Gynecomastia
Dennis C. Hammond
Eric Yu Kit Li
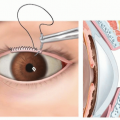
ANATOMY
In healthy patients, the male breast resembles that of a prepubescent female.
Fat is the predominant tissue and lobules are absent, in contrast to ductal and lobular development in females (FIG 1).
The ideal male breast is also flat, to accentuate the contour of the underlying pectoralis major muscle.
The arterial supply, venous drainage, lymphatic drainage, and sensory supply mimic those of the female breast.
Although there is general consensus on the ideal size, shape, and location of the nipple-areolar complex (NAC) in women, this subject has been less extensively studied in men.
Various authors have published equations to calculate the ideal NAC on the male torso, often as a function of measurements such as patient height and chest circumference.3,4,5,6,7,8
Some general themes exist among the various formulas, in that the ideal male NAC is
Slightly oval (horizontal greater than vertical)
Smaller (with diameter lesser than 3 cm)
Positioned around the 4th or 5th intercostal space
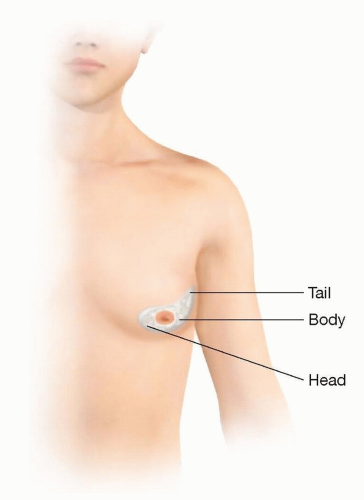
Recent studies have characterized the shape of gynecomastia specimens as having a head, body, and tail9,10 (FIG 2).
The head is semicircular in shape and extends toward the midline.
The body is located directly underneath the NAC and intimately attached to it.
The tail tapers off and extends toward the axilla.
Awareness of this shape may help guide intraoperative dissection.
PATHOGENESIS
Gynecomastia occurs due to a hormonal imbalance between the level or action of estrogens and androgens.1,2
Estrogens stimulate breast development, whereas androgens inhibit it.
Causes of this imbalance may be idiopathic, physiologic, pharmacologic, or pathologic.11
FIG 1 • In the normal male breast, fat is the predominant tissue and lobules are absent. This is in contrast to the developed female breast, which features lobules and ducts.
Obesity is also strongly associated with gynecomastia, due to increased levels of circulating estrogens from peripheral aromatization of androgens in adipose tissue.1
Histopathologically, early-stage gynecomastia is characterized by ductal proliferation with loose stromal tissue (florid type).12
Over time, generally over the course of a year, the stromal tissue undergoes fibrosis (fibrotic type).12
Gynecomastia that has undergone fibrosis is unlikely to be responsive to medical treatment.
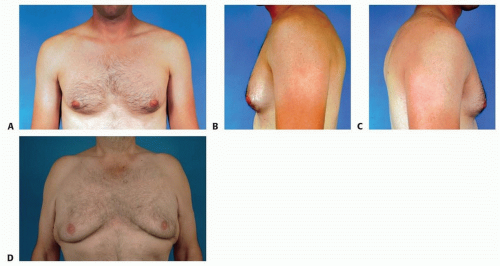
Physiologic gynecomastia (FIG 3A-C)
Often seen in newborns, adolescents, and older men
Adolescent gynecomastia:
May begin as early as age 12
Can occur in up to 65% of adolescent boys13
Breast enlargement typically lasts 6 to 12 months.
Ninety percent of cases spontaneously resolve without treatment.14
Generally, presents as a subareolar, firm, concentric, fibrous mass with surrounding fibrofatty tissue that is proportional to the body habitus of the patient
Senescent gynecomastia (FIG 3D):
Can occur in up to 65% of men over 65 years of age15
Generally presents as diffuse fibrofatty tissue that gradually enlarges over time
Pathologic gynecomastia
Can occur at any age, related to a tumor or medical condition (eg, liver or kidney disease)
There may be a history of rapid eccentric growth, nipple discharge, skin changes, or constitutional symptoms.12
Pharmacologic gynecomastia
Can occur at any age, related to a drug exposure.
Generally presents as a subareolar, firm, concentric, mass.
If the mass is not fibrotic, stopping the offending medication may resolve the condition.
If the mass is fibrotic, stopping the offending medication may halt progression of gynecomastia, but it is unlikely to reduce the breast enlargement already present.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with the suspected diagnosis should be evaluated for both signs and symptoms related to the abnormal breast growth.
A detailed history should inquire about:
The onset and velocity of breast growth
The onset of puberty and ongoing pubertal development (if applicable)
Any tendency for spontaneous resolution of the breast hypertrophy
Associated symptoms, including pain, tenderness, weight loss, night sweats, and general malaise
Any social, vocational, or avocational dysfunction due to the breast enlargement
The effect of the breasts on the patient’s psychological well-being and self-esteem
Any personal or family history of breast cancer or disorders
Medication history, especially recreational and off-thecounter drugs (eg, marijuana and exogenous steroids)
Symptoms suggestive of underlying thyroid, liver, or kidney disease
A detailed physical should examine
The patient’s height, weight, and body mass index
For the development of secondary sexual characteristics (if applicable)
For the presence of a subareolar mass and its area of involvement
For the presence of fibrofatty tissue and its area of involvement
For other masses, irregularities, or deformities involving the breasts or chest wall
Overall breast aesthetics, including the shape, size, and symmetry of the breasts and NACs, the degree of ptosis, excess skin, and the position and symmetry of the inframammary folds (IMFs)
Standard breast measurements to highlight asymmetries, including the sternal notch to nipple, midclavicular to nipple, nipple to midline, and nipple to IMF distances
The patient’s neck, abdomen, and testicles for any masses or irregularities
IMAGING
Imaging is not typically required if the history and physical examination are consistent with physiologic gynecomastia.
In suspected cases of pathologic gynecomastia, appropriate imaging (mammogram, ultrasound, etc.) should be carried out based on the identified or suspected abnormalities.
DIFFERENTIAL DIAGNOSIS
Idiopathic gynecomastia
Physiologic gynecomastia
Pseudogynecomastia or lipomastia
Benign breast tumors (eg, fibroadenoma, giant fibroadenoma, phyllodes tumor, lipoma, or cysts)
Malignant breast tumors (eg, ductal or lobular carcinoma, lymphoma, or metastases)
NONOPERATIVE MANAGEMENT
Patient reassurance is the foremost treatment in adolescent gynecomastia.
About 90% of adolescent cases spontaneously resolve, so no treatment may be needed at all.14
Treatment is indicated when gynecomastia has persisted for more than 2 years, or if there are overriding functional, medical, or psychosocial concerns that warrant earlier intervention.16
In gynecomastia related to reversible etiologies, the offending medication should be stopped or the underlying condition treated as soon as possible.
Weight loss through dietary restriction and exercise are important first-line treatments in any gynecomastia related to obesity.
Pharmacologic therapies, including danazol, tamoxifen, and anastrozole, may be effective in preventing or treating earlystage gynecomastia but are less effective once breast tissues undergo fibrosis.2
Of these medications, tamoxifen is most widely used, but there are no clear guidelines on the ideal dose or duration.
All medications also have unfavorable side effects that must be considered.
If pathologic gynecomastia is suspected, patients should be urgently referred to the appropriate specialist(s).
SURGICAL MANAGEMENT
Surgical treatment is indicated when gynecomastia is persistent or causes functional or aesthetic concerns.
Options include liposuction, excision of the subareolar fibrous tissue, or a combination of the two.
In patients with significant breast enlargement with skin excess and ptosis, mastopexy may be incorporated as well.
Although weight loss should be the first-line strategy in any obese patient with gynecomastia, it is still reasonable to proceed with surgery in obese patients since normalizing the chest wall contour may allow the patient to lead a more active lifestyle.16
Whether resected gynecomastia tissues should be routinely sent for histopathological examination is debatable.
Of note, the College of American Pathologists does not specifically require the use of cancer protocols for gynecomastia, nor do they offer any formal guidelines for the examination of gynecomastia tissue.
Preoperative Planning
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree