Laboratory Procedures and Tests
Christopher J. Kligora MD
Kenneth R. Watson DO
In addition to the usual laboratory procedures used in the workup of medical patients, certain special tests are of importance in the field of dermatology. These include skin tests, fungus examinations, biopsies, and immunologic diagnosis. For special problems, additional testing methods are suggested in the sections on the various diseases.
Skin Tests
There are three types of skin tests:
Intracutaneous
Scratch
Patch
The intracutaneous tests and the scratch tests can have two types of reactions: either an immediate wheal reaction or a delayed reaction. The immediate wheal reaction develops to a maximum in 5 to 20 minutes and is elicited in testing for the cause of urticaria, atopic dermatitis, and inhalant allergies. This is a type I or anaphylactoid type of immunity. The immediate wheal reaction test is seldom used for determining the cause of skin diseases.
The delayed reaction to intracutaneous skin testing is exemplified best by the tuberculin skin test. Tuberculin is available in two forms—as the purified protein derivative test and as a tuberculin tine test. The purified protein derivative test is performed by using tablets that come in two strengths and by injecting a solution of either one intracutaneously. If there is no reaction after the test with the first strength, then the second strength may be employed.
The tuberculin tine test (Mantoux) is a simple and rapid procedure using OTK. Nine prongs, or tines, covered with OTK are pressed into the skin. If at the end of 48 or 72 hours there is more than 2 mm of induration at the site of any prong insertion, the test is positive.
Patch tests are used commonly in dermatology and offer a simple and accurate method of determining whether a patient is allergic to any of the testing agents. There are two different reactions to this type of test: a primary irritant reaction and an allergic reaction. The primary irritant reaction occurs in most of the population if they are exposed to agents (in appropriate concentrations) that have skindestroying properties. Examples of these agents include soaps, cleaning fluids, bleaches, “corn” removers, and counterirritants. The allergic reaction indicates that the patient is more sensitive than normal to the agent being tested. This test reaction is idiosyncratic and not necessarily related to concentration or dose. It also shows that the patient has had a previous exposure to that agent or a cross-sensitizing agent. This is a type IV or delayed type of immunity. It is often very helpful in cases of contact dermatitis.
The technique of the patch test is simple, but the interpretation of the test is not. For example, consider a patient presenting with dermatitis on top of the feet. It is possible that shoe leather or some chemical used in the manufacture of the leather is causing the reaction. The procedure for a patch test is to cut out a half-inch square piece of the material from the inside of the shoe, moisten the material with distilled water, place it on the skin surface, and cover it with an adhesive band or some patch-test dressing. The patch test is left on for 48 hours. When the patch test is removed, the patient is considered to have a positive patch test if there is any redness, papules, or vesiculation under the site of the testing agent. Delayed reactions to allergens can occur, and, ideally, a final reading should be made after 96 hours (4 days), that is, 2 days after the patch is removed.
The patch test can be used to make or confirm a diagnosis of poison ivy dermatitis, ragweed dermatitis, or contact dermatitis caused by medications, cosmetics, or industrial chemicals. Fisher (1995) and Adams (1990) compiled lists of chemicals, concentrations, and vehicles to be used for eliciting the allergic type of patch test reaction. Most tests can be performed very simply, however, as in the case of the shoe leather dermatitis. One precaution is that the patch must not be allowed to become wet in the 48-hour period. A patch test kit, T.R.U.E. Test (Glaxo), includes ready-to-apply self-adhesive allergen tapes. There are other more extensive patch test trays available.
A method of testing for food allergy is to use the Rowe elimination diet. The procedure is to limit the diet to the following basic foods, which are known to be hypoallergenic: lamb, lemon, grapefruit, pears, lettuce, spinach, carrots, sweet potatoes, tapioca, rice and rice bread, corn sugar, maple syrup, sesame oil, gelatin, and salt. The patient is to remain on this basic diet for 5 to 7 days. At the end of that time, one new food can be added every 2 days. The following foods can be added early: beef, white potatoes, green beans, milk (along with butter and American cheese), and white bread with puffed wheat. If there is a flare-up of the dermatitis, which should occur within 2 to 8 hours after ingestion of an offending food,
the new food should be discontinued for the present. More new foods are added until the normal diet, minus the allergenic foods, is regained.
the new food should be discontinued for the present. More new foods are added until the normal diet, minus the allergenic foods, is regained.
Keeping a “diet diary” of all foods, medicines, oral hygiene items, or anything injected or inhaled can sometimes be a retrospective way of identifying an allergen. The skin reaction usually occurs less than 8 hours after ingestion.
Fungus Examinations
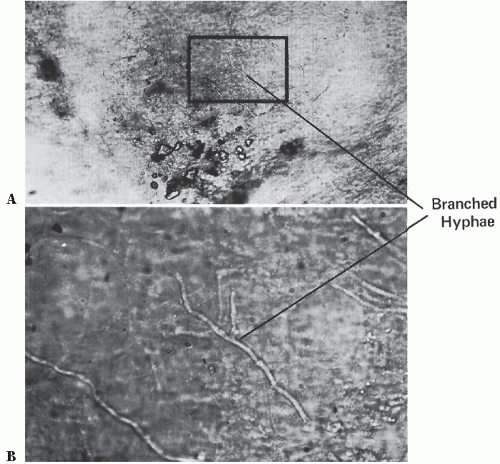
The KOH preparation is a simple office laboratory procedure for the detection of fungal organisms present in skin and nails. It is performed by scraping the diseased skin and examining the material with the microscope. The skin scrapings are obtained by abrading a scaly diseased area with a scalpel. If a blister is present, the underside of the blister is examined. The material is deposited on a glass slide and then covered with 20% aqueous potassium hydroxide solution and a coverslip. The preparation can be gently heated or allowed to stand at room temperature for 15 to 60 minutes. The addition of dimethyl sulfoxide to the KOH preparation eliminates the need to heat the specimen. A diagnostically helpful pale violet stain can be imparted to the fungi if the 20% KOH solution is mixed with an equal amount of Parker Super Quik permanent blue-black ink. Other staining solutions are available. The slide is then examined microscopically for fungal organisms (Fig. 2-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree