Key Words
breast reconstruction, nipple reconstruction, areolar reconstruction, skate flap, C-V flap
Introduction
Nipple–areola complex (NAC) reconstruction can be an important part of breast reconstruction and will definitely add an aesthetic component of breast reconstruction. Without NAC reconstruction, it usually gives the impression that the breast reconstruction has not been completed. Therefore, NAC reconstruction can be an important component of breast reconstruction and should be considered an important part of any type of breast reconstruction.
Although a number of techniques for NAC reconstruction have been described in the literature, only two methods are commonly used by most plastic surgeons and have frequently been studied. One is the skate flap in which the nipple is reconstructed by a local flap like a skate and the areolar circle is reconstructed with a full-thickness skin graft. The C-V flap was described as a modification of the skate flap to reduce the need for skin grafting the areola. It is a random “flap-on-a-flap,” where the “C” portion of the flap derives its blood supply from the “V” flap, which is a random flap. The areola circle after a C-V flap reconstruction can be tattooed later. Each type of NAC reconstruction may be equally good based on the patient’s selection and the surgeon’s experience and preference. In general, NAC reconstruction can be performed based on an autologous breast reconstruction since there is adequate tissue for such a reconstruction with higher patient satisfaction. However, for an implant-based reconstruction, the NAC reconstruction may present a challenge because there is lack of tissue over the breast implant for such a reconstruction with the lowest patient satisfaction. In addition, the scar pattern over the previous breast reconstruction may also impact the location and outcome of NAC reconstruction.
In this chapter, the skate flap with a skin graft and the C-V flap, the two most commonly performed NAC reconstructions, are described. The authors have also added their modifications to each type of NAC reconstruction so that a better reconstructive outcome can be achieved. Each surgical technique will be described in detail and several refinements are also described.
Indications and Contraindications
NAC reconstruction is indicated for almost all patients after their autologous or implant-based breast reconstruction. In general, the timing of such a reconstruction is about 2–3 months after initial or secondary breast reconstruction once no major revision for the reconstructed breast in terms of its size and shape is needed. If radiation has been performed on the reconstructed breast we prefer to postpone the NAC reconstruction for about a year once the radiation damage to the breast skin has been resolved so that overall complication of NAC reconstruction, such as delayed wound healing, can be minimized. If healing of the incision or radiation changes over the reconstructed breast has not been relatively mature or resolved, the timing of NAC reconstruction can be further postponed.
Preoperative Evaluation and Special Considerations
One of the major issues is determining whether the patient will have adequate soft tissue over the reconstructed breast that can be used for a nipple reconstruction. This can be done with a pinch test. If the thickness of the soft tissue over the reconstructed breast is less than 0.5 cm, which can be a common finding for implant-based breast reconstruction, limited projection after any type of NAC reconstruction may be expected. For bilateral nipple reconstructions, very often the location of the scar over the reconstructed breast can be problematic because it may interfere with the determination of new nipple position over the reconstructed breast. Sometimes the design of the new nipple position can be above or below the scar to avoid a high-ride look to the reconstructed nipple and the design of a local flap for NAC reconstruction can be modified.
For unilateral nipple reconstruction with consideration of where the new nipple should be on the reconstructed breast, obviously it will be based on the measurement in reference to the breast mound of the reconstructed breast and also to the contralateral side of the breast. Ideally, the new nipple position should be at the highest peak of the breast mound. However, it also can be placed higher or lower than the peak of the breast mound although the lower placement of the new nipple position is preferred to avoid a high-ride position of the reconstructed nipple.
When planning a new NAC reconstruction, attention should be made during the preoperative evaluation to make sure such a local skin flap used for nipple reconstruction can be elevated safely and healed without delay. If a skin graft is needed, it can be harvested from any location in which the patient has a scar. Very commonly, the authors prefer to harvest a full-thickness skin graft from the suprapubic area, the lateral aspect of abdominal incision, or the inguinal area.
Surgical Technique
Relevant Surgical Anatomy
The blood supply to the reconstructed nipple from local skin over the reconstructed breast is from the subdermal plexus regardless of the design for each type of reconstruction. Since the skin flap over the reconstructed breast is elevated to reconstruct the nipple, attention should be made to make sure that the flap is based wide enough to receive adequate blood supply so that the flap can survive after its elevation and closure. This is especially important for an implant-based reconstruction since the local skin flap should be elevated wider and thicker enough for nipple reconstruction. In addition, the flap should incorporate as much local subcutaneous tissue and/or dermis as possible to reconstruct an adequate-sized nipple since the reconstructed nipple can shrink up to 50% after reconstruction. It is important to base the skin flap away from the scar or the area with previous radiation injury.
Operative Technique
The Skate Flap
A skate flap is designed according to the symmetry and also the location of the scar over the reconstructed breast ( Fig. 21.1A ). The size of the flap is designed between 1 and 1.5 cm and the diameter of the new areolar circle is 3.8 or 4.8 cm depending on the expected final size and projection of the reconstructed nipple ( Fig. 21.1B ). The upper third of the skin within the designed areolar circle is de-epithelialized ( Fig. 21.1C ). A skin-only flap from both sides is then quickly raised with knife to the line on each side when a true skin flap with adequate fat is carefully railed with scissors. Within the base of the flap, each triangular shape of flap is then elevated and attention is made to carry adequate fat along with each skin flap ( Fig. 21.1D ). Each side of the skin flap is approximated in the volar aspect of the reconstructed nipple and the posterior skin flap is then approximated anteriorly to join the valor approximation. At this point, excess skin in each corner is marked ( Fig. 21.1E ) and precise de-epithelialization is then performed ( Fig. 21.1F ). In this way, additional healthy vascularized tissue can be inserted to add projection of the reconstructed nipple ( Fig. 21.1G ).
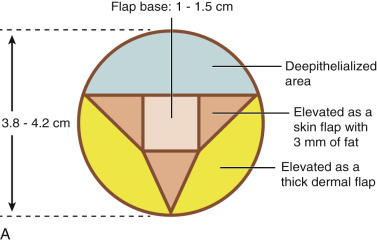









A 38- or 42-mm cookie cutter is used to outline the full-thickness skin graft site. A full-thickness skin graft is then harvested and defatted ( Fig. 21.1H ). Its incision site is closed in two layers accordingly. The skin graft is then placed through the reconstructed nipple to form the new alveolar circle and closed in both inner and outer circles with absorbable suture ( Fig. 21.1I ). At the end of the procedure, the reconstructed nipple is protected with a nipple protector and the areolar skin graft is immobilized with Steri-Strips ( Fig. 21.1J ).
If NAC reconstruction is performed over an implant-based reconstruction, derma-fat graft can be added to the reconstructed nipple before its final closure to add projection for possible better long-term results. It can be conveniently harvested during a skin graft harvest for areolar reconstruction. Within a planned excision of a full-thickness skin graft, a derma-fat graft (4 × 3 × 3 mm) can be made first after de-epithelialization ( Fig. 21.2A ). In general, two pieces would be needed for each nipple reconstruction and more optimal projection can be achieved with this approach ( Fig. 21.2B,C ). In addition, the design of a skate flap can also be orientated inferiorly to accommodate the location of a mastectomy scar ( Fig. 21.3 ).