Inflammatory and Other Benign Disorders of Skin Appendages
VIIA Pathology Involving Hair Follicles
Inflammatory processes may present as alopecia, or as follicular localization of inflammatory rashes. Acne and related conditions present as dilatation of follicles which are filled with keratin (1,2).
Scant Inflammation
Lymphocytes Predominant
With Prominent Eosinophils
Neutrophils Prominent
Plasma Cells Prominent
Fibrosing and Suppurative Follicular Disorders
Table VII.1. Non-scarring Alopecia (Normal Follicular Density) | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
VIIA1 Scant Inflammation
There is follicular alteration with a sparse infiltrate of cells, mainly lymphocytes. Androgenic alopecia and trichotillomania are important examples. These conditions may result in non-scarring alopecia in which the number of follicles is normal at least in the early stages of hair loss (see Table VII.1).
Androgenetic Alopecia
Clinical Summary
The expression of androgenetic alopecia (AGA) frequently shows a familial and probably genetic inheritance pattern. Hair shafts become progressively finer and shorter, with true alopecia occurring only as a later event. This involutional process slowly evolves to
become so severe that the scalp skin becomes exposed to a greater or lesser extent. This process can also occur in women, although much less frequently and with lesser severity so that significant balding is quite unusual.
become so severe that the scalp skin becomes exposed to a greater or lesser extent. This process can also occur in women, although much less frequently and with lesser severity so that significant balding is quite unusual.
Histopathology
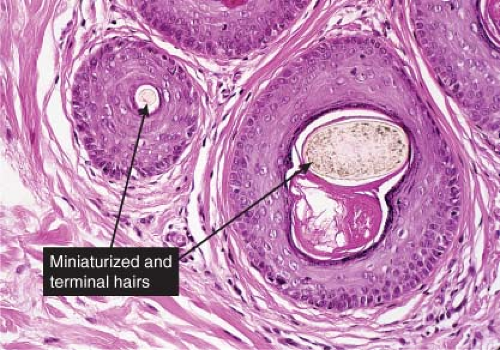
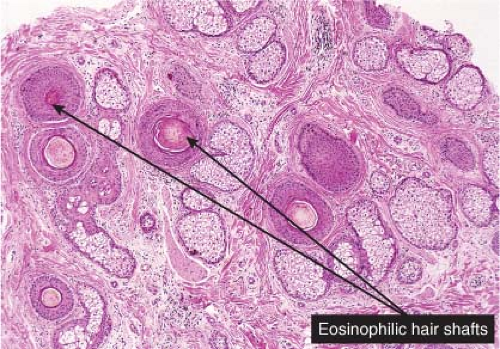
Evaluation of this condition can be achieved best from transverse sectioning of punch biopsy material (3,4). Diminution of follicular size, most effectively measured by assessment of mean hair shaft diameter, can be obtained with relative simplicity using an optical micrometer. Since this approach allows assessment of all follicles in the specimen, direct counting of anagen, telogen, and catagen follicles can be undertaken and the percentages of each obtained (5). Reduction of follicular size appears to be randomized, so that, initially, normal-size follicles coexist with an increased number of smaller ones, whereas, ultimately, follicular reduction becomes more persistent and obvious. Associated with this reduction in follicular size,
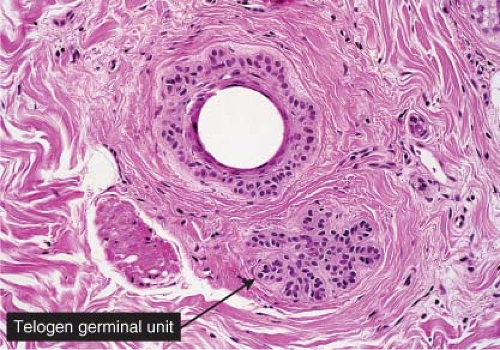
there is a progressive increase in the percentage of telogen follicles, both of normal club pattern and with increasing severity, diminutive or persistent telogen epithelial remnants (telogen germinal units). These structures appear to represent epithelial remnants of telogen follicles that no longer respond to the stimulus to return to anagen growth. Ultimately, there may be a reduction in the density of follicles. Peri-infundibular fibroplasia ultimately leading to focal follicular scarring may be the explanation for the reduced follicular density. The diminution of follicles leads to a substantial increase in the number of empty follicular sheaths in the deeper dermis and subcutaneous tissue.
there is a progressive increase in the percentage of telogen follicles, both of normal club pattern and with increasing severity, diminutive or persistent telogen epithelial remnants (telogen germinal units). These structures appear to represent epithelial remnants of telogen follicles that no longer respond to the stimulus to return to anagen growth. Ultimately, there may be a reduction in the density of follicles. Peri-infundibular fibroplasia ultimately leading to focal follicular scarring may be the explanation for the reduced follicular density. The diminution of follicles leads to a substantial increase in the number of empty follicular sheaths in the deeper dermis and subcutaneous tissue.
Trichotillomania
Clinical Summary
Compulsive avulsion of hair shafts leads to zones of thin, ragged, broken stubble on the affected scalp. If the damage is done in localized fashion it can occasionally mimic alopecia areata. Follicular breakage and loss may occasionally be associated with evidence of damage to the scalp by erosions or crusts.
Histopathology
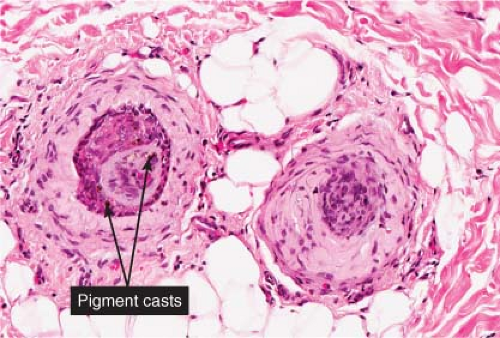
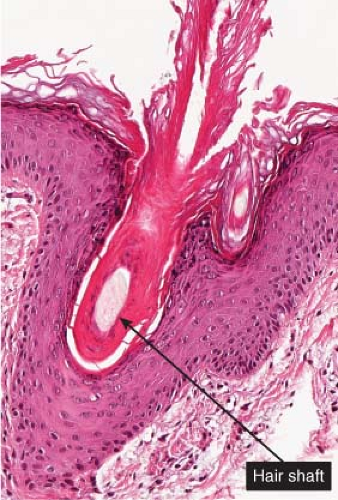
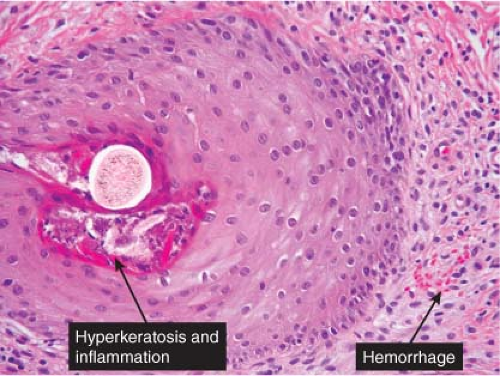
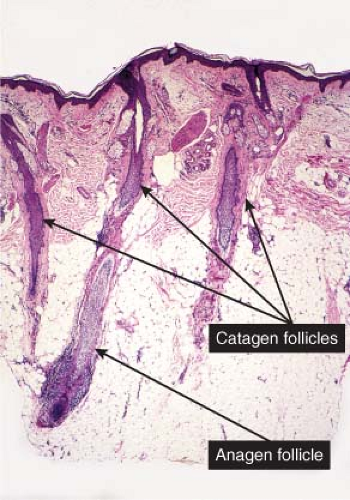
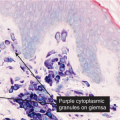
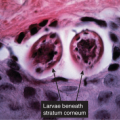
The most important findings in biopsy specimens are an increase in catagen hairs (up to 75%), pigmentary defects and casts, evidence of traumatized hair bulbs, and trichomalacia (a complete but distorted, fully developed terminal hair in its bulb) (6). Occasionally, follicles may be identified still in anagen but empty because of hair shaft avulsion. Follicles can show considerable distortion of the bulbar epithelium and sometimes conspicuous hemorrhage. Hair shaft avulsion may deposit melanin pigment in the hair papilla and peribulbar connective tissue. Pigment casts are also frequently identified in the isthmus or infundibulum. Trichomalacia, if present, is specific for trichotillomania. Longitudinal splitting of a hair shaft with blood sandwiched in between has been called the “hamburger sign” (7). These various injuries to the bulbar portions of follicles are not accompanied by significant inflammatory infiltrates. Trichotillomania is not associated with miniaturization of follicles or with deep perifollicular infiltrates, features that usually serve to differentiate it from alopecia areata. Histologic findings in early traction alopecia are said to be identical with those of trichotillomania, but fewer follicles are involved, the changes are less dramatic, and vellus hairs are preserved.
Telogen Effluvium
Clinical Summary
Telogen effluvium represents the increased or excessive shedding of hair in the telogen phase of the growth cycle. This condition has several precipitating causes or associated conditions, including chemotherapy and debilitating diseases of various kinds, which may cause alopecia by eliciting changes in the length of the anagen period of growth, and in the active process of release of hair shafts in telogen. Plucked or shed telogen hairs have a club-like appearance at the bottom of the shaft, and are therefore often known as “club hairs.”
Histopathology
Telogen effluvium does not show significant dermal inflammatory infiltrates, nor should there be evidence of diminution of follicular and hair shaft size, unless telogen effluvium occurs in patients with established androgenetic or another form of involutional alopecia (8). Proportions of normal telogen follicles in excess of 15% to 25% are considered to be abnormal and
suggest the likely presence of telogen. If a biopsy is obtained in the very early stages of recovery, early anagen regeneration follicles will also be present, while if recovery is substantial, the appearances may be entirely normal (9).
suggest the likely presence of telogen. If a biopsy is obtained in the very early stages of recovery, early anagen regeneration follicles will also be present, while if recovery is substantial, the appearances may be entirely normal (9).
 Clin. Fig. VIIA1.b. Trichotillomania. “Plucking” of hairs by a middle aged female with a delusional disorder resulted in well-demarcated patches of alopecia in a diffuse distribution. |
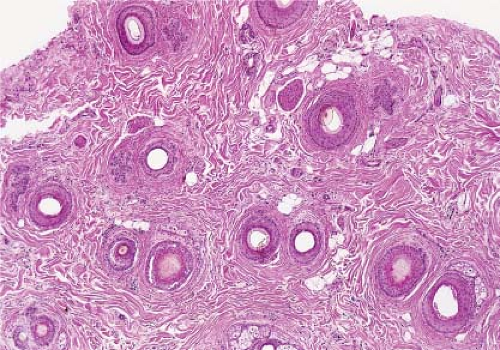
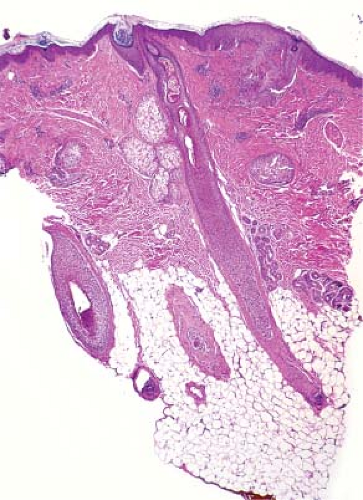 Fig. VIIA1.f. Trichotillomania, low power. At scanning magnification there is a normal number of hair follicles per cross-section. There is a mild, predominantly superficial inflammatory infiltrate. |
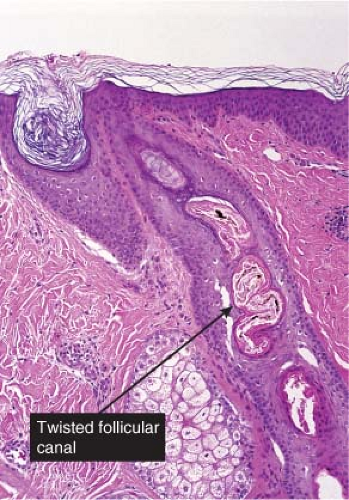 Fig. VIIA1.g. Trichotillomania, medium power. One frequently sees distortion of the hair follicle, as manifested here by the twisted contour of the follicular canal. |
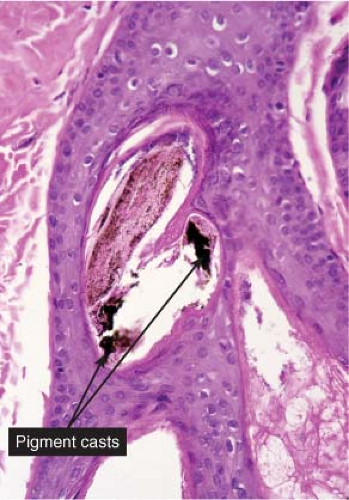 Fig. VIIA1.h. Trichotillomania, high power. A characteristic finding in trichotillomania is the presence of pigment casts (clumps of pigment) which are present in the follicular canal. (continues) |
Keratosis Pilaris
Keratosis pilaris (KP) is a common inherited disorder of follicular hyperkeratosis, which is characterized by small, folliculocentric keratotic papules that may have surrounding erythema, most commonly affecting the extensor aspects of the upper arms, upper legs, and buttocks. The small papules impart a stippled appearance to the skin resembling gooseflesh. Associated/related conditions may include keratosis pilaris atrophicans, erythromelanosis follicularis faciei et colli, and ichthyosis vulgaris (10).
Scurvy
See Figs. VIIA1.o–q.
Conditions to consider in the differential diagnosis:
Follicular maturation disorders
androgenetic alopecia
telogen effluvium
trichotillomania
scurvy
vitamin A deficiency (phrynoderma)
Follicular keratinization disorders
keratosis pilaris
lichen spinulosus
trichorrhexis invaginata (Netherton’s syndrome)
trichostasis spinulosa
acne vulgaris
Favre–Racouchot syndrome (nodular elastosis with cysts and comedones)
nevus comedonicus
Bazex syndrome (follicular atrophoderma)
VIIA2 Lymphocytes Predominant
There is follicular alteration with an inflammatory infiltrate mainly of lymphocytes. Conditions associated with inflammation may in many instances result in scarring alopecia in which hairs are lost and replaced by fibrosis (see Table VII.2).
Alopecia Areata
Clinical Summary
Alopecia areata is characterized by complete or nearly complete absence of hair in one or more circumscribed areas of the scalp (11). Inflammatory change is not clinically obvious, and the follicular openings are preserved. Complete scalp involvement (alopecia totalis), or complete or nearly complete loss of the entire body hair (alopecia universalis) can occur. Involvement of the eyebrows and eyelashes and a pitted defect in the nail plates are additional features of this condition. Most patients undergo spontaneous resolution, but a few patients have permanent hair loss. In the areas of active hair shedding, a short, fractured hair shaft may be identified’the characteristic “exclamation point” hair.
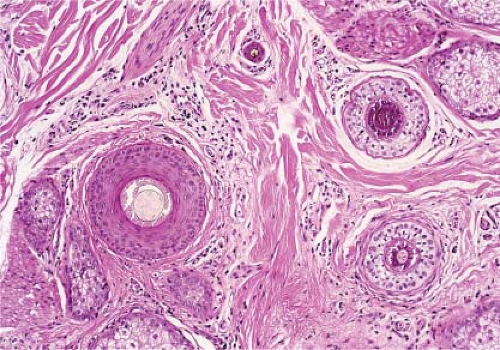
Histopathology
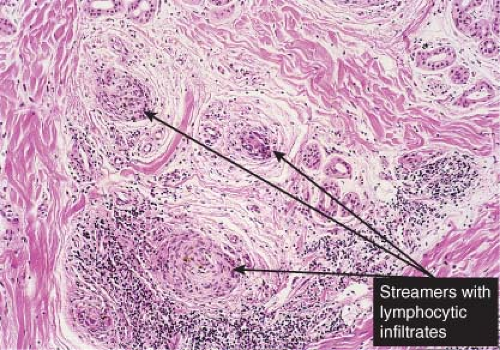
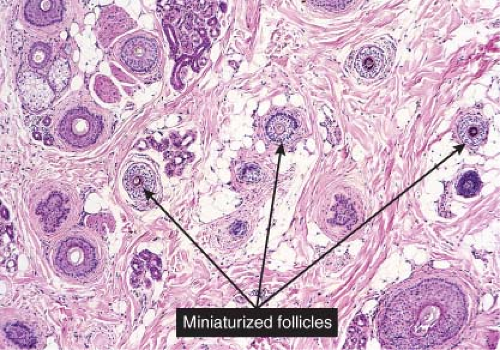
The critical diagnostic pathologic sign is lymphocytic infiltrates in the peribulbar area of anagen follicles, or follicles in early catagen (12). The lymphocytic infiltrates are present around the receding epithelial remnant but also in the area of the collapsing follicular sheaths. While still in anagen, lymphocytes may be seen sparsely infiltrating the matrix epithelium. Follicular structures diminish in size rapidly and become miniaturized, and as a result are identified more superficially in the dermis (13). The diminutive follicles are observed predominantly in early or late catagen. During the recovery phase, diminutive anagen follicles may be quite numerous, many showing some peribulbar lymphocytic infiltrates. In long-standing cases, the inflammatory infiltrates appear to diminish. In severe alopecia universalis and totalis of long duration (a decade or more), functional follicular structures may be diminished in number and some scarring of the follicular sheaths may be identified. Dilated follicular infundibula, which on horizontal sectioning bears resemblance to Swiss cheese, is another helpful clue in alopecia areata (14). When biopsy specimens are sectioned transversely early in the disease, it can be demonstrated that the number of follicles is not diminished but that follicles enter a persistent phase of telogen (telogen germinal units) and that there is a diminution of normal club telogen follicles.
Lichen Planopilaris
Clinical Summary
Lichen planopilaris is lichen planus with follicular involvement in some or all of the lesions. This type of lichen planus predominantly affects the scalp. Initially, there may be only follicular papules or perifollicular erythema; however, with progressive hair loss irregularly shaped atrophic patches of scarring alopecia develop on the scalp (15). The axillae and the pubic region may also be affected and the alopecia in these areas may be cicatricial. Hyperkeratotic follicular papules may also be seen on glabrous skin. The association of scarring alopecia of hair-bearing areas and hyperkeratotic follicular papules on glabrous skin is known as Graham Little syndrome. Lichen planopilaris may also coexist with typical lichen planus lesions on skin, mucous membranes, or nails. Linear lichen planopilaris of the face resolving with scarring has also been described.
Frontal fibrosing alopecia is a variant of lichen planopilaris that occurs in a band over the frontal scalp, typically in postmenopausal females (16). Recent research has shown that the characteristic histologic findings also involve vellus hair follicles on the face, clinically presenting as small papules (17).
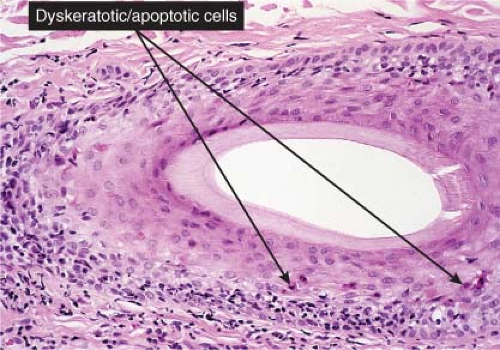
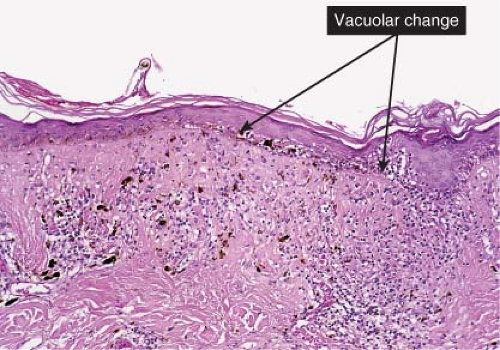
Histopathology
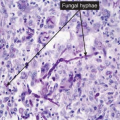
Most early lesions of lichen planopilaris show a focally dense, band-like perifollicular lymphocytic infiltrate at the level of the infundibulum and the isthmus where the hair “bulge” is located (18). Initially, the inferior segment of the hair follicle is spared. Vacuolar changes of the basal layer of the outer root sheath and necrotic keratinocytes are often seen. In addition, orthokeratosis and follicular plugging are observed. A few biopsies exhibit simultaneous involvement of the interfollicular epidermis and the hair follicles. In more developed lesions perifollicular fibrosis and epithelial atrophy at the level of the infundibulum and isthmus are characteristic findings. Damage to the hair bulge, the site where stem cells of the hair follicle reside, results in permanent scarring alopecia. Advanced cases show alopecia with vertically oriented fibrotic tracts containing clumps of degenerated elastic fibers replacing the destroyed hair follicles. This end-stage scarring alopecia in which no visible hair follicles remain has been designated by some as pseudopelade of Brocq.
Table VII.2. Scarring Alopecia (Decreased Follicular Density | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 Clin. Fig. VIIA2.a. Alopecia Areata. Well circumscribed patch of alopecia with “exclamation” (!) hairs (tapering at proximal end) at the periphery typically respond to intralesional corticosteroids. |
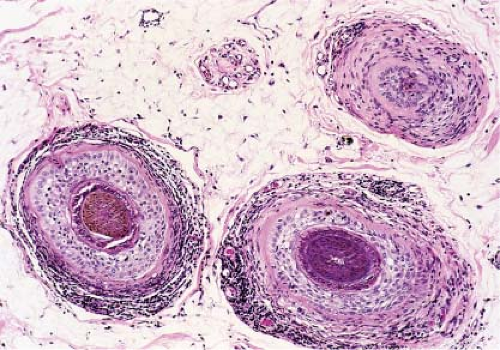
 Fig. VIIA2.b. Alopecia areata, high power, vertical section. A dense lymphocytic infiltrate (“swarm of bees”) hugs the bulb of the terminal anagen follicle seen in the previous figure. |
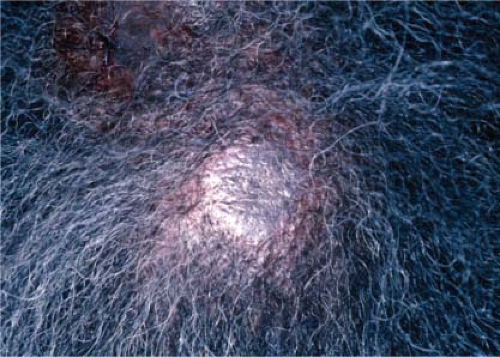
Central Centrifugal Cicatricial Alopecia
Clinical Summary
Since many forms of scarring alopecia share clinical and histologic features that make them difficult to distinguish with certainty, a unifying concept of central centrifugal cicatricial alopecia (CCCA) was proposed to reflect the overlap (19). CCCA encompasses several types of permanent hair loss which have in common the following features: alopecia centered on the crown or vertex of the scalp; progressive chronic disease with eventual “burnout”; fairly symmetrical expansion with the most active areas at the periphery; and clinical and microscopic evidence of inflammation in these active sites (20).
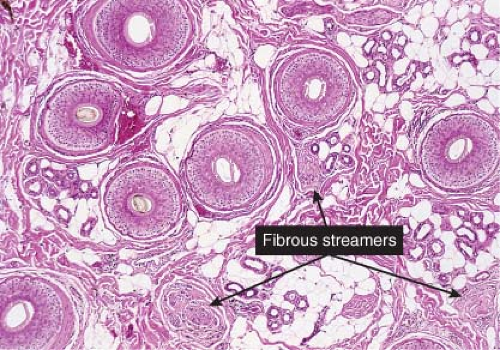
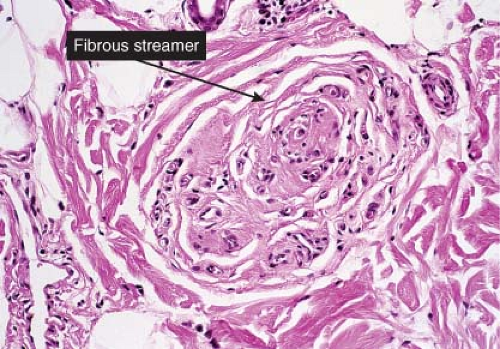
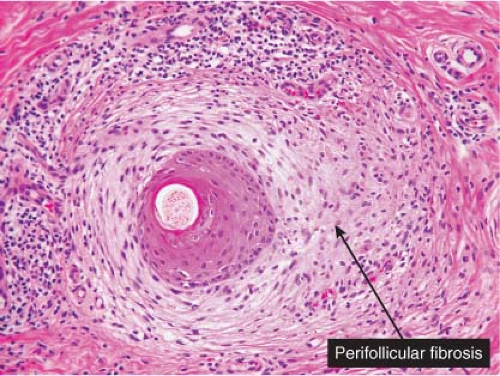
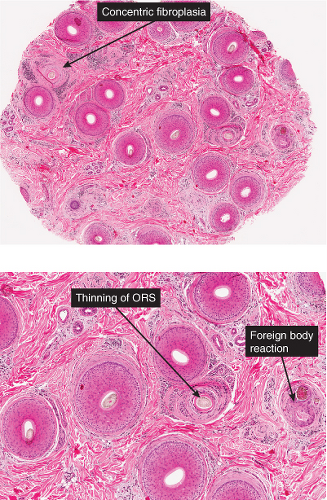
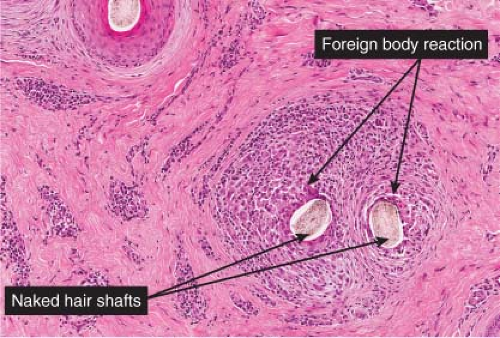
Histopathology
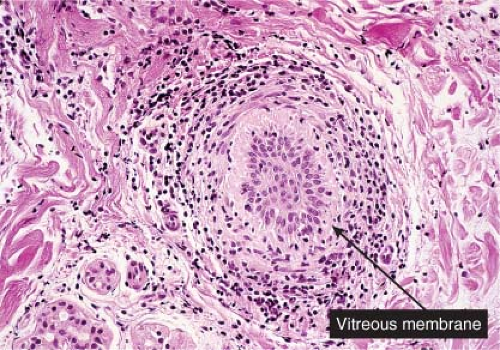
CCCA displays all of the following histologic features: eccentric thinning of the outer root sheath epithelium, most prominent at the level of the isthmus and lower infundibulum, associated with close
apposition of the hair shaft and follicular contents to the dermis; concentric lamellar fibroplasia (“onion skin” fibrosis); and chronic inflammation composed of lymphocytes and plasma cells surrounding the zone of fibroplasia (21). Eventually, the hair shaft migrates into the dermis, inciting granulomatous inflammation and additional epithelial destruction. Finally, the follicle is replaced by a vertical band of connective tissue, resulting in a “follicular scar.” Singly, these histologic features may be found in other types of scarring alopecia.
apposition of the hair shaft and follicular contents to the dermis; concentric lamellar fibroplasia (“onion skin” fibrosis); and chronic inflammation composed of lymphocytes and plasma cells surrounding the zone of fibroplasia (21). Eventually, the hair shaft migrates into the dermis, inciting granulomatous inflammation and additional epithelial destruction. Finally, the follicle is replaced by a vertical band of connective tissue, resulting in a “follicular scar.” Singly, these histologic features may be found in other types of scarring alopecia.
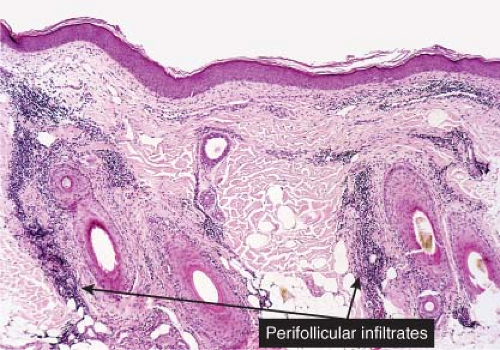
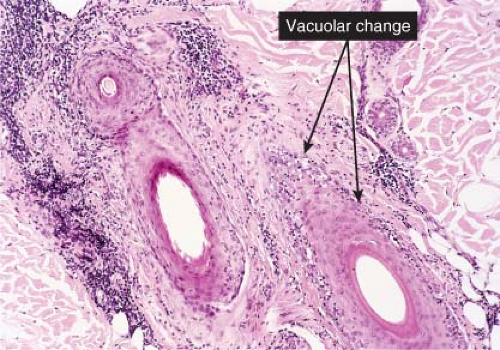 Fig. VIIA2.i. Lichen planopilaris, medium power, vertical section. The lymphocytic infiltrate is associated with vacuolar alteration of the outer layers of the follicular epithelium. |
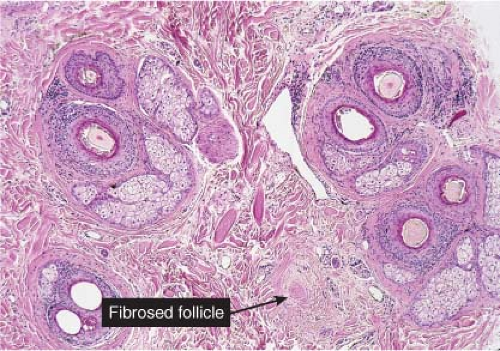 Fig. VIIA2.j. Lichen planopilaris, low power, horizontal section. Follicular loss (i.e., scarring) is best identified on horizontal sections. A perifollicular lymphoid infiltrate is also apparent. |
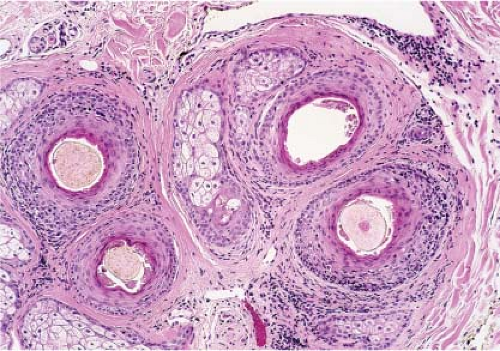 Fig. VIIA2.k. Lichen planopilaris, medium power, horizontal section. At the level of the isthmus, vacuolar change, perifollicular fibrosis and inflammation are most prominent. |
CCCA may also show one of three histologic patterns of disease: follicular degeneration syndrome, pseudopelade pattern (a “modern” use of the term, not pseudopelade of Brocq), and folliculitis decalvans (22). Features may be
present that allow sub-classification into one of these patterns. For instance, African American patients with CCCA who display characteristics of the follicular degeneration syndrome pattern tend to show premature desquamation of the inner root sheath (23). A characteristic histologic feature of the folliculitis decalvans pattern is folliculocentric neutrophilic inflammation, typically seen if a pustule from the expanding margin is biopsied.
present that allow sub-classification into one of these patterns. For instance, African American patients with CCCA who display characteristics of the follicular degeneration syndrome pattern tend to show premature desquamation of the inner root sheath (23). A characteristic histologic feature of the folliculitis decalvans pattern is folliculocentric neutrophilic inflammation, typically seen if a pustule from the expanding margin is biopsied.
 Clin. Fig. VIIA2.b. Central centrifugal cicatricial alopecia. This condition occurs most commonly in African-Americans and affects the crown and vertex scalp. Hair loss is permanent. |
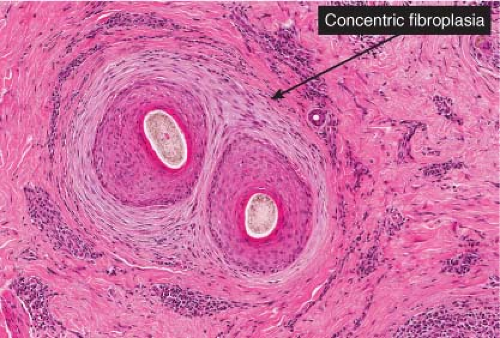 Fig. VIIA2.o. Central centrifugal cicatricial alopecia, transverse section. The affected follicles show early perifollicular fibrosis with some mononuclear inflammation. (continues) |
Alopecia Mucinosa
Alopecia mucinosa can be seen in childhood but is more common in adults. It may occur in three settings: a primary idiopathic form, a form associated with malignancy, and a form secondary to inflammatory conditions. The histologic
hallmark is follicular mucinosis, the accumulation of mucin in the follicular epithelium (24).
hallmark is follicular mucinosis, the accumulation of mucin in the follicular epithelium (24).
 Clin. Fig. VIIA2.c. Discoid lupus erythematosus. The inflammation in this hyperpigmented plaque with follicular plugging led to permanent hair loss. |
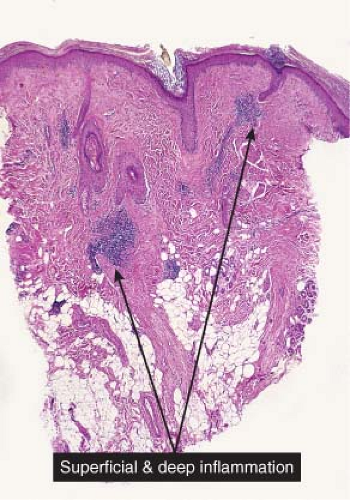 Fig. VIIA2.q. Discoid lupus erythematosus of the scalp, low power. A superficial and deep often quite prominent perivascular and perifollicular inflammatory infiltrate is seen at low magnification. |
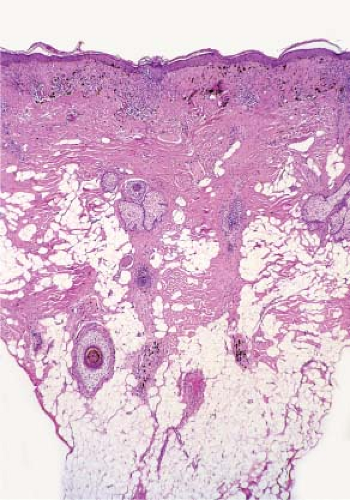 Fig. VIIA2.r. Discoid lupus erythematosus, low power. In some examples, as here, the infiltrate can be quite sparse. The number of hair follicles is diminished at scanning magnification. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree