bow of the femur and also allows for cancellous allograft to be obtained from the distal femur (TECH FIG 1G). Tibial or humeral strut allografts are acceptable alternatives. A strut allograft of appropriate length to allow adequate graft overlap with the femoral prosthesis and passage of two cables on either side of the fracture is necessary (generally, a minimum length of 25 to 30 cm is required). In addition, it is advisable to avoid ending the allograft at the same level distally as the plate and creating a stress riser. The anterior cortex of the distal femoral allograft is prepared using an oscillating saw and burr. Appropriate sizing and contouring of the graft is confirmed with provisional placement on the anterior cortex of the femur (TECH FIG 1H).
Cable passage and allograft placement: Prior to definitive allograft placement, cables are passed around the femur using a cable passer, as these are more easily passed prior to graft placement. It is critical that these cables are passed directly on the bone to avoid entrapment of neurovascular structures (TECH FIG 1I). The authors typically use two cables proximal to the fracture and two cables distal to the fracture. The graft is then placed on the anterior aspect of the femur creating a 90–90 construct. The cables are then sequentially tightened, locked, and trimmed (TECH FIG 1J). At this stage, supplemental screw fixation is placed proximal and distal to the fracture. Proximally, this involves placing nonlocked screws or polyaxial locking screws around the well-fixed femoral stem or the use of unicortical locking screws. Intraoperative fluoroscopy is then used to confirm anatomic reduction and alignment of the fracture and satisfactory positioning of the plate, screws, cables, and allograft strut. At this point, the wound is irrigated copiously with normal saline. Cancellous allograft harvested from the distal femoral allograft is then placed at the fracture site and at the graft–host interface. A standard closure is then performed in layers.
 Minimally Invasive Isolated Lateral Locking Plate Fixation
Minimally Invasive Isolated Lateral Locking Plate Fixation
Surgical approach: A lateral exposure of the proximal femur is made using the distal aspect of the total hip arthroplasty incision with extension just proximal to the fracture. Deep dissection is carried out through fascia lata and posterior to vastus lateralis to expose the proximal femur from the level of the greater trochanter to just proximal to the fracture site. Care is taken to preserve the soft tissues and vascular supply at the fracture site. A distal incision of 4 to 5 cm is made at the level of the metaphyseal flare to expose the lateral aspect of the distal femur (TECH FIG 2C). A cobb elevator is then used to create a submuscular plane along the lateral aspect of the femur.

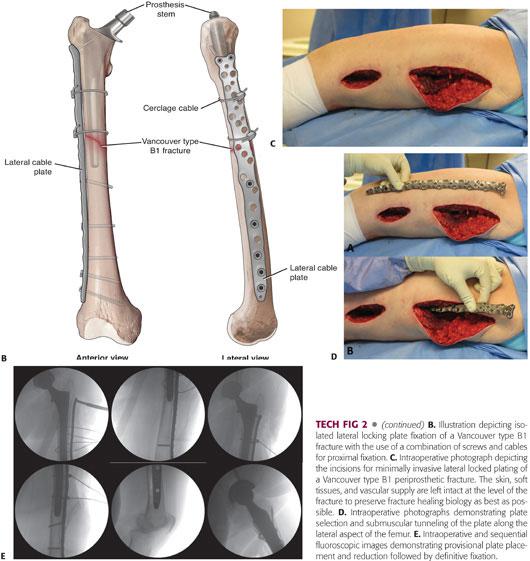
Plate placement and indirect reduction: A lateral locking plate of appropriate length to span the entire femur is selected, contoured, and tunneled in the submuscular plane from the proximal incision to the distal incision (TECH FIG 2D). An indirect reduction is performed with traction of the limb and use of the plate as a reduction aid. The plate is reduced to the femur using a nonlocking screw distally and with the use of a cable or reduction clamp proximally (TECH FIG 2E). Fluoroscopy is used to confirm reduction in the coronal and sagittal planes.
Cable placement and definitive fixation: Once reduction is confirmed fluoroscopically, definitive fixation is carried out with a combination of locking and nonlocking screws distally and the use of cables and locking screws placed around the femoral component proximally. Newer generation periprosthetic locking plates allow for the placement of polyaxial locking screws around the prosthesis. Both cables and screws should be used to optimize proximal fixation, with the use of two to four cables combined with two to four screws based on bone quality. Distal fixation is obtained with a combination of locking and nonlocking screws, again based on bone quality. Spaced fixation and a screw density of 50% (ie, half of the distal screw holes should be left empty) should be used to prevent a large concentration of stress over a small length of plate at the fracture site (see TECH FIG 2A). Final fluoroscopic images (see TECH FIG 2E) are obtained and a standard layered closure is performed.
PEARLS AND PITFALLS | |
Periprosthetic fracture patient management |
|
| |
| |
| |
Implant loosening |
|
Fracture fixation |
|
| |
| |
| |
| |
| |
Cable plating and allograft strut |
|
| |
| |
| |
Isolated lateral locked plating |
|
| |
| |
| |
POSTOPERATIVE CARE
 Postoperatively, the patient is typically kept touch weight bearing for a period of 6 weeks with range of motion of the knee and hip as tolerated. At 6 weeks, the patient is progressed to weight bearing as tolerated. The authors will allow patients treated with cable plating and strut allograft to weight bear as tolerated immediately after surgery, which is one of the advantages of using this construct as if facilitates more rapid mobilization and rehabilitation of the patient.
Postoperatively, the patient is typically kept touch weight bearing for a period of 6 weeks with range of motion of the knee and hip as tolerated. At 6 weeks, the patient is progressed to weight bearing as tolerated. The authors will allow patients treated with cable plating and strut allograft to weight bear as tolerated immediately after surgery, which is one of the advantages of using this construct as if facilitates more rapid mobilization and rehabilitation of the patient.
OUTCOMES
 As discussed before, Bhattacharyya et al1 have demonstrated that patients presenting with a periprosthetic fracture about a total hip arthroplasty have similar rates of morbidity and mortality to that of the hip fracture population, with a 1-year mortality rate of approximately 11%.
As discussed before, Bhattacharyya et al1 have demonstrated that patients presenting with a periprosthetic fracture about a total hip arthroplasty have similar rates of morbidity and mortality to that of the hip fracture population, with a 1-year mortality rate of approximately 11%.
 One-year mortality has been shown to be increased with delays to surgery of greater than 48 hours and it is vital that these patients receive surgery as soon as possible.1
One-year mortality has been shown to be increased with delays to surgery of greater than 48 hours and it is vital that these patients receive surgery as soon as possible.1
COMPLICATIONS
 Variable outcomes have been reported in the literature with regard to complication and reoperation rates. Pooled assessment of the literature on outcomes following fixation of Vancouver type B1 fractures (based on a sample size of 333 patients) suggests the following rates:
Variable outcomes have been reported in the literature with regard to complication and reoperation rates. Pooled assessment of the literature on outcomes following fixation of Vancouver type B1 fractures (based on a sample size of 333 patients) suggests the following rates:
Overall complication rate = 15%
Reoperation rate = 9%
Nonunion or hardware failure = 9%
Malunion = 6%
Infection = 5%
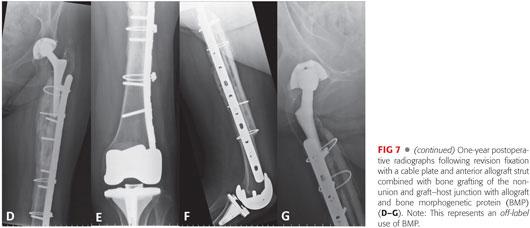
 Nonunion or hardware failure is reliably treated with revision ORIF using cable plating, strut allograft, and bone grafting (or use of an osteoinductive bone graft substitute) of the nonunion site (FIG 7).
Nonunion or hardware failure is reliably treated with revision ORIF using cable plating, strut allograft, and bone grafting (or use of an osteoinductive bone graft substitute) of the nonunion site (FIG 7).

REFERENCES
1. Bhattacharyya T, Chang D, Meigs JB, et al. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg 2007;89(12):2658–2662.
2. Buttaro MA, Farfalli G, Paredes Nunez M, et al. Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint Surg Am 2007;89(9):1964–1969.
3. Corten K, Vanrykel F, Bellemans J, et al. An algorithm for the surgical treatment of periprosthetic fractures of the femur around a well-fixed femoral component. J Bone Joint Surg Br 2009;91(11):1424–1430.
4. Lindahl H, Malchau H, Odén A, et al. Risk factors for failure after treatment of a periprosthetic fracture of the femur. J Bone Joint Surg Br 2006;88(1):26–30.
5. Masri BA, Meek RM, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res 2004;(420):80–95.
6. Ricci WM, Bolhofner BR, Loftus T, et al. Indirect reduction and plate fixation, without grafting, for periprosthetic femoral shaft fractures about a stable intramedullary implant. J Bone Joint Surg Am 2005;87(10):2240–2245.
7. Zdero R, Walker R, Waddell JP, et al. Biomechanical evaluation of periprosthetic femoral fracture fixation. J Bone Joint Surg Am 2008;90(5):1068–1077.
< div class='tao-gold-member'>






















