Myelomeningocele: Postnatal Repair
Gregory G. Heuer
Jesse A. Taylor
DEFINITION
Myelomeningocele (MMC) is a congenital malformation of the spinal cord in the family of neural tube defects and spina bifida.1
MMC develops from a failure of neurulation of the spinal cord during the fourth week of gestation. The exposure of the spinal cord results in dysfunction of neural tissue as a result of the malformation itself and damage to the exposed neural tissue.
MMCs occur in roughly 1 in 1000 live births and lead to significant morbidity including bowel and bladder dysfunction, gait disturbances, and even paralysis. Importantly, lack of sensation caudal to the MMC may result in significant decubital wound issues.
ANATOMY
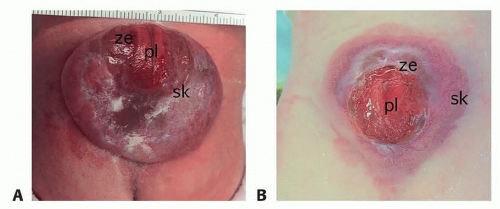
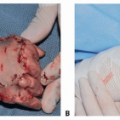
The MMC results from failure of neurulation, which results in an “open book” of distinct elements that are normally closed over the spinal cord2 (FIG 1).
The placode, the exposed flat spinal cord tissue, is present in the center, with nerve roots running ventrally and exiting through the spine foramen. Atrophic nerve roots can often be seen exiting the placode and running to the skin and soft tissue. These are nonfunctional elements.
The zona epitheliosa surrounds the placode and contains cerebrospinal fluid (CSF). This is part of the sac or “bubble” seen on imaging studies.
The dura of the meninges is open and reflected and covers the fascia and muscle.
The skin is located laterally to the lesion. Some of this tissue is extremely thin and atrophic. The quality of the skin needs to be taken into account, as it impacts surgical closure.
Elements of the posterior vertebral body—the spinous process and lamina—are absent, and the spinal column is open dorsally. The open spinal column can be seen laterally as the bifida bone elements.
In some cases, a sac is not present, and the placode is flat and in the spinal elements. This condition is known as myeloschisis and is managed in the same way as a MMC.
PATHOGENESIS
During neurulation, normally the neural tube undergoes an ordered process of formation and closure. During this process, the neural folds meet and fuse, followed by closure of the layers around the spinal cord—including the dura, bone, muscle, and skin.1
MMC results from a failure of the neural tube to close at the caudal end, resulting in the exposure of the spinal cord—the placode—to the external environment.
Most cases are idiopathic, though risk factors include genetic susceptibility and environmental risks such as toxins or medication exposure.
Risk factors include genetic susceptibility and environmental risks such as toxins or medication exposure. In most cases, there is not an identifiable cause and is thus idiopathic.
In some populations, the use of high-dose folic acid supplementation prior to conception can reduce the risk of neural tube defects, as folate is a known cofactor in many of the folding processes involved in neurulation.
NATURAL HISTORY
MMC leads to irreversible loss of nerve function at the level of the exposed spinal cord.
This loss of function occurs from3:
Abnormal development of the spinal cord
Direct damage to the exposed spinal cord from trauma and toxic injury
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with MMC are typically identified prior to birth.
Ultrasound examination is performed for three reasons:
To define the MMC defect and its spinal level
To look at associated abnormalities of the central nervous system
To analyze the fetus for other structural abnormalities
Patients with known MMC lesions are typically delivered via cesarean section.
Newborn MMC patients are cared for in a systematic fashion (http://www.chop.edu/clinical-pathway/myelomeningocele-myeloschisis-neonatal-clinical-pathway).
General neonatal care must be the first priority, assuring that the newborn is stable and healthy and avoiding the temptation to focus solely on the MMC lesion.
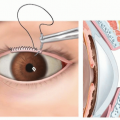
In the presence of a MMC, the patient is generally positioned prone to avoid undue pressure on the exposed spinal elements. A sterile gauze is placed on the MMC lesion, and this is kept moist with a constant drip of sterile saline from a bag suspended above the patient.
The patient is placed on antibiotics (ampicillin and amoxicillin) as prophylaxis against bacterial seeding of the spinal elements.
Consults are obtained including the physical therapy, neurosurgery, orthopedics, plastic surgery, urology, and spina bifida team.
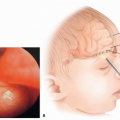
An ultrasound of the head is obtained to establish a baseline of the ventricular system.
A physical exam is performed on the infant.
The infant is examined for signs of hydrocephalus such as a full fontanelle, large head circumference, or splayed sutures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree