Abstract
Naso-orbito-ethmoid (NOE) fractures, although less common in isolation, are a frequent component of other midface fractures and can be some of the most difficult facial fracture patterns to treat successfully. The prominent location on the face, the complex 3-dimensional structure and the attachment of delicate periorbital structures increase the complexity of the fractures and difficulty of treatment. Two classification systems (Manson and Gruss) describe the increasing severity of NOE fractures based on integrity of the medial canthal tendon and overall stability of the midface due to associated fractures respectively. Clinical findings of traumatic telecanthus, saddle nose deformity, and rounded palpebral fissure must be corrected acutely as these are almost impossible to correct secondarily. Delay and malreduction produce fixed deformity with thickened scarred soft tissue. Various surgical approaches and reduction techniques are often necessary to attain anatomic reduction of the NOE fractures, but successful treatment can lead to excellent surgical results.
Keywords
naso-orbito-ethmoid fracture, naso-orbital ethmoid, NOE, facial trauma, craniofacial trauma, maxillofacial trauma, craniomaxillofacial trauma, telecanthus, medial canthal tendon, medial canthoplasty, saddle nose deformity, epiphora, palpebral fissure
Background
The naso-orbito-ethmoid (NOE) region of the central face is defined by the orbits laterally, the glabella superiorly and the nose inferiorly. It is a particularly challenging region of the face to reconstruct due to its aesthetic prominence, its 3-dimensional contour and the delicate associated structures involved in the region. NOE fractures occur from direct blunt force trauma to the central face, such as striking the dashboard in a motor vehicle collision (MVC). While isolated NOE fractures accounted for only (5.8%) of all facial fractures at a busy trauma center, they are a frequent component of associated midface fractures and must be accurately diagnosed and treated to attain anatomic fracture reduction.
Surgical Anatomy
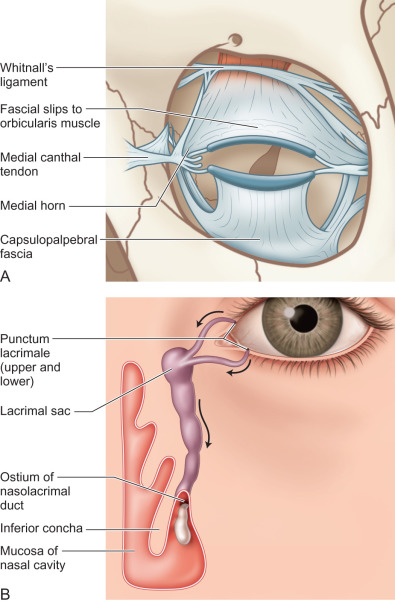
The NOE complex is comprised of the frontal process of the maxilla, internal angular process of the frontal bone, the ethmoid sinuses, and the lacrimal bone ( Fig. 1.11.1 ). As such, it contributes to the shape and volume of the medial orbits, the contour of the inferior orbital rim, the patency of the pyriform aperture, and the support of the nasal dorsum. Additionally, it serves as the drainage of the frontal sinus and the attachment of the medial canthal tendon and the trochlea, and the location of the nasolacrimal apparatus are associated structures ( Fig. 1.11.2 ).

Clinical Presentation
Patients present after blunt force trauma to the central face. They will often complain of diplopia, nasal airway obstruction, and alteration of physical appearance. They may report numbness of the central face and forehead, epiphora, and CSF rhinorrhea.
After a complete ATLS evaluation with particular attention paid to the C-spine, a focused craniofacial examination is performed. Begin with inspection of the eyes, noting telecanthus, rounding of the palpebral fissure, and lid malposition. If avulsion of the medial canthal tendon is suspected, the examiner can use forceps to pull on the tendon, noting presence or absence of a firm stop ( ). Assess visual acuity and test extraocular muscle integrity looking for entrapment. Measure globe position noting enophthalmos or exophthalmos. The presence of an orbital fracture merits an ophthalmological consultation to rule out injury to the eye, visual system, and retina.
The examiner should note asymmetry of the nose and presence of a saddle nose deformity ( Fig. 1.11.3 ). Sequentially, assess nasal airway patency and perform a speculum exam noting integrity of the septum, nasal perforation, and presence of a septal hematoma, which requires prompt drainage. The presence of a collapsed/telescoped septal fracture may require dorsal or caudal nasal cantilever bone grafting to maintain nasal support. Proceed next with gentle palpation of the craniofacial skeleton noting point tenderness, crepitus, and bony step-offs.

Radiological Evaluation
If, after physical exam, an NOE fracture is suspected, one should obtain a fine cut (0.5 mm) maxillofacial computed tomography (CT) scan extending from vertex through menton. Plain films are of no utility. Axial and coronal views are both required and additional sagittal and 3D views may be helpful if orbital involvement is extensive and/or the fractures are complicated. The skull should be included to assess for viable split calvarial bone graft harvest sites for possible nasal and orbital reconstruction.
Classification
The severity of NOE fractures is determined by CT scan evaluation based on either the Manson or Gruss classification system. In the Gruss classification, severity is graded into five types based on the presence of increasingly difficult surrounding midface fractures ( Table 1.11.1 ). As severity increases, additional surgical maneuvers such as orbital repositioning or bone grafting may be required. In the Manson classification system, focus is placed on the medial canthal tendon. Severity is graded into three types based on the degree of comminution of the NOE segment and the integrity of the medial canthal attachment ( Fig. 1.11.4 ). Similarly, with increasing severity, the Manson classification system predicts additional surgical maneuvers such as open reduction internal fixation, transnasal wires, and medial canthoplasty.
| Type 1: | Isolated bony NOE injury |
| Type 2: | Bony NOE injury and central maxilla |
| 2a: | Central maxilla only |
| 2b: | Central maxilla and one lateral maxilla |
| 2c: | Central and bilateral lateral maxillae |
| Type 3: | Extended NOE injury |
| 3a: | With craniofacial injuries |
| 3b: | With LeFort II and III fractures |
| Type 4: | NOE injury with orbital displacement |
| 4a: | With oculo-orbital displacement |
| 4b: | With orbital dystopia |
| Type 5: | NOE injury with bone loss |

Surgical Indications
Once an NOE fracture is diagnosed, the surgeon must decide whether an operative intervention is warranted. Generally, this decision is based on amount of displacement and degree of comminution. A nondisplaced, nonmobile NOE fracture can be treated nonoperatively. A minimally impacted, large segment NOE fracture may be treated with closed reduction and splint stabilization ( Fig. 1.11.5 ), whereas a displaced, comminuted NOE fracture may require operative fixation via one or multiple surgical approaches ( Fig. 1.11.6 ).


In addition to displacement and comminution, the effects of the NOE fracture on various facial features are taken into consideration when deciding operative management. With regards to the orbit, NOE fractures affect orbital volume, medial canthal position, and inferior rim support. As the ethmoid bulge is diminished, orbital volume increases which can lead to enophthalmos and such fractures should be treated with bone graft or alloplastic implant to the medial orbital wall. Rotation of the NOE segment can change the 3-dimensional ogee of the naso-orbital region and create a bony step-off at the inferior rim. This rotation can also lead to telecanthus as can comminution or detachment of the medial canthal tendon, all of which require surgical intervention to reestablish normal intercanthal distance (35–40 mm in adults).
With regards to the nose, NOE fractures can affect the patency of the airway and the stability of the nasal tip and dorsum. Fracture segments that impact into the pyriform can narrow the airway. If obstruction is noted on exam, then the segment must be reduced and fixated to reestablish the normal lateral pyriform contour. With severe comminution and concomitant septal fracture, loss of dorsal support can lead to a saddle nose deformity ( Fig. 1.11.7 ), which is difficult, if not impossible, to correct secondarily once the soft tissue envelope contracts and must therefore be treated acutely.











