Chapter 8 Indications for Primary Flexor Tendon Repair
Outline
Injuries in the flexor tendons can occur in the digits, palm, wrist, or distal and mid-forearm. Tendon repairs in the digital sheath area are most technically demanding and controversial. The advent of primary flexor tendon repairs within the synovial sheath region should be credited to pioneers of nearly half a century ago, including Verdan1 and Kleinert and colleagues.2,3 Prior to that time, over most of the previous half century, primary tendon repair was not advocated and surgeons were accustomed to removing the tendons entirely and grafting in new tendon.4,5 The reports of Verdan and of Kleinert and his colleagues on primary flexor tendon repairs followed by early mobilization established that the lacerated digital flexor tendon can be treated by direct end-to-end repairs when wound conditions are favorable.1–3
Anatomical Divisions
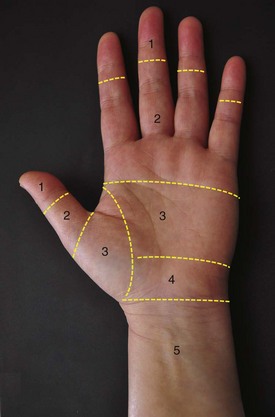
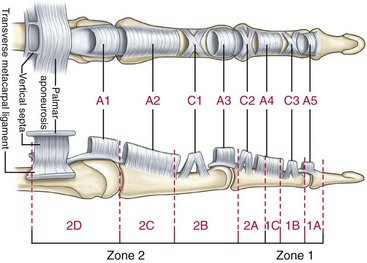
By virtue of their anatomical features, the flexor tendons in the hand and forearm are divided into five zones, which delineates the fundamental nomenclature for flexor tendon anatomy and surgical repairs.1,3,6 In the 1990s, the most complex areas—the flexor tendons within the digital sheath—were subdivided by Moiemen and Elliot7 and by Tang.8 The zoning is described in Box 8-1, and its relation to the locations of pulleys is shown in Figures 8-1 and 8-2.
Box 8-1 Nomenclature for Flexor Tendon Anatomy in the Hand and Forearm
Zones of Finger Flexor Tendons (Verdan)
| 1 | From the insertion of the FDS tendon the terminal insertion of the FDP tendon |
| 2 | From the proximal reflection of the digital synovial sheath to the FDS insertion |
| 3 | From the transverse carpal ligament to the digital synovial sheath |
| 4 | Area covered by the transverse carpal ligament |
| 5 | Proximal to the transverse carpal liagment |
Zones of Thumb FPL Tendon
| 1 | Distal to the IP joint |
| 2 | From the IP joint to the A1 pulley |
| 3 | The area of the thenar eminence |
Zone 1 in Fingers (Moiemen and Elliot)
| 1A | The very distal FDP tendon (usually <1 cm) |
| 1B | From zone 1A to distal margin of the A4 pulley |
| 1C | The FDP tendon within the A4 pulley |
Zone 2 in Fingers (Tang)
| 2A | The area of the FDS tendon insertion |
| 2B | From the proximal margin of the FDS insertion to the distal margin of the A2 pulley |
| 2C | The area covered by the A2 pulley |
| 2D | From the proximal margin of the A2 pulley to the proximal reflection of digital sheath |
Etiologies and Evaluation of Tendon Injuries
During examination, any changes in resting position of the fingers should be closely observed (Figure 8-3). In assessment of function of the FDP and FDS tendons, patients are asked to actively flex the fingers. Inability to actively flex the finger proximal interphalangeal (PIP) or distal interphalangeal (DIP) joints using the specific tests shown in Figures 8-4 and 8-5, when passive motion is complete, indicates that the FDP or FDS tendon (or both) is completely severed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree