Femoroacetabular impingement (FAI) is a common cause of hip pain and hip osteoarthritis in the young adult.5
 FAI is a dynamic pathologic condition that occurs when an abnormally shaped femoral head–neck and/or an overcovered acetabulum abut each other under physiologic range of motion (ROM), causing damage to the acetabular labrum and articulating cartilage.9
FAI is a dynamic pathologic condition that occurs when an abnormally shaped femoral head–neck and/or an overcovered acetabulum abut each other under physiologic range of motion (ROM), causing damage to the acetabular labrum and articulating cartilage.9
 The Ganz technique of safe surgical hip dislocation (SHD) of the hip was the first method described for treatment of FAI and helped refine the concept of FAI.1,4
The Ganz technique of safe surgical hip dislocation (SHD) of the hip was the first method described for treatment of FAI and helped refine the concept of FAI.1,4
 The greatest advantage of the SHD technique is a 360-degree visualization and access to the acetabulum and femoral neck. Unobstructed visualization allows the hip surgeon to address FAI as well as other intra-articular and extra-articular hip disorders that may require correction at the time of surgery.
The greatest advantage of the SHD technique is a 360-degree visualization and access to the acetabulum and femoral neck. Unobstructed visualization allows the hip surgeon to address FAI as well as other intra-articular and extra-articular hip disorders that may require correction at the time of surgery.
ANATOMY
The Deep Branch of the Medial Femoral Circumflex Artery
 Knowledge of the anatomy of the deep branch of the medial femoral circumflex artery (MFCA) allowed Ganz et al6 to develop a safe approach to dislocate the hip without the risk of avascular necrosis of the femoral head.
Knowledge of the anatomy of the deep branch of the medial femoral circumflex artery (MFCA) allowed Ganz et al6 to develop a safe approach to dislocate the hip without the risk of avascular necrosis of the femoral head.
 The MFCA branches from the deep femoral artery and has five constant branches: superficial, ascending, acetabular, descending, and deep. The deep branch of the MFCA supplies blood to the femoral head.6
The MFCA branches from the deep femoral artery and has five constant branches: superficial, ascending, acetabular, descending, and deep. The deep branch of the MFCA supplies blood to the femoral head.6
 The deep branch of the MFCA lies at an average of 8.8 mm from the insertion of the obturator externus. It runs between the pectineus medially and iliopsoas tendon laterally along the inferior border of the obturator externus. It reaches the trochanter proximal to the quadratus femoris muscle, where it leads to the trochanteric branch. The trochanteric branch of the deep MFCA crosses over the trochanteric crest toward the lateral aspect of the greater trochanter.
The deep branch of the MFCA lies at an average of 8.8 mm from the insertion of the obturator externus. It runs between the pectineus medially and iliopsoas tendon laterally along the inferior border of the obturator externus. It reaches the trochanter proximal to the quadratus femoris muscle, where it leads to the trochanteric branch. The trochanteric branch of the deep MFCA crosses over the trochanteric crest toward the lateral aspect of the greater trochanter.
 The main deep branch of the MFCA crosses the tendon of the obturator externus posteriorly and continues its course anteriorly to the tendons of the superior gemellus, obturator internus, and inferior gemellus. It is found at an average of 1.5 cm from the lesser trochanter. The deep branch perforates the capsule just proximal to the insertion of the tendon of the superior gemellus and distal to the tendon of the piriformis, where it commonly divides into two of four terminal branches. Covered by synovium, these branches continue their course and perforate the femoral head at 2 to 4 mm lateral to the bone–cartilage junction.
The main deep branch of the MFCA crosses the tendon of the obturator externus posteriorly and continues its course anteriorly to the tendons of the superior gemellus, obturator internus, and inferior gemellus. It is found at an average of 1.5 cm from the lesser trochanter. The deep branch perforates the capsule just proximal to the insertion of the tendon of the superior gemellus and distal to the tendon of the piriformis, where it commonly divides into two of four terminal branches. Covered by synovium, these branches continue their course and perforate the femoral head at 2 to 4 mm lateral to the bone–cartilage junction.
 The anastomosis between the inferior gluteal artery and the MFCA occurs at the inferior border of the piriformis. This constant anastomosis must be preserved.
The anastomosis between the inferior gluteal artery and the MFCA occurs at the inferior border of the piriformis. This constant anastomosis must be preserved.
 Surgical dislocation of the hip does not cause significant strain on the deep branch of the MFCA.
Surgical dislocation of the hip does not cause significant strain on the deep branch of the MFCA.
Trochanteric Trigastric (Flip) Osteotomy
 During the trochanteric flip osteotomy, the trochanter is cut from posterior to anterior. The flip osteotomy allows the hip to be exposed anteriorly and dislocated in the same direction without disrupting the short external rotators or the MFCA. The trochanteric osteotomy also minimizes injury to the superior gluteal neurovascular bundle by maintaining the abductors in continuity.
During the trochanteric flip osteotomy, the trochanter is cut from posterior to anterior. The flip osteotomy allows the hip to be exposed anteriorly and dislocated in the same direction without disrupting the short external rotators or the MFCA. The trochanteric osteotomy also minimizes injury to the superior gluteal neurovascular bundle by maintaining the abductors in continuity.
Acetabular Labrum
 The acetabular labrum is a triangular fibrocartilaginous structure that is attached to the bony acetabular rim. The labrum is a relatively avascular structure. The main blood supply is from the hip capsule to the periphery of the labrum.
The acetabular labrum is a triangular fibrocartilaginous structure that is attached to the bony acetabular rim. The labrum is a relatively avascular structure. The main blood supply is from the hip capsule to the periphery of the labrum.
 The labrum helps with the stability of the hip by lateralizing femoral head coverage as well as maintaining a suction seal of the hip joint.
The labrum helps with the stability of the hip by lateralizing femoral head coverage as well as maintaining a suction seal of the hip joint.
 The labral innervation comes from a branch of the nerve to the quadratus femoris and from the obturator nerve. Sensory nerve organs as well as free nerve endings suggest that the injury to the labrum causes pain and is important in proprioception.
The labral innervation comes from a branch of the nerve to the quadratus femoris and from the obturator nerve. Sensory nerve organs as well as free nerve endings suggest that the injury to the labrum causes pain and is important in proprioception.
Femoral Head–Neck Osteopathy
 A precise knowledge of superior retinacular vessel anatomy is necessary for any procedures at the femoral neck. The femoral head–neck osteochondroplasty is performed in FAI surgery to increase the femoral head offset.
A precise knowledge of superior retinacular vessel anatomy is necessary for any procedures at the femoral neck. The femoral head–neck osteochondroplasty is performed in FAI surgery to increase the femoral head offset.
 The superior retinacular vessels are located over the posterosuperior neck. They are covered by synovial tissue and perforate 2 to 4 mm lateral to the articular margin. The retinacular vessels must be always visualized.
The superior retinacular vessels are located over the posterosuperior neck. They are covered by synovial tissue and perforate 2 to 4 mm lateral to the articular margin. The retinacular vessels must be always visualized.
PATHOMECHANICS
 FAI is a dynamic process where there is abutment between the acetabular rim and the femoral neck under physiologic ROM of the hip. Repetitive trauma during impingement leads to labral pathology and cartilage degeneration.5
FAI is a dynamic process where there is abutment between the acetabular rim and the femoral neck under physiologic ROM of the hip. Repetitive trauma during impingement leads to labral pathology and cartilage degeneration.5
 The decreased femoral offset at the head–neck junction and the lack of sphericity of the femoral head is known as a cam morphology (also described as a pistol grip or head tilt deformity). Cam impingement is more common in young males.3
The decreased femoral offset at the head–neck junction and the lack of sphericity of the femoral head is known as a cam morphology (also described as a pistol grip or head tilt deformity). Cam impingement is more common in young males.3
 Cam deformity causes damage mainly to the anterior superior acetabular cartilage during hip flexion, causing chondrolabral separation and shearing of the acetabular cartilage from subchondral bone.
Cam deformity causes damage mainly to the anterior superior acetabular cartilage during hip flexion, causing chondrolabral separation and shearing of the acetabular cartilage from subchondral bone.
 Pincer impingement is caused by excessive coverage of the acetabulum. This can be seen in patients with acetabular retroversion or coxa profunda. Pincer is more common in females and the pattern of labral injury is seen in the anterior superior acetabulum, globally or posteriorly (coup–contrecoup).
Pincer impingement is caused by excessive coverage of the acetabulum. This can be seen in patients with acetabular retroversion or coxa profunda. Pincer is more common in females and the pattern of labral injury is seen in the anterior superior acetabulum, globally or posteriorly (coup–contrecoup).
 The combination of cam and pincer is most commonly the mechanism in FAI.
The combination of cam and pincer is most commonly the mechanism in FAI.
NATURAL HISTORY
 FAI is a major etiologic factor in the development of early degenerative joint disease of the hip. Although the natural history of FAI needs further understanding, the pathophysiology and clinical data suggest that FAI plays an important role in early hip osteoarthritis in the young adult.5
FAI is a major etiologic factor in the development of early degenerative joint disease of the hip. Although the natural history of FAI needs further understanding, the pathophysiology and clinical data suggest that FAI plays an important role in early hip osteoarthritis in the young adult.5
PATIENT HISTORY AND PHYSICAL FINDINGS
 The main goal of performing a clinical history and physical examination in the young adult with hip pain is to establish a differential diagnosis and determine if the origin of pain is intra- or extra-articular.10
The main goal of performing a clinical history and physical examination in the young adult with hip pain is to establish a differential diagnosis and determine if the origin of pain is intra- or extra-articular.10
 FAI is one cause of intra-articular hip pain in the young adult.
FAI is one cause of intra-articular hip pain in the young adult.
 Most patients are active and pain is related to activities that flex, rotate, or load the joint. Pain is usually reproduced in positions of hip flexion such as prolonged sitting.
Most patients are active and pain is related to activities that flex, rotate, or load the joint. Pain is usually reproduced in positions of hip flexion such as prolonged sitting.
 The distribution of pain in FAI includes the groin (88%), lateral hip (67%), anterior thigh (35%), and buttocks (29%).8
The distribution of pain in FAI includes the groin (88%), lateral hip (67%), anterior thigh (35%), and buttocks (29%).8
 Associated symptoms include hip snapping, catching, locking, and weakness.
Associated symptoms include hip snapping, catching, locking, and weakness.
 The physical evaluation includes observation of gait pattern (foot progression angle and abductors’ strength) and seating posture, passive hip ROM,11 and provocative hip tests.
The physical evaluation includes observation of gait pattern (foot progression angle and abductors’ strength) and seating posture, passive hip ROM,11 and provocative hip tests.
 Common provocative hip tests include the following:
Common provocative hip tests include the following:
The classic FAI impingement test (flexion, adduction, and internal rotation)
Flexion, abduction, and external rotation
Lateral rim impingement (abduction)
Posterior rim impingement (extension, abduction, and external rotation)
Stinchfield (hip flexion–straight-leg raise against resistance)
 A diagnostic image-guided intra-articular hip injection can help to determine if the pain is related to an intra-articular hip disorder.
A diagnostic image-guided intra-articular hip injection can help to determine if the pain is related to an intra-articular hip disorder.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Radiographs are the main diagnosis modality for FAI. Advanced cross-sectional studies, such as computed tomography (CT) and magnetic resonance arthrogram (MRA), are used to further characterize the acetabulum and femur’s bony and soft tissue structures.
Radiographs are the main diagnosis modality for FAI. Advanced cross-sectional studies, such as computed tomography (CT) and magnetic resonance arthrogram (MRA), are used to further characterize the acetabulum and femur’s bony and soft tissue structures.
 Plain radiographs are used in the evaluation of subtle bony structural abnormalities such as hip dysplasia or FAI. The recommended views include a true standing anteroposterior pelvis, frog-leg lateral, cross-table lateral, and false-profile pelvis.
Plain radiographs are used in the evaluation of subtle bony structural abnormalities such as hip dysplasia or FAI. The recommended views include a true standing anteroposterior pelvis, frog-leg lateral, cross-table lateral, and false-profile pelvis.
 The orthopaedic surgeon needs to assess the degree of hip osteoarthritis, amount of anterior and lateral acetabular coverage, acetabular version and depth, femoral head sphericity, and amount of femoral head–neck offset seen on plain radiographs.
The orthopaedic surgeon needs to assess the degree of hip osteoarthritis, amount of anterior and lateral acetabular coverage, acetabular version and depth, femoral head sphericity, and amount of femoral head–neck offset seen on plain radiographs.
 MRA is commonly used to detect the presence of labral and chondral damage associated with FAI. Additionally, MRA can help rule out other differential diagnosis of hip pain.
MRA is commonly used to detect the presence of labral and chondral damage associated with FAI. Additionally, MRA can help rule out other differential diagnosis of hip pain.
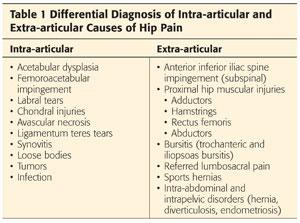
DIFFERENTIAL DIAGNOSIS
 See Table 1.
See Table 1.
NONOPERATIVE MANAGEMENT
 Nonsurgical management should be the first line of treatment for FAI. This includes restriction of activities that place the hip in extreme ROM or high-impact activities.
Nonsurgical management should be the first line of treatment for FAI. This includes restriction of activities that place the hip in extreme ROM or high-impact activities.
 Nonsteroidal anti-inflammatory medications are recommended to alleviate symptoms.
Nonsteroidal anti-inflammatory medications are recommended to alleviate symptoms.
 Physical therapy to maintain core and hip muscle strength is recommended.
Physical therapy to maintain core and hip muscle strength is recommended.
 Physical therapy aiming to improve ROM is contraindicated.
Physical therapy aiming to improve ROM is contraindicated.
SURGICAL MANAGEMENT
 The decision to proceed with open versus arthroscopic surgery for surgical treatment of FAI should be based on the patient’s anatomy, surgeon’s experience/preference, and potential rehabilitation.7
The decision to proceed with open versus arthroscopic surgery for surgical treatment of FAI should be based on the patient’s anatomy, surgeon’s experience/preference, and potential rehabilitation.7
Indications for Surgical Hip Dislocation to Treat Femoroacetabular Impingement
 Patients younger than 40 years with preserved articular cartilage and the following:
Patients younger than 40 years with preserved articular cartilage and the following:
Coxa profunda, defined as lateral center edge angle greater than 40 degree
Cam lesions extending over the retinacular vessels as seen on CT scan or radiographs
High-riding trochanter from old Perthes or slipped capital femoral epiphysis
• Trochanteric advancement and relative lengthening can be performed.
Combined procedures to address both intra-articular and extra-articular impingement
• Combined periacetabular osteotomy and SHD
• Combined derotational femoral osteotomy and SHD
Anticipated labral reconstruction (fascia lata or round ligament autograft)
 Other non-FAI indications for SHD include the following:
Other non-FAI indications for SHD include the following:
Femoral head and/or acetabular fracture
Removal of intra-articular heterotopic bone
Benign tumors
• Synovial chondromatosis
• Pigmented villonodular synovitis
• Proximal femur osteochondromas and enchondromas
Contraindications for Surgical Hip Dislocation to Treat Femoroacetabular Impingement
 Patients age 40 years old and older2
Patients age 40 years old and older2
 Extensive cartilage damage
Extensive cartilage damage
Anterior hip subluxation
Anterior and posterior cartilage damage (coup–contrecoup)
 No clearly defined pathology causing hip pain
No clearly defined pathology causing hip pain
 Pain out of proportion
Pain out of proportion
 Smokers
Smokers
Preoperative Planning
 Preoperative planning is based on clinical evaluation and radiographic assessment.
Preoperative planning is based on clinical evaluation and radiographic assessment.
 The amount of acetabular bony resection should not exceed 25 degrees of lateral coverage.
The amount of acetabular bony resection should not exceed 25 degrees of lateral coverage.
 The cam deformity is resected until impingement-free ROM is obtained. Thirty percent of the head and neck diameter is considered the maximum amount of cam resection without affecting the load to failure, but the correction never extends to that amount.
The cam deformity is resected until impingement-free ROM is obtained. Thirty percent of the head and neck diameter is considered the maximum amount of cam resection without affecting the load to failure, but the correction never extends to that amount.
Positioning
 The patient is placed in the lateral decubitus position.
The patient is placed in the lateral decubitus position.
 Hip ROM and impingement with internal rotation at 90 degrees is measured. This is used as future reference during the offset procedure.
Hip ROM and impingement with internal rotation at 90 degrees is measured. This is used as future reference during the offset procedure.
Approach
 Posterior Kocher or Gibson approach with osteotomy of the greater trochanter
Posterior Kocher or Gibson approach with osteotomy of the greater trochanter
 Perform a straight lateral incision centered over the greater trochanter. The size of the incision averages 15 cm. Incise skin and subcutaneous tissue down to the fascia.
Perform a straight lateral incision centered over the greater trochanter. The size of the incision averages 15 cm. Incise skin and subcutaneous tissue down to the fascia.
 Elevate the subcutaneous tissue from the anterior fascia until perforators are encountered.
Elevate the subcutaneous tissue from the anterior fascia until perforators are encountered.
 Leg position 1: straight lateral on the table (tensions fascia, allowing easy visualization of Gibson interval if the surgeon prefers)
Leg position 1: straight lateral on the table (tensions fascia, allowing easy visualization of Gibson interval if the surgeon prefers)
 These vessels mark the plane that divides the anterior border of the gluteus maximus with the underlying muscles. Incise the fascia through this interval starting from distal to proximal, ensuring that the gluteus maximus fibers head posteriorly.
These vessels mark the plane that divides the anterior border of the gluteus maximus with the underlying muscles. Incise the fascia through this interval starting from distal to proximal, ensuring that the gluteus maximus fibers head posteriorly.
 Peel the gluteus maximus posteriorly off the gluteus medius, including its overlying shiny fascia, because the pedicle to the anterior half of the gluteus maximus muscle runs within this gluteus medius fascia. Dissect the interval proximally as far up as possible.
Peel the gluteus maximus posteriorly off the gluteus medius, including its overlying shiny fascia, because the pedicle to the anterior half of the gluteus maximus muscle runs within this gluteus medius fascia. Dissect the interval proximally as far up as possible.
TECHNIQUES
 Trochanteric Trigastric (Flip) Osteotomy
Trochanteric Trigastric (Flip) Osteotomy
The objective of the osteotomy is to leave the gluteus medius tendon, long tendon of the gluteus minimus tendon, and vastus lateralis tendon attached to the mobile trochanter. The stable trochanter is preserved with the piriformis and all other external rotators.
Incise gliding tissue over the posterior border of the trochanter over the bursa in a straight line similar to fascia for closure over the trochanter and screws after surgery.
Leg position 2: Internal rotation and extension of the hip allows better visualization of the posterior trochanter, short rotators, and sciatic nerve.
A safe distance to mark the proximal starting point of the osteotomy is 5 mm anterior to the trochanteric overhang (TECH FIG 1A,B).
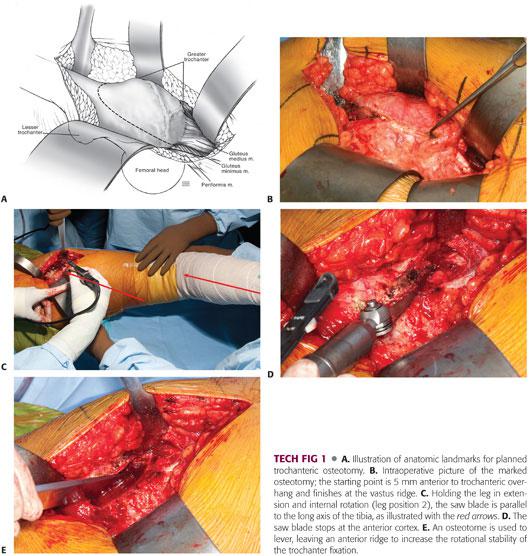
Perform the osteotomy from the posterior trochanter toward the vastus ridge. The saw blade must be parallel to the long axis of the leg (tibia) with the hip internally rotated over the table (TECH FIG 1C). Stop the saw at the anterior cortex (TECH FIG 1D). Complete the osteotomy by levering the fragment with an osteotome. The anterior ridge created potentially increases rotational stability of the trochanter after fixation (TECH FIG 1E).
Open the osteotomy using a Hohmann retractor. Beware of potential damage to the femoral head if the Hohmann retractor is placed too far anterior or left in place when exposing the anterior capsule (especially in a Perthes hip with a short neck).
Use the knife to cut the remaining gluteus medius fibers and vastus lateralis intermedius fibers off the stable trochanter. Aim the knife blade parallel to the femur and stable trochanter.
A shiny fat pad is visible anterior to the posterosuperior tip of the trochanter. Incise only through this gap to visualize the capsule. Occasionally, fibers of the piriformis tendon remain attached to the trochanteric fragment and must be cut to allow further mobilization of the trochanter. The anterior Hohmann retractor should be exchanged for a Meyerding or knee retractor.
Incise the vastus fascia posteriorly, just anterior to the intramuscular septum. Using sharp dissection, elevate the vastus lateralis muscle subperiosteally in continuity with the trochanteric fragment. This dissection continues over the anterior border of the proximal femur by releasing proximal attachments of the vastus intermedius and lateralis up to the inferior medial aspect of the capsule. The mobile trochanter should become more and more retractable while the assistant flexes and externally rotates the hip.
 Capsular Exposure
Capsular Exposure
Leg position 3: Flexion and external rotation of the hip decreases tension over the posterior interval between piriformis and gluteus minimus and trochanteric flip (TECH FIG 2A).

The gluteus medius muscle is gently retracted in an anterosuperior direction using a narrow Deaver retractor. Mobilizing the gluteus medius provides exposure of the piriformis and gluteus minimus muscles.
Find the interval between the piriformis and the gluteus minimus proximally (TECH FIG 2B). Stay proximal to the piriformis tendon because an anastomosis between the deep branch of the MFCA and inferior gluteal artery runs inferior to the piriformis.
Elevate the gluteus minimus off the superior and posterior capsule down to the sciatic notch. Be careful because the nerve to the gluteus minimus runs anterior over the muscle and not far from the distal border. The gluteus minimus must be elevated enough to avoid damage at the time of femoral head dislocation.
The superior dissection can be carried up anteriorly to the reflected head of the rectus, which becomes visible over the acetabular rim.
Anteroinferiorly, the insertions of the short head of the minimus onto the capsule should be released. The remaining capsular thickening is known as a Bigelow ligament.
The trochanteric fragment is retracted anteriorly throughout this exposure. Increasing flexion and abduction facilitates anterior retraction of the trochanteric fragment. A complete anterior, superior, and posterior capsular exposure should be obtained.
The insertions of the short external rotator muscles and the piriformis muscle are left intact to protect the deep branch of the MFCA.
 Z–Shaped Capsulotomy
Z–Shaped Capsulotomy
A Z-shaped capsulotomy for the right hip and an inverse Z-shaped capsulotomy for the left hip are performed (TECH FIG 3A).
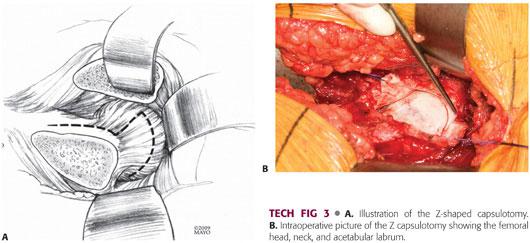
Use the knife blade to perform the Z-shaped capsulotomy. Start at the anterosuperior edge of the stable trochanter toward the acetabular rim along the long axis of the neck from distal to proximal. Initially, start with 2 cm, then begin the perpendicular anterior limb (just 1 cm), enough to see the joint inside. Continue to carry the transverse limb of the capsulotomy with a knife from inside out, so that the labrum can be seen as the rim is approached. Use Vicryl 0 to tag each side of the transverse limb of the capsulotomy (TECH FIG 3B).
Use an 8-mm Hohmann retractor in the anterior wall, taking care not to damage the anterior labrum or cartilage next to the rim. This places the anterior capsule at stretch.
Complete the capsulotomy anteriorly inside-out until the iliacus muscle is visualized. Posteriorly carry the capsulotomy along the acetabular rim, taking care not to injure the labrum.
Use a superior acetabular Hohmann or large Langenbeck retractor in the ilium.
 Femoral Head Dislocation
Femoral Head Dislocation
Leg position 4: Hip is flexed and externally rotated, and foot is brought into sterile pocket.
Use a bone hook on the neck to sublux the femoral head out of the acetabulum. Use large parametrium (90 degrees) scissors to cut the round ligament. The head is dislocated and the leg is flexed and externally rotated and placed inside the pocket.
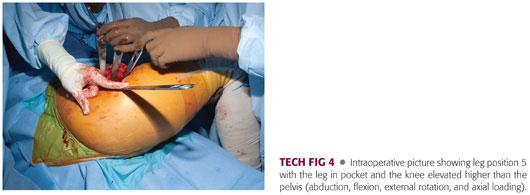
Leg position 5: leg in pocket. Elevate the knee higher than pelvis and toward the head of the patient (abduction, flexion, external rotation, and axial loading) with a gentle axial push at the knee to push the femoral head posteriorly, creating enough space to have 360-degree visualization of the acetabulum (TECH FIG 4).
Place the inferior cobra retractor into the teardrop. This move assists posterior and inferior subluxation of the femoral head.
 Acetabulum and Labrum
Acetabulum and Labrum
Inspection, labral takedown, and rim trimming can be performed with a 360-degree direct visualization of the acetabulum (TECH FIG 5A).
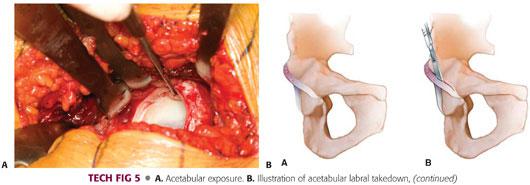
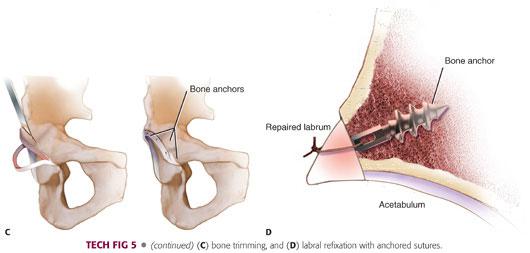
The rim trimming is performed at the site of acetabular impingement, most commonly located in the anterosuperior acetabulum at the 12 o’clock to 3 o’clock positions.
Bone resection down to healthy rim cartilage can be performed with a high-speed burr or with a narrow curved osteotome (if roof is large enough). The amount of bone removed depends on the cartilage damage and the depth of the socket (TECH FIG 5B–D).
Nonabsorbable anchored sutures (2-0 Ethibond) are used for labral refixation into the acetabular rim. The knots should be tied over the rim outside of the joint, taking care to pass the suture through the undersurface of the labrum so that it is not reattached in the inverted manner or too high. Three or four anchors are usually used.
 Femoral Head and Neck Resection
Femoral Head and Neck Resection
Leg position 6: Remove the inferior cobra retractor and bring the knee down (adduction), keeping the leg position within the sterile pocket for femoral head and neck exposure.
Place two Eva retractors underneath the femoral neck.
Remove the ligamentum teres at this time.
Assess the femoral head offset and mark out the area to be removed.
A change in cartilage color may be visible where the offset problem begins. Remove excess bone and recreate femoral neck waist (TECH FIG 6A).
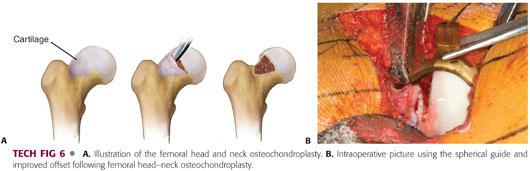
Always visualize the retinaculum. The retinacular vessels penetrate the femoral neck about 2 to 4 mm lateral to the cartilage bone junction posterosuperiorly. If an offset is present near the retinaculum, it is safer to bring the osteotome proximal to distal, not too deeply, because it may cross the intraosseous vessels. Stop at the superior border of retinaculum; break the piece of bone off and, using a knife in an inside-out maneuver, detach the piece from the soft tissues.
After the femoral head–neck offset has been recreated, use femoral head templates to verify good neck clearance (TECH FIG 6B).
Reduce hip and check ROM for impingement. Internal rotation of 45 degrees free of impingement should be obtained.
Place bone wax into cancellous bone of the head–neck junction to prevent capsular adhesions.
Loose capsular closure prevents hematoma formation and stretch of retinacular vessels, decreasing blood flow to the femoral head.
Evaluate for extra-articular impingement (posterior trochanter on pelvis). If necessary, trim the posterior stable trochanter.
 Extended Retinacular Soft Tissue Flap: A Technique for Severe Femoral Head Deformities and Extra-articular Greater Trochanteric Impingement
Extended Retinacular Soft Tissue Flap: A Technique for Severe Femoral Head Deformities and Extra-articular Greater Trochanteric Impingement
The medial retinacular soft tissue flap as described by Ganz et al6 allows extending the SHD approach to treat sequelae of slipped capital epiphysis or Perthes deformities.
The soft tissue flap is developed by subperiosteal release of the external rotators.
Leg position 1: straight lateral on the table. Femoral head is reduced into the acetabular socket.
Expose the cancellous bone of the stable trochanter by retracting the mobile trochanteric fragment anteriorly with a Meyerding or knee retractor.
Visualize the retinaculum.
Using a small osteotome, the posterior stable trochanter is reduced in a piecemeal fashion. Avoid posterior penetration with the osteotome. The mobilized fragments are turned and subperiosteal elevation of the osteotomized pieces is performed under direct visualization with a knife. This is performed until the osteotomy surface levels the posterior and superior surface of the neck.
The periosteum anterior to the retinacular vessels is incised longitudinally with a knife at the superior femoral neck. The periosteum distal to the quadratus femoris is also incised and mobilized posteriorly. The subperiosteal flap is developed posteriorly, containing the deep branch of the MFCA and the retinacular vessels.
The retinacular soft tissue flap allows performing relative lengthening of the femoral neck to manage intra- and extra-articular impingement, improve ROM, and improve the abductor mechanism strength.
The relative neck lengthening is obtained at the superior femoral neck without affecting the overall lower extremity length. This is performed by distally advancing the trochanter and trimming the posterior superior circumference of the trochanter.
 Trochanteric Reattachment and Closure
Trochanteric Reattachment and Closure
For trochanteric reattachment, use a bone hook to pull distally and internally rotate the fragment. The fragment is reduced in anatomic position with the bone hook or with a ball spike pusher (Picador) held by the assistant.
Two or three 4.5-mm screws, commonly 65 to 70 mm in men and 55 to 60 mm in women, are used for fixation of the greater trochanter. Medial and lateral are the preferred location for screw fixation.
The bursa is closed over the screws with a running 2-0 Vicryl suture for gliding tissue reconstruction.
Layered closure including the fascia, subcutaneous tissues, and skin is performed.
Subcutaneous tissue and skin closure is routine. Suction drainage is only occasionally needed.
PEARLS AND PITFALLS | |
Trochanteric osteotomy |
|
| |
| |
Capsule exposure |
|
HO |
|
| |
Labral injury at exposure |
|
Sciatic nerve compression |
|
Painful screws |
|
Femoral neck fractures |
|
Capsular adhesions |
|
POSTOPERATIVE CARE
 Patients undergoing surgery for FAI are mobilized the day following surgery.
Patients undergoing surgery for FAI are mobilized the day following surgery.
 Passive- and active-assisted internal or external rotation is permitted to protect trochanteric fixation. Passive ROM is initiated immediately with the use of a continuous passive motion (CPM) machine 6 hours a day for 6 weeks. A stationary bike may begin at week 2.
Passive- and active-assisted internal or external rotation is permitted to protect trochanteric fixation. Passive ROM is initiated immediately with the use of a continuous passive motion (CPM) machine 6 hours a day for 6 weeks. A stationary bike may begin at week 2.
 Hip flexion is limited to 90 degrees.
Hip flexion is limited to 90 degrees.
 The patients are touch weight bearing for the first 4 weeks after surgery.
The patients are touch weight bearing for the first 4 weeks after surgery.
 Weight bearing is advanced after 4 weeks.
Weight bearing is advanced after 4 weeks.
 Active abductor strengthening begins at week 4.
Active abductor strengthening begins at week 4.
 Our protocol is to see patients for follow-up 8 weeks after surgery. At that time, patients are typically on one crutch or using no support.
Our protocol is to see patients for follow-up 8 weeks after surgery. At that time, patients are typically on one crutch or using no support.
 Muscle weakness may persist for 3 months after surgery and abductor rehabilitation is continued throughout the ensuing months.
Muscle weakness may persist for 3 months after surgery and abductor rehabilitation is continued throughout the ensuing months.
 A therapist who specializes in return to sports programs supervises the return to high-impact pivoting sports, which usually does not occur before 6 months.
A therapist who specializes in return to sports programs supervises the return to high-impact pivoting sports, which usually does not occur before 6 months.
 Screws are removed at 3 months in athletes.
Screws are removed at 3 months in athletes.
OUTCOMES
 The current literature to assess the outcomes of SHD is level IV, evidence from small case series studies reporting early and midterm results.
The current literature to assess the outcomes of SHD is level IV, evidence from small case series studies reporting early and midterm results.
 Good to excellent results have been seen in 70% to 90% of patients at 2 to 5 years follow-up.
Good to excellent results have been seen in 70% to 90% of patients at 2 to 5 years follow-up.
 Patient selection is very important. Those older than 40 years or patients with degenerative changes have less favorable results.
Patient selection is very important. Those older than 40 years or patients with degenerative changes have less favorable results.
COMPLICATIONS
 Heterotopic ossification (HO) (37%; most were Brooker type 1)
Heterotopic ossification (HO) (37%; most were Brooker type 1)
 Trochanter nonunion and failure of trochanteric fixation (1% to 2%)
Trochanter nonunion and failure of trochanteric fixation (1% to 2%)
 Sciatic nerve neurapraxia (<1%)
Sciatic nerve neurapraxia (<1%)
REFERENCES
1. Beck M, Leunig M, Parvizi J, et al. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res 2004;(418):67–73.
2. Boone GR, Pagnotto MR, Walker JA, et al. Caution should be taken in performing surgical hip dislocation for the treatment of femoroacetabular impingement in patients over the age of 40. HSS J 2012;8:230–234.
3. Clohisy JC, Baca G, Beaule PE, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med 2013;41:1348–1356.
4. Espinosa N, Beck M, Rothenfluh DA, et al. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. Surgical technique. J Bone Joint Surg Am 2007;89(suppl 2, pt 1):36–53.
5. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;417:112–120.
6. Gautier E, Ganz K, Krugel N, et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br 2000;82:679–683.
7. Nepple JJ, Byrd JW, Siebenrock KA, et al. Overview of treatment options, clinical results, and controversies in the management of femoroacetabular impingement. J Am Acad Orthop Surg 2013;21(suppl 1):S53–S58.
8. Nepple JJ, Prather H, Trousdale RT, et al. Clinical diagnosis of femoroacetabular impingement. J Am Acad Orthop Surg 2013;21(suppl 1):S16–S19.
9. Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg 2007;15:561–570.
10. Sierra RJ, Trousdale RT, Ganz R, et al. Hip disease in the young, active patient: evaluation and nonarthroplasty surgical options. J Am Acad Orthop Surg 2008;16:689–703.
11. Yuan BJ, Bartelt RB, Levy BA, et al. Decreased range of motion is associated with structural hip deformity in asymptomatic adolescent athletes. Am J Sports Med 2013;41:1519–1525.
< div class='tao-gold-member'>














