Abstract
Management of frontal sinus and anterior skull base injuries can be complex. Accurate diagnosis and meticulous surgical technique are required to obtain optimal surgical results. This chapter reviews key anatomy, pathophysiology, and surgical techniques used for management of these injuries. Controversies in surgical decision-making are thoroughly discussed, and a systematic treatment algorithm is presented.
Keywords
frontal sinus, frontal sinus fractures, frontal bone, coronal incision, cranialization, frontal sinus obliteration, endoscopic approach
Background
The frontal sinus is protected by thick cortical bone. High-velocity impacts can result in frontal sinus fracture and brain injury. These complex injuries pose many surgical challenges and can be associated with long-term sequelae such as mucocele and meningitis. Optimal management strategies remain controversial. Treatment goals should include protection of the intracranial contents, avoidance of short- and long-term complications, restoration of an aesthetic frontal contour, and maintenance of sinus function when possible. A treatment algorithm is presented based on injury to three anatomic regions: the anterior table, the frontal recess, and the posterior table/dura.
Anatomy
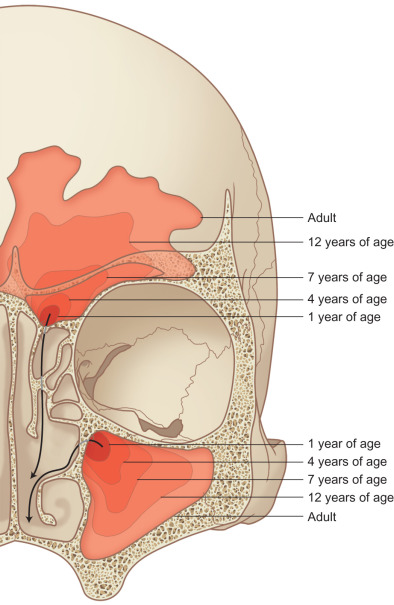
Although not present at birth, the frontal sinus aerates by extension of the ethmoid air cells into the frontal bone. This process usually begins at 2 years of age and the sinus is completely developed by about the age of 15 ( Fig. 1.7.1 ). The degree of frontal sinus development is variable, with up to 11% of people having only a unilateral frontal sinus and 4% of people having no frontal sinuses at all. The anterior table bone averages 4 mm in thickness; while the posterior table is thinner, providing less protection to the anterior cranial fossa ( Fig. 1.7.2 ). The intersinus septum often divides the frontal sinus into two sides, each of which drains into their respective frontal sinus outflow tract. The frontal sinus drainage pathway has an hourglass shape ( Fig. 1.7.3 ), with the infundibulum above, true ostia in the middle (1–3 mm), and frontal recess below.


Etiology and Incidence
Frontal sinus fractures comprise approximately 5%–15% of maxillofacial injuries. The force required to fracture the frontal bone is greater than for any other facial bone. Improvements in vehicle safety, such as seatbelts and airbags, have significantly decreased the incidence of frontal sinus fractures. The majority of patients are young males (average 30 years) who sustain high-velocity injuries such as: motor vehicle collisions (52%), interpersonal violence (26%), and recreation or industrial accidents (14%). One-third of these injuries are isolated anterior table fractures; two-thirds involve some combination of the anterior and posterior tables as well as the nasofrontal recess; while isolated posterior table fractures remain quite rare (<2%). The majority of patients (75%) who sustain frontal sinus injuries will have associated craniofacial fractures.
History and Physical Examination
Due to the high velocity nature of these injuries, the initial evaluation should focus on airway control and hemodynamic stability. A complete head and neck examination should rule out injury to the brain, spine, orbits, and facial skeleton; including the frontal sinus. Patients with frontal sinus fractures often complain of forehead pain and swelling. Physical findings may include paresthesias, epistaxis, diplopia, forehead abrasions, lacerations, and hematoma.
Fractures of the posterior table place patients at increased risk of dural tear, cerebrospinal fluid (CSF) rhinorrhea, and meningitis. The most common clinical presentation of CSF rhinorrhea is intermittent bloodstained, or clear watery anterior nasal discharge, salty postnasal drainage, and headache. If rhinorrhea is present, it can be evaluated with a “halo test,” whereby the fluid is allowed to drop onto filter paper. If CSF is present, it will diffuse faster than blood and result in a clear halo around the blood. A more definitive diagnosis can be made using a beta-2 transferrin assay. With its high sensitivity (99%) and specificity (97%), this biochemical assay is viewed as the gold standard for diagnosis of CSF rhinorrhea. Disadvantages of the test include: expense, labor-intensive fluid collection, and waiting period for results (approximately 3–5 days).
Radiography
The gold standard radiographic examination for traumatic injuries of the facial skeleton is a thin cut (≤1 mm) computed tomography (CT) scan. To help improve diagnostic accuracy, these images should be reformatted into coronal, sagittal, and 3-dimensional reconstructions. The axial images are preferred for evaluation of the anterior and posterior table ( Fig. 1.7.4 ); sagittal images for the frontal sinus outflow tract and skull base ( Fig. 1.7.5 ); and the coronal images for the orbital roof/sinus floor ( Fig. 1.7.6 ). Three-dimensional reconstructions ( Fig. 1.7.7 ) offer a comprehensive view of the injury. They are helpful to assist in surgical planning, facilitate patient education, and delineate the size/location of bone fragments, which can reduce the need for soft tissue dissection.




Surgical Approaches
The major surgical approaches to the frontal sinus include: laceration, trephination, percutaneous, endoscopic brow, direct forehead/suprabrow, upper blepharoplasty, endonasal sinusotomy, and coronal.
Lacerations
When lacerations are present, they should be used to assist with fracture visualization/reduction as well as hardware placement. While lacerations can be extended for greater access, caution should be used. This may result in more pronounced facial scaring and paresthesias. Small fractures can be treated through lacerations alone. But the actual exposure requirements necessary to complete the repair can only be assessed intraoperatively. Therefore, consent for other surgical approaches should always be obtained.
Trephination
Frontal sinus trephination is a technique that offers added visualization and access to the frontal sinus. A 1.0–1.5 cm curved skin incision midway between the medial canthus and glabella is made just inferior to the brow ( Fig. 1.7.8 ). Incisions within the brow itself are not recommended due to the risk of alopecia and injury to the supratrochlear/supraorbital neurovascular bundles. To reduce the risk of visible scar formation or webbing, a “V” can be inserted to break up the incision line. Careful dissection down to the frontal bone is performed with a guarded needle tip electrocautery. The frontal sinus location is confirmed with a CT scan or the use of intraoperative navigation. A small cutting bur is used to create a 4–5 mm frontal sinusotomy ( Fig. 1.7.9 ), the mucosa is opened, and a 30 degree endoscope is used to visualize the sinus. A Valsalva maneuver can be performed to better localize a CSF leak. If more lateral visualization is required, a flexible pediatric bronchoscope can be used.


Percutaneous
Several authors have described case reports or small case series of percutaneous fracture reduction for primary repair. This involves stab incisions to visualize the bone segments, and percutaneous screws for fracture reduction.
Endoscopic Brow
Endoscopic brow approaches, while developed for brow-lifting procedures, have been adapted for primary and secondary repair of anterior table frontal bone fractures. Using brow-lift instrumentation, a 3–5-cm parasagittal “working” incision ( Fig. 1.7.10 ) is placed 3 cm posterior to the hairline directly above the fracture. Limited use of electrocautery will reduce the risk of alopecia. The incision is taken down to bone and a brow-lift elevator is used for subperiosteal dissection to the level of the fracture. Through a second 1–2-cm “endoscope” incision (placed approximately 6 cm medial to the working incision), a 4 mm 30 degree endoscope within a rigid endosheath is introduced for visualization. A large guard on the endosheath will help with tissue elevation and maintenance of the optical cavity. Careful subperiosteal dissection ( Fig. 1.7.11 ) is performed over the fracture deformity under endoscopic visualization, with care to identify and preserve the supraorbital and supratrochlear neurovascular bundles.


Direct Forehead/Suprabrow
Large lacerations can provide adequate access for open reduction and internal fixation of some fractures. Significant extension of such lacerations should be avoided for aesthetic reasons. However, a direct approach, whereby an incision is placed within a horizontal rhytid over the fracture, is effective in patients with deep rhytids. Direct transcutaneous supra- and infrabrow incisions have also been described. Paresthesias related to these approaches resolve in most patients, however the authors believe that incisions placed directly above the brow have a higher risk of long-term paresthesias and visible scarring.
Upper Blepharoplasty
An upper blepharoplasty incision will allow access to fractures of the superior orbital rim and inferior frontal bone. This approach has been cited more commonly for sinus surgery, CSF leak repair, skull base surgery, and orbital roof fractures. An incision is placed in the supratarsal crease at least 10–12 mm above the eyelid margin. It can be extended from the supraorbital notch to just outside the lateral canthus as necessary for access. The incision is initially carried through the skin and orbicularis oculi muscle, allowing identification of the orbital septum. The orbital septum should not be violated, as this will expose orbital fat and the levator palpebrae superioris. At this point, upward traction can be applied to the brow, transposing the incision over the bony orbital rim. An electrocautery with a microtip needle (on a low setting) is then used to dissect directly onto the frontal bone. Once the rim is palpated, the electrocautery can be used to incise the periosteum and expose the frontal bone in a subperiosteal plane.
Endonasal Sinusotomy
A transnasal endoscopic frontal sinusotomy (or Draf III procedure) is commonly used for management of chronic frontal sinusitis, mucoceles, frontal sinus trauma, and frontal sinus tumors. It provides access to the frontal recess as well as the anterior and posterior table of the frontal sinus. The procedure begins with an endoscopic ethmoidectomy and identification of the ethmoid skull base and lamina papyracea ( Fig. 1.7.12A ). Utilizing angled endoscopes (30, 45, or 70 degree depending on surgeon preference) and through cutting instrumentation, the floor, posterior wall, and roof of the agger nasi cell are removed. The frontal recess has now been dissected and an endoscopic view of the frontal sinus is achieved. The same procedure is then performed on the contralateral side until the bilateral frontal sinus ostia are visible. A 2 × 2 cm superior septectomy is then performed to gain bilateral access to the floor of the frontal sinus ( Fig. 1.7.12B ). The posterior limit of this window should align with the anterior aspect of the middle turbinate. The septal window is lowered until the opposite frontal recess and upper half of the opposing middle turbinate is visible. The septal mucosa is harvested and preserved as it may later be used for mucosal grafting of the exposed bone of the frontal beak. Utilizing a high-speed, angled 4 mm diamond bur, the bone of the septum is removed to identify the floor of the frontal sinus ( Fig. 1.7.12C ). The posterior limit of this dissection is the first olfactory neuron. The axilla of the middle turbinate (i.e., frontal process of the maxilla) is demucosalized and drilling proceeds from lateral to medial, removing the bone of the axilla and identifying the periosteum of the underlying skin ( Fig. 1.7.12D ). This marks the lateral limit of the dissection. The floor of the frontal sinus is then removed to create a large horseshoe-shaped neostium. The nasofrontal beak is thinned utilizing a 70 degree bur and 30 degree endoscope. The frontal intersinus septum is partially removed to create a median drainage pathway for the frontal sinus ( Fig. 1.7.12E ). The exposed bone of the frontal beak may be left bare, dressed with Silastic sheeting, or grafted with septal mucosa harvested from the creation of the septal window.





Coronal Incision
The coronal incision is still considered the “gold standard” for management of significant frontal sinus injuries. However, as less invasive approaches are adopted, it is less commonly used. The approach provides uncompromised access to the anterior table, frontal recess, posterior table, and anterior cranial fossa. The coronal approach can be used for primary fracture repair, as well as treatment of secondary deformities. Unfortunately, it carries a significant risk of iatrogenic sequelae such as alopecia, paresthesias, facial nerve injury, and visible scarring. Therefore this approach is usually reserved for complex injuries requiring open manipulation and hardware application.
The coronal incision is marked out at least 4–6 cm behind the hairline. The hair can be banded and need not be shaved. The incision may be a peaked line ( Fig. 1.7.13 ) or “zig-zag” ( Fig. 1.7.14 ). The zig-zag incision assists with scar camouflage; taking advantage of the hair’s inferior alignment which covers the transverse arms of the scar. The scalp is opened in thirds to minimize blood loss. Hemostasis during the initial scalp incision is addressed with limited use of bipolar cautery (minimizing damage to hair follicles), local sutures, or hemostatic clips according to surgeon preference.



An intimate knowledge of the temporal anatomy is required to preserve the temporal branch of the facial nerve, minimize alopecia, and reduce the risk of temporal hollowing ( Fig. 1.7.15 ). If use of the pericranial flap is not required, the pericranium can be incised and elevated along with the scalp in a subperiosteal plane. If a pericranial flap is needed for dural repair or frontal sinus obliteration, the scalp is elevated first; leaving the pericranium on the bone. The pericranium is then elevated as a separate vascularized flap ( Fig. 1.7.16 ). Inferior dissection should identify and preserve the supraorbital and supratrochlear neurovascular pedicles ( Fig. 1.7.17 ). These pedicles may exit from a notch in two-thirds of cases or a foramen in one-third of cases. True foramina can be outfractured with a 2 mm osteotome to free the contents of the foramen and gain access to the orbital roof and medial wall ( Fig. 1.7.18 ).




Laterally, the dissection continues below the temporal line, leaving the temporalis muscle fascia (deep temporal fascia) intact. The temporoparietal fascia is carefully elevated to preserve the temporal branch of the facial nerve ( Fig. 1.7.15 ). If the zygomatic arch requires exposure, the superficial layer of the temporalis muscle fascia is incised approximately 2 cm above the arch and the dissection continues between the fascia and the superficial temporal fat pad. This is a dense dissection plane that does not elevate easily. Once the zygomatic arch is exposed, the periosteum is incised on the upper border (to protect the temporal branch of the facial nerve) and a periosteal elevator is used to expose the bony arch.
After fracture repair, the closure is performed in layers, suturing and re-suspending the temporal soft tissue layers to prevent postoperative ptosis. The galea aponeurosis is realigned with absorbable suture and the skin is carefully closed with atraumatic technique to prevent alopecia. Drains and a pressure dressing can be used according to surgeon preference.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







