Introduction
Oncoplastic surgery for the management of breast cancer has been receiving worldwide attention and gaining widespread acceptance. Simply stated, oncoplastic surgery is defined as tumor excision with a wide margin of resection followed by immediate reconstruction of the partial mastectomy defect. Much of the enthusiasm for this procedure stems from safety data demonstrating oncologic feasibility and efficacy data demonstrating high patient satisfaction. These facts, as well as others, have resulted in improved outcomes for women with breast cancer.
Although modern methods of breast cancer management date back to the turn of the 20th century, the history of oncoplastic surgery is relatively new and has not been well chronicled. There have been several paradigm shifts that have occurred over the past century regarding the various treatment modalities. ( Table 1.1 ) To appreciate the current impact of oncoplastic surgery as it relates to the management of breast cancer, a brief history of modern breast cancer therapy is useful.
| Author | Year | Treatment |
|---|---|---|
| Halsted | 1890 | Radical mastectomy |
| Patey | 1948 | Modified radical mastectomy |
| McWhirter | 1948 | Simple mastectomy and radiotherapy |
| Toth | 1991 | Skin-sparing mastectomy |
| Noguchi | 1996 | Sentinel lymph node biopsy |
| VerHeyden | 1998 | Subcutaneous mastectomy (malignant disease) |
Prior to the era of William Stewart Halsted, the diagnosis of breast cancer was often associated with few options for management and poor patient survival. With the introduction of the radical mastectomy, the morbidity and mortality of breast cancer were markedly improved; however, the disfigurement following this operation was significant. The modified radical mastectomy (MRM), in which the pectoral major muscle was preserved and the axillary lymph node basin was dissected, maintained similar survival statistics with slightly less physical disfigurement. The simple mastectomy in conjunction with radiation therapy was introduced at the same time and continued to open the door for less aggressive surgical techniques. Further refinements in mastectomy techniques allowed for skin-sparing patterns that did not modify or alter local recurrence or survival patterns. With the introduction of sentinel lymph node biopsy for breast cancer, the need to perform an axillary dissection was significantly reduced and the simple mastectomy has become commonplace. Finally, the application for mastectomy with preservation of the nipple–areolar complex (NAC) for malignant disease was introduced and applied for women in select situations.
All of these mastectomy techniques resulted in significant disfigurement because the breast parenchyma was removed. In order to improve upon the physical disfigurement, breast reconstruction was introduced and popularized ( Table 1.2 ). Reconstructive options have included local tissues, prosthetic devices, musculocutaneous flaps, and perforator flaps. The evolution of these techniques has made a significant impact and ultimately led to the development of oncoplastic surgical techniques.
| Author | Year | Technique |
|---|---|---|
| Berson | 1944 | Derma-fat grafts |
| Longacre | 1953 | Local flaps |
| Snyderman | 1969 | Prosthetic devices |
| Arnold | 1976 | Omentum and prosthetics |
| Schneider | 1977 | Latissimus dorsi |
| Hartrampf | 1982 | TRAM flap |
| Argenta | 1984 | Tissue expansion |
| Grotting | 1989 | Free TRAM flap |
| Allen | 1994 | Perforator flaps |
Over the years, as our understanding of the pathophysiology of breast cancer has improved and our utilization of radiation therapy as an adjuvant mode of therapy was optimized, modifications to these original operations have evolved ( Table 1.3 ) It became accepted that for many breast cancers total mastectomy was not an absolute requirement; a partial mastectomy could be performed. With the introduction of breast conservation therapy (BCT), breast cancers could be excised with a 2–5 mm margin, the NAC could be preserved, and breast shape and contour would be maintained in the majority of women. Following the operative portion, radiation therapy is initiated. The outcomes following BCT have been generally favorable, with survival statistics that have remained essentially equal to that of MRM. However, local recurrence rates have been generally increased. Although the aesthetic outcomes following BCT have been good to excellent in the majority of women, some have required secondary procedures to improve the appearance and achieve symmetry. Thus, the shortcomings of BCT have included increased local recurrence and occasional breast distortion.
| Author | Year | Treatment |
|---|---|---|
| Crile | 1973 | Partial mastectomy |
| Montague | 1978 | Breast conservation therapy |
| Veronesi | 1994 | Segmental parenchymal excision |
| Gabka | 1997 | Oncoplastic surgery |
| Clough | 1998 | Reduction mastopexy lumpectomy |
| Amanti | 2002 | Periareolar parenchymal excision |
| Anderson | 2005 | Parallelogram excision patterns |
In an effort to reduce the incidence of local recurrence and maintain natural breast contour, the concept of oncoplastic surgery was introduced. Oncoplastic surgery differs from standard BCT in that the margin and volume of excision are typically greater than in lumpectomy or quadrantectomy. Excision margins typically range from 1 to 2 cm and resection volumes typically range from 180 to 220 cm 3 , although much greater margins and volumes are possible. The resultant deformity is reconstructed immediately using techniques related to volume replacement or volume displacement that include adjacent tissue rearrangement, reduction mammaplasty, or distant flaps. Contralateral procedures can be performed immediately at the time of partial breast reconstruction or on a delayed basis. Oncoplastic techniques have resulted in survival and local recurrence rates that are essentially equal to those of MRM.
The purpose of this introductory chapter is to review the history of these oncoplastic procedures. This chapter will emphasize some of the landmark studies and important conclusions. It will highlight some of the surgeons who have made significant contributions to the concept and practice of oncoplastic surgery. As oncoplastic surgery continues to gain acceptance and popularity, an optimal and systematic approach to management is becoming increasingly necessary. This chapter will touch upon some of the salient components and historic vignettes of oncoplastic surgery. The subsequent chapters will expand upon many of the principles, concepts, and techniques that are important in incorporating oncoplastic surgery successfully into one’s practice.
Toward safety and efficacy
The indications and patient selection criteria for oncoplastic surgery have not been without controversy, scrutiny, and criticism. There have been individuals who were of the opinion that the boundaries between oncologic management and aesthetic reconstruction have been blurred within the promotion of oncoplastic surgery. Contrary to this opinion is that by adhering to oncologic principles oncoplastic techniques can be safely performed in properly selected women. Regardless of one’s opinion, in order for oncoplastic surgery to be safely and effectively performed, patients should be properly selected and properly consented for these procedures. Surgeons should be aware of all aspects relating to the recovery and well-being of these women. These include not only recurrence and survival but also donor site considerations, secondary procedures, and effects over time. The importance of proper patient counseling, with close attention to the short-term and long-term consequences, should not be dismissed. The application of these principles for ablative and reconstructive surgeons will facilitate the acceptance and success of oncoplastic surgery.
Safety in oncoplastic surgery requires attention to detail and proper technique selection. The process begins with obtaining a diagnosis. Breast cancer is diagnosed by various techniques that include fine-needle aspiration, core needle biopsy, and excisional biopsy. The next step is the excision. The importance of obtaining a clear margin becomes evident when one considers that the relative risk of developing a recurrence is 15-fold higher in patients in whom the surgical margin was not clear of tumor. The question of a positive margin being related to the type of biopsy performed has been studied and found not to be related. A positive margin was, however, related to the size of the primary tumor (T3 > T2 > T1) and to histological subtype (lobular > ductal). Preoperative identification of those women with infiltrating lobular carcinoma who may be at higher risk of a positive surgical margin can be sometimes made via mammography based on the presence of architectural distortion.
In light of the fact that larger tumors have an increased likelihood of a positive margin, the benefit of oncoplastic resections has been recognized. It has been demonstrated by Kaur, et al that resection margins are greater and the incidence of a positive margin is reduced when comparing oncoplastic resection to standard quadrantectomy. Mean resection volume in this study was 200 cm 3 following oncoplastic resection and 117 cm 3 following quadrantectomy. Giacalone, et al have demonstrated that glandular resection was increased, histological margins were wider, and the need for re-excision was decreased following oncoplastic surgery. There was a trend toward fewer mastectomies following oncoplastic resection (2/42, 4.8%) compared to standard lumpectomy (12/57, 21.1%). These facts are merely scratching the surface regarding the safety and efficacy of oncoplastic surgery. Additional studies and supportive data will be reviewed in the upcoming chapters.
Immediate reconstruction of the partial mastectomy deformity
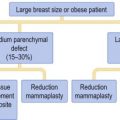
The techniques that are currently used for the reconstruction of the partial mastectomy defect are based on two different concepts: volume displacement and volume replacement. Volume displacement procedures include local tissue rearrangement, reduction mammaplasty, and mastopexy. Volume replacement procedures include local and remote flaps from various regions of the body. All of these techniques have been utilized extensively and found to be useful. The indications for each are different and various algorithms have been devised to assist with the decision process. In these studies, the selection of appropriate technique was based primarily on bra cup size and defect size. In general, women with smaller breasts with minimal ptosis were found to be better candidates for volume replacement procedures, e.g. local flap, latissimus dorsi, lateral thoracic flap; whereas women with larger and more ptotic breasts would be better candidates for volume displacement procedures, e.g. adjacent tissue rearrangement, reduction mammaplasty, mastopexy. The history of these techniques as they relate to oncoplastic surgery will be further reviewed ( Table 1.4 ).
| Study | Year | Technique | # | Morbidity | Satisfaction |
|---|---|---|---|---|---|
| Kat | 1999 | Latissimus dorsi | 30 | 38% (seroma, infection) | 100% |
| Losken | 2002 | Reduction mammaplasty | 20 | 30% (delayed healing) | 100% |
| Clough | 2003 | Reduction mammaplasty | 101 | 20% (delayed healing, fibrosis) | 88% |
| Gendy | 2003 | Latissimus dorsi | 47 | 8% (sensory changes, reduction in ADL) | 84% |
| Spear | 2003 | Reduction mammaplasty | 11 | 27% (fat necrosis) | 100% |
| Losken | 2004 | Latissimus dorsi | 30 | 33% (recurrence, seroma) | NA |
Reduction mammaplasty
It is difficult to state with certainty who first began performing immediate partial breast reconstruction; however, the individual who is most credited with the introduction and popularization is Melvin J Silverstein MD. This occurred in 1982 following the excision of a fibroadenoma. The breast was immediately repaired using a reduction mammaplasty approach.
Since then, reduction mammaplasty has been frequently utilized for oncoplastic surgery. There have been several studies that have reported on outcomes ( Table 1.5 ). Krishna Clough MD has been a significant contributor and proponent of oncoplastic resection. He began performing reduction-based oncoplastic operations in the 1980s and recently reported on his 14-year experience from the Curie Institute in Paris, France. Subjects included 101 women who were selected for oncoplastic resection because a standard lumpectomy would have resulted in a significant contour abnormality. The primary reduction technique utilized was an inverted ‘T’ with the NAC based on a superior pedicle. The contralateral reduction mammaplasty was performed immediately in 83% of women and secondarily in 17% of women. Mean tumor excision weight was 222 g. The 5-year local recurrence rate was 9.4%, the overall survival rate was 95.7%, and the metastasis-free survival rate was 82.8%. Cosmetic outcome was satisfactory in 82% of women. It was demonstrated that cosmetic outcome tended to deteriorate when radiotherapy was delivered preoperatively compared to postoperatively.
| Study | Year | Technique | Patients | Tumor size (cm) | Follow-up (months) | Margin involvement (%) | Local recurrence (%) | Cosmetic failure (%) |
|---|---|---|---|---|---|---|---|---|
| Chang | 2004 | Reduction mammaplasty | 37 | 0.6–5.2 | NR | 2.7 | 0 | NR |
| Spear | 2003 | Reduction mammaplasty | 11 | NR | 24 | 0 | 0 | NR |
| Clough | 2003 | Reduction mammaplasty | 101 | 3.2 | 46 | 10.9 | 6.9 | 12 |
| Newman | 2001 | Reduction mammaplasty | 28 | 1.5 | 24 | 7 | 0 | NR |
| Nos | 1998 | Reduction mammaplasty | 50 | 3.25 | 48 | 10 | 7 | 15 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree