Lips and Perioral Area
OVERVIEW
The term cheilitis refers to inflammatory lesions involving the mucous membranes of the lips. Many disorders of mucous membranes (see also Oral Cavity), both inflammatory, as well as neoplastic, are difficult to distinguish from one another when confined to the mucosa since they tend to look alike clinically.
Because the lower lip is in a more sun-exposed position than the upper lip, sun-induced cheilitis (actinic cheilitis) and neoplasms such as actinic keratoses and squamous cell carcinomas are more often seen here. The upper lip, its vermillion border, and perioral area are common locations for herpes simplex virus infections.
Benign lesions such as venous lake, labial melanotic macule, and pyogenic granuloma are also seen on the lips. Many of the conditions that occur in the perioral region represent an extension of disorders noted elsewhere on the face such as acne, folliculitis, atopic dermatitis, and contact dermatitis.
CHILDREN AND ADULTS
Atopic Cheilitis
Atopic cheilitis is a variant of atopic dermatitis. As in atopic dermatitis elsewhere on the body, atopic cheilitis occurs in association with a personal or family history of atopy. It is exacerbated by frequent wet/dry cycles, lip licking and lip biting, and exposure to allergens or irritants, lip cosmetics, as well as some systemic medications, such as isotretinoin (commonly known as Accutane), that cause dryness.
Distinguishing Features
Inflammation of the lips is characterized by redness, fissuring, and scaling
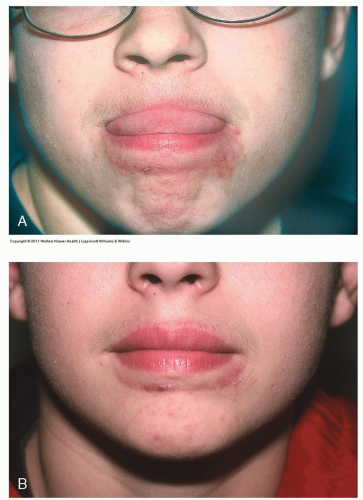
The scaling and erythema of eczema may spread on and beyond the vermillion border, which becomes less distinct and blurred (Fig. 8-1)
Worsened by lip licking, mouth breathing
Frequently occurs in patients with eczema elsewhere on the body
History of easy chapping in wintertime
May be exacerbated by irritant or sensitizing chemical agents, ultraviolet irradiation, and by cold and windy weather
Diagnosis
Clinical
Management
Low-potency (class 6) ointment-based topical steroids
Moisturization with petroleum jelly at bedtime
ChapStick or other fragrance-free lip balms
Avoidance of identified irritants
If indicated, psychological consultation for obsessive/compulsive lip licking
 Figure 8-1 Atopic cheilitis. Note the scaling, crusting, lichenification, as well as blurring of the vermillion border in this child who has atopic dermatitis. |
Irritant and Allergic Cheilitis
Both irritant and allergic cheilitis may be caused by agents such as lipsticks, lip balms, sunscreen in lip cosmetics, toothpaste ingredients, dental prostheses, nail varnish, cosmetics, and nickel in the mouthpieces of musical instruments. Other potential allergens include fragrance, balsam of Peru, lanolin, and flavorings (i.e., strawberry and vanilla).
Distinguishing Features
Inflammation of the lips with redness, fissuring, and scaling (Fig. 8-2)
History of easy chapping
May also have coexistent eczema elsewhere on the body
Diagnosis
Diagnostic clues have to be obtained from a careful history which includes a review of oral rinses, toothpastes, and cleansers
Lip licking (Fig. 8-3, A and B)
Patch testing if necessary
Management
Avoid identified irritant/allergen contactants
Low-potency (class 6) ointment-based topical steroids
Moisturize lips with petroleum jelly at bedtime
Angular Cheilitis (Perlèche)
Angular cheilitis (AC), also known as perlèche (from the French “to lick”), is an inflammatory condition that occurs at the corners of the mouth. It is most often seen in elderly people who have diabetes.
AC appears in seniors, when atrophy of the perioral muscles of facial expression causes a pocketing at the corners of the mouth, resulting in an overhang of the upper lip over the lower lip, resulting in a moist deep furrow at the angles of the mouth. Other contributing factors, such as poor-fitting dentures, malocclusion, lack of teeth, and bone resorption, may lead to drooling or vertical shortening of the face, thus accentuating the melolabial crease.
Coexistent atopic cheilitis, lip licking in children, mouth breathing, and the presence of orthodontic devices are also risk factors. Vitamin and iron deficiency are often blamed, but rarely proven as a cause of AC.
Distinguishing Features
Redness, maceration, scaling, fissuring, and crusting occur at the corners (angles) of the mouth
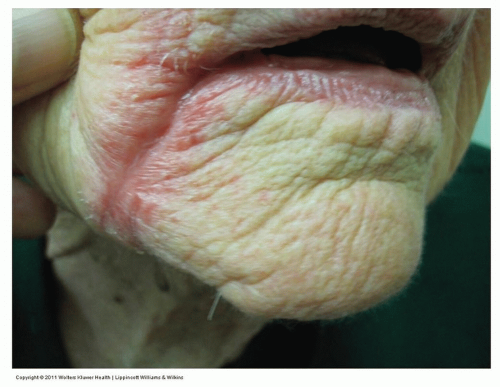
Figure 8-4 Angular cheilitis (perlèche).
An 88-year-old diabetic woman with redness and maceration at the angle of her lips. KOH preparation revealed Candida pseudohyphae.
The macerated “pockets” may also serve as a nidus for the secondary overgrowth of Candida albicans (Fig. 8-4) or Staphylococcus aureus
Diagnosis
Clinical
Fungal examination, bacterial cultures as needed
Management
Petrolatum or other ointments are used to protect and moisturize the area
A low- or mid-potency topical steroid such as desonide (DesOwen) 0.05% or Elocon (mometasone furoate) ointment 0.1% or over-the-counter hydrocortisone 1% ointment often helps resolve the inflammation
Mupirocin (Bactroban) ointment should be applied for suspected bacterial infection
For candidiasis, a topical anticandidal such as ketoconazole, clotrimazole, or nystatin in combination with a class 6 topical hydrocortisone ointment is helpful
Topical immunomodulators such as topical calcineurin inhibitors such as tacrolimus 0.1% ointment (Protopic) or pimecrolimus (Elidel) 1% cream also may be effective
If necessary, a dental referral is suggested to correct potential causative factors
Perioral Dermatitis (Periorificial Dermatitis)
Perioral dermatitis also known as periorificial dermatitis is a rosacea-like eruption seen primarily in young women between the ages of 15 and 40 and in young children (see also Eyelids and Periorbital Area and Nose and Paranasal Area). As with rosacea, the etiology of perioral dermatitis is unknown.
Tooth whiteners and fluoridated toothpaste have occasionally been implicated, but without any consistent evidence. It is accepted, however, that the frequent application of high-potency, and less commonly, low-potency topical corticosteroids, or inhaled corticosteroids can cause a topical steroid-induced rosacea/periorificial dermatitis-like eruption in some individuals.
Distinguishing Features
Manifests in tiny 1- to 3-mm erythematous papules or pustules without comedones or telangiectasias
Characteristically, lesions are confined symmetrically around the mouth with a clear zone of about 5 mm between the vermilion border of the lips and the affected skin (Fig. 8-5)
Occasionally, there is superimposed scaling
Usually, this condition does not recur after successful treatment
Diagnosis
Clinical
Inquire about topical steroid applications
Diagnosis is confirmed by response to treatment with a systemic antibiotic (most often a tetracycline derivative)
Management
Gentle facial cleansing
Discontinue application of topical steroids to face or wean to weaker strengths
Responds readily to oral doxycycline or minocycline in adults and erythromycin or azithromycin in children
Antibiotic is tapered when the inflammation has improved, usually after 2 to 3 weeks. Azithromycin, clarithromycin, or amoxicillin is used as a second-line alternative when a tetracycline fails or is not tolerated
Topical antibiotics such as erythromycin, clindamycin, or metronidazole are less effective
Nonsteroidal azelaic acid (Finacea) or topical calcineurin inhibitors such as tacrolimus 0.1% ointment (Protopic) or pimecrolimus 1% cream (Elidel) may also be effective
When perioral dermatitis is caused by the application of a potent topical steroid, its continued application seems to improve the condition; however, discontinuance may result in a flare and worsening before it starts to improve. Thus, the patient is inclined to continue using the topical steroid “one step forward, two steps backward” in a vicious cycle.
Herpes Simplex Virus Infection
Herpes simplex virus infection of the lips and perioral area is caused most often by herpes simplex virus-1 (HSV-1). HSV-1 is mainly associated with oral-facial infections (“cold sores” or “fever blisters”); less often, HSV-2 may be the cause. Neonatal herpes simplex occurs when newborns are exposed to HSV-2 via the birth canal of an actively infected mother who has an HSV-1 or, more commonly, HSV-2 infection, during a vaginal delivery.
Primary HSV infections (see also Oral Cavity) are acquired in infancy and early childhood (Fig. 8-6) and most are subclinical; however, when HSV is symptomatic, the most common clinical presentation in infants and children occurs in the oropharyngeal epithelium where it can be quite severe (see Fig. 9-5).
The virus is highly contagious and is spread by direct contact with the skin or mucous membranes. It invades and replicates in neurons as well as in epidermal and dermal cells. Virions travel from the initial site of infection on the skin or mucosa to the sensory dorsal root ganglion where the virus becomes incorporated into the genetic material of the cells and remains latent until it becomes reactivated.
 Figure 8-6 Primary herpes simplex virus. Perioral vesicles and bullae on an erythematous base are seen in this 1-year-old child. (Courtesy of Robert I. Rudolph, MD.) |
 Figure 8-7 Recurrent herpes simplex virus. Grouped umbilicated vesicles on the vermilion border of the lower lip. |
Recurrent HSV Infections (Herpes Labialis)
Reactivation occurs from various triggers such as sunlight exposure, menses, immunosuppression, fever, common colds, dental surgery, and possibly stress. In many cases, no reason for the eruption is evident. Herpes labialis, also referred to as a “cold sores” and “fever blisters,” tends to be very painful. Recurrent HSV infection often occurs on the vermilion border
Distinguishing Features
Patients commonly experience a localized prodrome of itching, pain, or numbness (“tingling”) 1 to 2 days before the outbreak
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree