Hypospadias Repair
Christopher D. Morrison
Earl Y. Cheng
DEFINITION
Hypospadias is defined as a ventrally located meatus proximal to its expected orthotopic location.
Hypospadias is often associated with chordee, an abnormal ventral curvature of the penis.
ANATOMY
The hypospadiac meatus can be located anywhere along the course of the urethra:
Posterior/proximal: perineal, scrotal, penoscrotal
Middle: along the shaft of the penis
Distal/anterior: subcoronal, glandular
In general, a more proximal hypospadiac meatus is associated with a more significant degree of chordee.
The glans can vary in size, and the urethral plate can range from grooved to completely flat.
In most cases, the prepuce does not extend ventrally, resulting in a noncircumferential dorsal hooded foreskin.
The skin overlying the ventral aspect of the urethra can be dysplastic or insufficient, leading to ventral tethering of the penis.
The corpus spongiosum diverges laterally or is completely atretic, which can result in a urethra that is only covered by a very thin layer of ventral skin.
PATHOGENESIS
Hypospadias results from the incomplete development of the penis and urethra between 8 and 14 weeks gestation.
Tubularization of the urethra is thought to be androgen mediated, and disruption of this process results in a hypospadiac meatus.3
Both genetic and environmental factors have been associated with hypospadias.4
Hypospadias is heritable and can be associated with several syndromes (less than 10% of cases).
Over 20 genes have been implicated in the pathogenesis of hypospadias.
Environmental factors such as maternal medication/drug use, maternal age, maternal obesity, and placental insufficiency have been associated with hypospadias and may account for the rising prevalence of hypospadias.
PATIENT HISTORY AND PHYSICAL FINDINGS
Hypospadias is typically recognized at the time of birth during newborn examination.
Newborn circumcision (if desired) is contraindicated in the setting of hypospadias because the foreskin may be needed for surgical repair of the hypospadias.
History
A complete prenatal and family history should be performed to identify possible contributing factors.
If possible, ask the parents about the direction and strength of the patient’s urinary stream, as well as the curvature of the penis with erections. A downward deflected urinary stream or significant curvature of the penis may affect the patient’s urinary and sexual function later in life.
Exam
Penile exam:
Location and appearance of the meatus
Quality and depth of urethral plate
Size and configuration of the glans
Degree of chordee
Integrity of the ventral skin
Amount of dorsal hooded foreskin available
A careful scrotal and inguinal exam should be performed to look for other abnormalities such as cryptorchidism, hydrocele, or hernia.5
If a patient also has undescended testicles (unilateral or bilateral), it is important to consider the possibility of a disorder of sex development (DSD).
If undiagnosed, a DSD condition such as congenital adrenal hyperplasia (CAH) can be life threatening.
These patients should undergo an endocrine workup and karyotype.
Approximately 20% to 30% of patients with hypospadias and cryptorchidism will have a karyotype abnormality.3
The most common DSD seen in patients with hypospadias and cryptorchidism is mixed gonadal dysgenesis.
IMAGING
Proximal hypospadias can be associated with renal anomalies. However, routine imaging is not performed in most cases of hypospadias. If the patient has a severe proximal hypospadias, one could consider obtaining a renal ultrasound.
NONOPERATIVE MANAGEMENT
For patients with distal/anterior hypospadias in which the urinary stream is relatively straight and there is no significant chordee, surgical correction is generally considered optional and is usually performed more for appearance and psychosocial reasons rather than for correction of a functional need.
There is controversy among some urologists as to whether correction of distal hypospadias confers long-term benefits for patients.
A 1995 study of 500 men found great variability in the meatal location. Thirteen percent of these men had anterior hypospadias with no functional compromise, and two-thirds of these patients were unaware of their hypospadiac condition.5
In contrast, a 2014 study examined the self-reported outcomes for patients who had uncorrected hypospadias and found that these patients were more likely to have worse voiding symptoms, more penile curvature making sexual intercourse difficult, and worse satisfaction with the appearance of their penis.6
SURGICAL MANAGEMENT
Multiple different surgical techniques have been described for distal hypospadias, including the MAGPI and the Mathieu repair. However, the tubularized incised plate (TIP) urethroplasty, as described by Snodgrass, is the technique that is now most commonly performed by hypospadias surgeons. It is suitable for patients with a sufficiently healthy and wide (greater than 7 mm) urethral plate and less than 30-degree chordee.
Midshaft hypospadias is often approached similarly to distal hypospadias; however, it tends to be associated with more significant chordee.
If there is less than 30-degree chordee and the urethral plate is sufficiently healthy and wide, a TIP urethroplasty can be performed.
If there is less than 30-degree chordee but the urethral plate is too narrow, hypospadias repair can be performed using a transverse preputial island flap or an inner preputial inlay graft.
Proximal hypospadias repair presents a greater challenge for several reasons:
There is a longer length of urethra that must be tubularized.
The urethral plate may be narrow, fibrotic, or even nonexistent.
There tends to be a more significant degree of chordee.
Preoperative Planning
If diagnosed at the time of birth, most urologists will delay treatment until the child is 6 months of age to decrease potential anesthetic risks.
Ideally, the surgery should be performed prior to the child being old enough to remember the surgery.
Many advocate hypospadias repair between 6 and 12 months of life.7
Historically, hormonal stimulation with testosterone, dihydrotestosterone, or human chorionic gonadotropin was given preoperatively to increase penile length, glans circumference, and vascularity as this was thought to aid in surgical correction.
However, there is now concern that hormonal stimulation may affect normal wound healing and may lead to an increased risk of postoperative complications.8
Nevertheless, hormone stimulation is still felt to be beneficial in more severe cases of hypospadias.
Positioning
After the induction of general anesthesia, if possible, a caudal anesthetic block is recommended for perioperative pain control.
The patient is positioned supine for the surgery.
Approach
The operative approach varies based on the following:
Location of the hypospadiac meatus
Severity of chordee
Characteristics (width, depth, and health) of urethral plate
Quality of penile shaft and dorsal hood skin
Surgeon preference/experience
The main components of a hypospadias repair consist of the following:
Evaluation and correction of chordee
Urethroplasty
Glanuloplasty
Skin coverage
Hypospadias repair is typically performed with the use of 2.5 times surgical loupes or with an operating microscope.
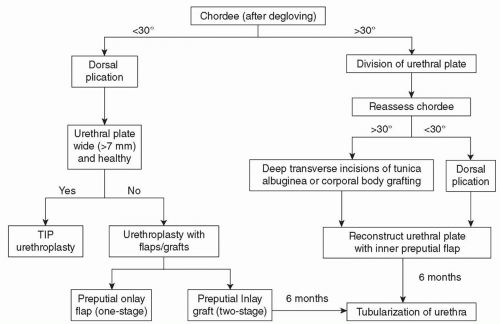
Hypospadias repair can be either a one- or two-staged repair. The decision to perform a one- or two-stage repair depends primarily on the degree of chordee and the health of the urethral plate.
If the chordee can be corrected with dorsal plication and the urethral plate is healthy and wide, a TIP urethroplasty should be performed.
If the chordee can be corrected with dorsal plication but the urethral plate is NOT healthy and wide, the surgeon can perform either a one-staged preputial onlay island flap urethroplasty or a two-staged inner preputial inlay graft with subsequent tubularization.
If division of the urethral plate is required for correction of chordee, this should be performed during the initial stage. The urethroplasty should be performed in a second stage at least 6 months later.
An algorithm for intraoperative decision-making during hypospadias repair is presented in FIG 1.
TECHNIQUES
▪ Tubularized Incised Plate Urethroplasty for Distal Hypospadias Repair
▪ Examination Under Anesthesia
Prior to beginning the surgery, examine the anatomy.
Visually inspect the meatus.
Calibrate the meatus with bougies and examine the ventral penile skin overlying the urethra.
If the urethra and overlying skin is too thin, it may be necessary to perform a cutback procedure to healthier tissue and perform a more proximal hypospadias repair.
Examine the urethral plate for width, depth, and overall health.
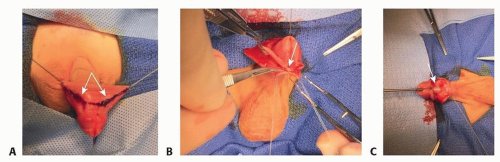
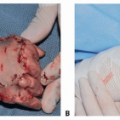
▪ Initial Approach (TECH FIG 1)
Place a 4-0 Ethibond suture longitudinally at the tip of the glans for retraction purposes.
Make a reverse chevron incision on the dorsum of the penis to preserve the mucosal collar flaps.
Working laterally to medially, carefully elevate the ventral skin off of the urethra. (Avoid incising into the urethra. If necessary, it is better to buttonhole the overlying skin than to incise into the native urethra.)
Deglove the penis down to the penopubic and penoscrotal junction.
Induce an artificial erection and evaluate degree of chordee by constricting the corpora cavernosa at the base of the penis with a tourniquet device (ie, rubber band, dental roll, and hemostat) and injecting saline through a small-gauge butterfly needle into the corpora cavernosa.
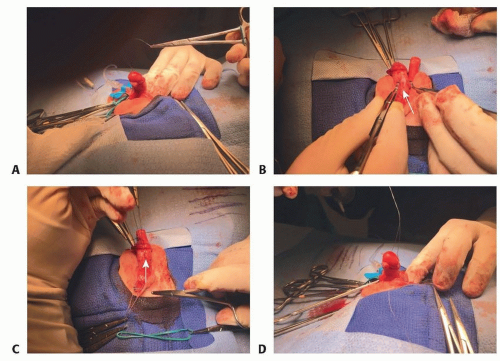
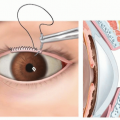
▪ Correction of Chordee With Dorsal Plication
In most cases of distal hypospadias, degloving of the penis alone will adequately straighten the penis.
In cases in which residual chordee remains that is less than 30 degrees, this can be corrected with dorsal plication (TECH FIG 2).
Dorsal plication will shorten the penis and should be avoided in patients with a small phallus.
Make an incision in Buck fascia at the 12 o’clock position over the dorsal vasculature.
Place a 3-0 or 4-0 Ethibond suture (Ethicon Inc., Somerville, NJ) parallel to the shaft, ensuring not to injure the neurovascular bundles laterally.
Imbricate Buck fascia over the plication suture using interrupted 6-0 PDS.
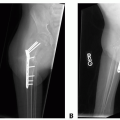
▪ TIP Urethroplasty (TECH FIG 3)
Elevate the spongiosum and create glans wings.
Often, the corpora spongiosum can be identified diverging lateral to the urethral plate.
If easily identified, elevate the divergent spongiosal tissue off the corporal bodies.
The corpus spongiosum can be used as an additional layer of closure over the urethral repair.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree