Nails
OVERVIEW
Mammals use their nails as weapons, as primitive tools, for grooming purposes, for scratching, and for the removal of infestations. Humans use their fingernails to help pick up small objects and to scratch itchy skin. As with fingernails, the toenails are in constant contact with and exposed regularly to contactants and trauma. Fingernails protect vulnerable fingertips; toenails protect toes from the impact of footwear and external trauma. Nails are also important contributors to the aesthetic appearance of the hands and feet.
Inflammatory disorders that involve the nail matrix (root), such as psoriasis and eczema, can result in distinctive deformities of the nails. To the health care provider, nails may represent clinical findings of a skin disorder or be a signal to an underlying systemic disease.
COMMON NAIL PROBLEMS
Longitudinal Ridging (Onychorrhexis)
Longitudinal ridging is a quite common nail issue that is considered a normal variant in elderly persons. It consists of parallel ridges that run lengthwise along the nail plates. They are more commonly observed in fingernails than in toenails (Fig. 15-1).
Management
There is no treatment available to decrease longitudinal ridging, except for filing and buffing the ridges down with a soft file
Brittle Nails (Onychoschizia)
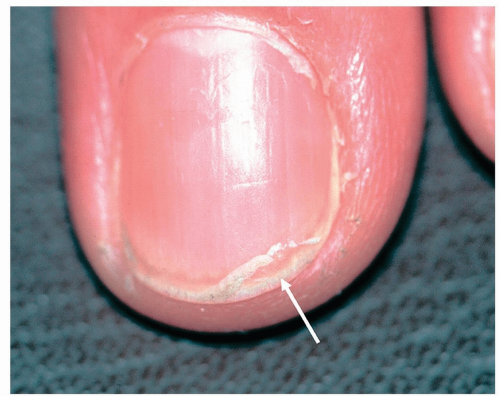
Brittle nails (onychoschizia), distal nail splitting (Fig. 15-2), can be compared to scaly, dry skin elsewhere on the body. Thus, many treatment recommendations are similar to those for dry skin.
Management
Moisturizing creams or ointments (e.g., lactic acid creams in 5% to 12% concentrations or Vaseline Petroleum Jelly) at bedtime or after bathing or washing. Excessive washing and drying of the nails should be avoided to prevent brittle nails
The nails should be kept short and trimmed when they are well hydrated, so they are less likely to be frayed
 Figure 15-1 Longitudinal ridging (onychorrhexis). Parallel ridges running lengthwise along the nail plate. |
Onycholysis
Onycholysis represents a separation of the nail plate from its attachment to the underlying pink nail bed (Fig. 15-3). It has a number of causes. Most commonly it is initiated by trauma such as over vigorous cleaning with an instrument beneath the nail plate. This can weaken the adhesion of the nail plate to the underlying nail bed. Exposure to chemicals, especially those in nail cosmetic products, can further irritate the delicate nail bed tissue and cause separation.
Distinguishing Features
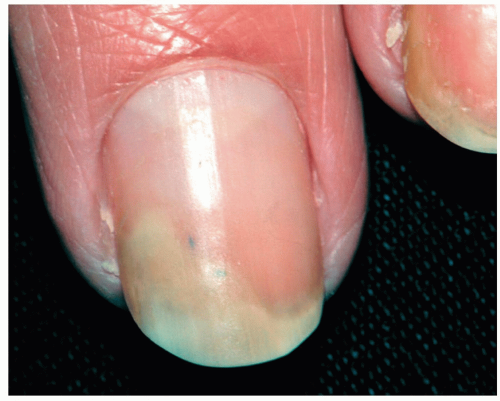 Figure 15-3 Onycholysis. The separated portion of the nail is yellowish white and opaque; the attached portion is pink and translucent. |
External Causes
Irritants such as nail polish, nail wraps, nail hardeners, artificial nails, the use of fingernails as a tool, and habitual finger sucking. The toenails are subject to athletic injuries and from wearing tight shoes
Fungal infections such as chronic paronychia and onychomycosis (see below)
Certain drugs can act as phototoxic agents to induce fingernail onycholysis. Such drugs include diuretics, sulfa drugs, tetracycline, minocycline, and doxycycline. Hemorrhagic onycholysis may result from taxanes, a chemotherapeutic agent used in the treatment of various cancers
Internal Causes
Psoriasis is the most common inflammatory cause of onycholysis. Often there is evidence of psoriasis elsewhere on the body or there may be other psoriatic nail findings such as pitting, subungual hyperkeratosis, and “oil spots” (see Psoriatic Nail Dystrophy below)
Inflammatory skin diseases of the nail matrix (root), such as eczematous dermatitis or lichen planus
Thyroid disease, pregnancy, and anemia have been reported as potential associations
Management
The goal of management is to keep the newly growing nail attached by:
Keeping nails dry and cut closely; proper trimming along the nail’s contour on a regular basis can protect the nails from injury
Using nail polish sparingly
Avoiding unnecessary filing and manipulation
Nails should be kept short. A long nail acts as a lever and magnifies traumatic damage
Green Nail Syndrome
Green nail syndrome is an asymptomatic, blue-green discoloration under the nail that is a consequence of a Pseudomonas infection of an onycholytic nail. The “dead space” under the elevated nail serves as an excellent breeding ground for microbes. The green, greenish-yellow, or green-black nail color is due to the bacteria’s production of pyocyanin pigment (Fig. 15-4).
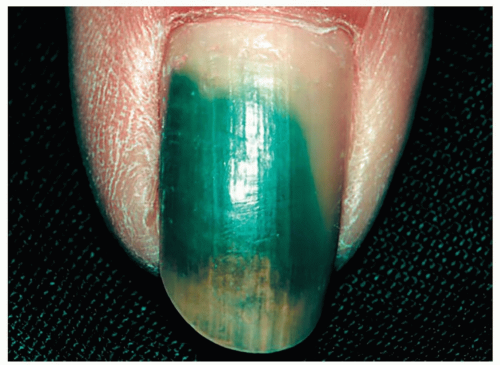 Figure 15-4 Green nail syndrome. The “dead space” under the nail often harbors Pseudomonas species. The green color is virtually pathognomonic for Pseudomonas. |
Management
Soaking the affected nail twice daily in a mixture of either one-part chlorine bleach (Clorox) and three-parts water or equal parts acetic acid (vinegar) or isopropyl alcohol and water generally eliminates the discoloration
If possible, avoid or minimize the underlying causes (see onycholysis discussed above)
Onychomycosis
Onychomycosis (tinea unguium) refers to an infection of the fingernails or toenails caused by various fungi, yeasts, and molds. The term tinea unguium refers specifically to nail infections caused by dermatophytes. Many patients who have toenail onychomycosis will also have chronic tinea pedis. Onychomycosis is uncommon in children, but its prevalence increases dramatically with advancing age, with rates as high as 30% in those who are over 70 years old. The major causes of onychomycosis are:
Dermatophytes: Epidermophyton floccosum, Trichophyton rubrum, and Trichophyton mentagrophytes, yeasts, mainly Candida albicans and molds.
Clinical Variants
Distal subungual onychomycosis accounts for more than 90% of all cases and is characterized by the following.
Fingernails
Nail thickening and subungual hyperkeratosis (Fig. 15-5) (scale buildup under the nail)
Nail discoloration (yellow, yellow-green, white, or brown)
Nail dystrophy
Onycholysis (nail plate elevation from the nail bed)
Frequently associated with chronic palmoplantar tinea (i.e., “two feet, one hand” variant of tinea) (see Fig. 14-19)
Toenails
May affect one or more toenails, most often the great toenail (Fig. 15-6) or the fifth toenail
Generally asymptomatic, aside from footwear causing occasional physical discomfort and the psychosocial liability of unsightly nails, onychomycosis can be a source of seeding for bacterial infection leading to cellulitis, especially in diabetics
Toenail onychomycosis is cured less quickly and effectively than in the fingernails
In superficial white onychomycosis, the fungus is located in the upper level of the nail plate (Fig. 15-7).
In proximal white onychomycosis, HIV infection should be suspected (Fig. 15-8).
 Figure 15-6 Onychomycosis (tinea unguium). The great toenail is dystrophic with pronounced subungual hyperkeratosis. |
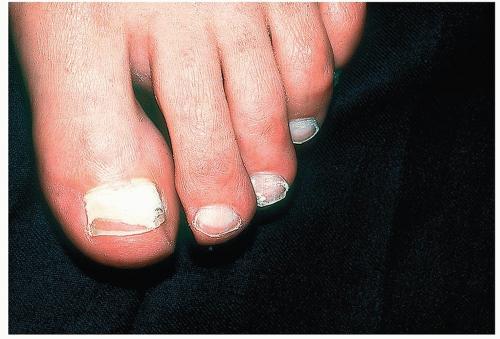 Figure 15-7 Superficial white onychomycosis. A KOH specimen was easily obtained from the surface of this lesion. |
Diagnosis
A positive KOH examination or growth of dermatophyte, yeast, or mold on culture
Management
See Table 15-1 for list of systemic antifungal medications
Oral Terbinafine (Lamisil) Tablets
Oral terbinafine (Lamisil) tablets are now the first-line treatment for onychomycosis, replacing griseofulvin, which is less effective and is associated with a high recurrence rate
Terbinafine is fungicidal, especially against dermatophytes; however, long-term cure rates are probably no greater than 40% to 50%
Side effects are infrequent. However, baseline liver function tests are performed, and the tests should be repeated in 4 to 6 weeks
Terbinafine has a reservoir effect. Because it persists in the nail for up to 4 to 5 months, there is no need to wait until the nail appears clinically normal as there is continued clearing even after cessation of therapy.
Dosage
Adults: 250 mg/day for 6 weeks for fingernails; 250 mg/day for 12 weeks for toenails
Alternatively, pulse dosing with 250 mg/day for 1 week monthly for 4 months
Children (weight 20 to 40 kg): 125 mg/day; weight more than 40 kg: 250 mg/day for 6 to 12 weeks
Oral Itraconazole (Sporanox) Capsules
This is a broad-spectrum fungistatic agent
The primary drawback to the use of this drug is the risk for significant drug interactions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree