Kaposi Sarcoma
Elyse M. Love
Evan Rieder
BACKGROUND
Kaposi sarcoma (KS) is a multifocal cutaneous disease of multiple variants that affects endothelial cells.
PRESENTATION
Patients present with slow-growing, pink to red to violaceous macules on the lower extremities. Patients may have a history of immunosuppression, AIDS, or Mediterranean or African heritage.
DIAGNOSIS
Clinical Diagnosis
The lesions of KS are notable for their violaceous hue and well demarcated, jagged borders. Four clinical variants of KS exist: classic KS, KS associated with iatrogenic immunosuppression, AIDS-related epidemic KS, and African endemic KS. All 4 variants are thought to occur secondarily to activation of human herpesvirus (HHV)-8. The histology of all 4 lesions is identical.
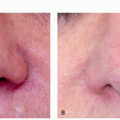
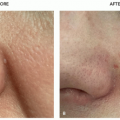
Classic KS and KS associated with iatrogenic immunosuppression are clinically similar. Patients present with slow-growing, pink to red to violaceous macules on the lower extremities. Over time, the lesions coalesce to patches and evolve to papules and plaques (Figure 14.7.1). Lesions may involute as new lesions form, resulting in lesions at different stages. Patients may have asymptomatic involvement of the mouth and gastrointestinal tract. For KS associated with iatrogenic immunosuppression, lesions may resolve after the immune system is restored. Chronically immunosuppressed patients are at risk of fatal internal organ involvement.
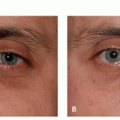
AIDS-related epidemic KS is an opportunistic infection and occurs in patients with CD4+ T cell counts <500 cells per cubic millimeter; its presentation is varied. Lesions range in color and morphology from pink to erythematous to violaceous to purple-black and patches, plaques, or tumors with the potential to ulcerate, respectively. Lesions may be individual or multifocal. The trunk and midface are the most common sites of involvement, although any body surface can be affected. Lesions may cause physical restrictions and cosmetic
disfigurement. The gastrointestinal tract, lymph nodes, and lungs can be affected. Lung involvement portends a poor prognosis.
disfigurement. The gastrointestinal tract, lymph nodes, and lungs can be affected. Lung involvement portends a poor prognosis.
African endemic KS is further divided into 4 subcategories: nodular, florid, infiltrate, and lymphadenopathic. Like classic KS, the nodular variant is indolent, whereas the florid, infiltrative, and lymphadenopathic variants are more aggressive. The lymphadenopathic variant most commonly presents in the lymph nodes of children and is fatal.
Suspicious lesions should be biopsied to confirm diagnosis. Human immunodeficiency virus (HIV) testing should be considered in patients whose HIV status is unknown.
Histopathology
The histology of KS varies based on the stage of the lesion. In early, patch stage KS, there is an irregular proliferation of delicate vessels in the superficial dermis, with a mild lymphoplasmacytic infiltrate. As the lesion progresses to the more palpable plaque stage, the proliferation of angulated and interconnecting vessels infiltrates to the deep dermis and upper panniculus, with a more conspicuous proliferation of spindled endothelial cells. In the late nodular stage, the proliferation fills the dermis, and characteristic slitlike spaces are seen between the fascicles of spindled endothelial cells. Immunohistochemical staining against HHV-8 is highly specific for KS.1
Subtypes
Classic KS
KS associated with iatrogenic immunosuppression
AIDS-related epidemic KS
African endemic KS
Differential Diagnosis
The differential for early KS includes all other benign and malignant vascular neoplasms, venous hypertension, cutaneous metastases, leukemia cutis, polyarteritis nodosa, and erythema elevatum diutinum.
The differential for later-stage KS includes pseudo-KS (acroangiodermatitis of Mali) and Stewart-Bluefarb syndrome.
PATHOGENESIS
All clinical variants are all understood to be secondary to viral activation of HHV-8. It remains unclear whether KS represents a neoplasm or hyperplasia of endothelial cells. It is also unclear if affected endothelial cells are vascular, lymphatic, or a mixture of the 2 types.1
TREATMENT
With the exception of the aggressive African endemic variants, KS follows an indolent, chronic, and relapsing clinical course. Treatment is aimed at improving quality of life through improved cosmesis and symptom relief. In certain patient populations, interval clinical monitoring without active treatment may be an appropriate course of action. Algorithm 14.7.1 outlines the treatment of KS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree