Lichen Planus
Elyse M. Love
Evan Rieder
BACKGROUND
PRESENTATION
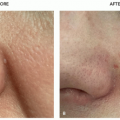
Classically, cutaneous LP presents with purple (violaceous), pruritic, polygonal papules or plaques, colloquially referred to as the “4 Ps.”
Cutaneous LP most commonly presents between 30 and 60 years of age. LP is uncommon in children, but pediatric cases have been documented.4 Cutaneous lesions tend to spontaneously remit in 1 to 2 years with no treatment; however, oral lesions may persist for 5 years, and erosive lesions may not self-resolve.
DIAGNOSIS
Clinical Diagnosis
When observed closely, papules and plaques are composed of numerous 1- to 2-mm papules that coalesce into larger flat-topped papules and plaques. Fine white lines (“Wickam striae”) can be appreciated on lesion surfaces. Koebnerization of previous sites of trauma may occur.
Distribution is typically limited, with the most common affected areas including the volar wrists, ankles, flexural forearms, dorsal hands, neck, genitalia, shins, and presacral area.
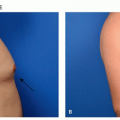
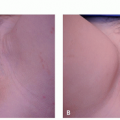
Generalized as well as blashkoid, zosteriform, and inverse lichen planus has been documented. A clinical example of inverse lichen planus is shown in Figure 14.4.1. The oral mucosa is affected in over half of cases with cutaneous findings. Oral mucosa can also be the only site affected.
Classic lesions of LP may be diagnosed via clinical examination alone. Physical examination should include a total body skin examination, including inspection of oral and genital mucosa. Dermoscopic examination may increase visibility of Wickam striae. Given LP’s association with hepatitis C virus (HCV) and the presence of a drug-induced variant, a detailed drug history and HCV risk factors should be obtained. Patients with oral involvement should undergo review of systems to assess for possible esophageal involvement.
Routine screening for HCV in patients with LP is controversial, and there is no expert consensus at this time.
Histopathology
Atypical lesions benefit from histopathologic correlation with a shave or punch biopsy that captures epidermis to mid-dermis. Histopathology of classic and atypical lichen planus shows hyperkeratosis, irregular acanthosis with “sawtooth” elongation of the rete ridges, and a bandlike lymphocytic infiltrate at the dermal-epidermal junctional.
Direct immunofluorescence is not needed in the majority of cases, but it is beneficial for bullous lesions where autoimmune bullous diseases are included in the differential.
Subtypes
Clinical variants include:
Actinic: erythematous, eczematous, and hyperpigmented patches and plaques with a hypopigmented perimeter on sun-exposed skin
Annular: annular plaques with erythematous centers and hypopigmented edge on penile glans or shaft
Atrophic: atrophic plaques that eventuate from hypertrophic or annular variants, seen more commonly after treatment with topical corticosteroids
Bullous: vesicles or bullae present in preexisting LP lesions
Erosive: painful ulcers affecting the oral or genital mucosa
Hypertrophic: hyperkeratotic, thick, pruritic red-brown to gray-purple plaques often on the anterior lower legs
Inverse: LP lesions distributed in axilla, neck, or inframammary regions
Lichen planopilaris: patches of hair loss, scaling, redness with or without papules surrounding hair follicles, and pain, burning, tenderness, or itching on the scalp
Lichen planus pigmentosus: small black macules that enlarge and coalesce into hyperpigmented plaques in darker skin types on sun-exposed skin.
Linear: papules are distributed along lines of Blaschko
Vulvovaginal-gingival: a severe variant of erosive LP affecting the gums and vagina in women
Nail: thinning, longitudinal ridging, and distal splitting of the nail plate
Drug-induced: see section “Lichenoid Drug Eruption”
Although the variants are clinically distinct from classic LP, all variants share similar histology to the classic form.
Differential Diagnosis
Lichenoid Drug Eruption
No definitive clinical or histopathologic features distinguish idiopathic LP from drug-induced LP. However, thorough history and clinicopathologic correlation can help to distinguish the two. A thorough drug history
should be obtained in patients with new-onset LP. Potential identification of the culprit drug is complicated by the delayed onset of the drug reaction and delayed resolution after cessation of the drug. The duration between initiation of drug and rash onset can vary from weeks to months, with an average time frame of 12 months. Resolution of lesions also may take weeks to months after cessation of the culprit drug. Many drugs have been implicated; however, confirmation on reexposure has not been documented for many of the documented causative agents. The most common culprits include angiotensin-converting enzyme inhibitors, thiazide diuretics, antimalarials, quinacrine, and gold.
should be obtained in patients with new-onset LP. Potential identification of the culprit drug is complicated by the delayed onset of the drug reaction and delayed resolution after cessation of the drug. The duration between initiation of drug and rash onset can vary from weeks to months, with an average time frame of 12 months. Resolution of lesions also may take weeks to months after cessation of the culprit drug. Many drugs have been implicated; however, confirmation on reexposure has not been documented for many of the documented causative agents. The most common culprits include angiotensin-converting enzyme inhibitors, thiazide diuretics, antimalarials, quinacrine, and gold.
Lichenoid id Reaction From a Contact Dermatitis
In children, the most common allergen to cause a lichenoid id reaction is nickel. Oral lesions after recent dental work should raise the suspicion for contact allergy to amalgam, copper, or gold.
Other Lichenoid Dermatoses
Lichen planus is the hallmark disorder of the lichenoid dermatoses, which include lichen nitidus, lichen striatus, lichen sclerosus, annular lichenoid eruption, and lichenoid graft-versus-host disease.
Overlap Syndromes
Lichen planus may be associated with lupus erythematous in lichen planus-lupus erythematous overlap syndrome and bullous pemphigoid in lichen planus pemphigoides syndrome. Clinicopathologic correlation can distinguish the entities.
Lichen Planus Pigmentosa and Erythema Dyschromicum Perstans
Lichen planus pigmentosa and erythema dyschromicum perstans have subtle examination findings, are difficult to distinguish clinically, and require histologic confirmation.
Other
Pityriasis rosea
Psoriasis
Secondary syphilis