Abstract
Flaps are often the ideal closure for skin wounds when a simple primary closure is not possible. After perfection of suturing and surgical technique, the ability to choose the ideal flap comes from a thorough understanding of the fundamentals of flaps and especially the tissue movement dynamics for each flap subgroup. There are four basic flap types including the Burow’s triangle displacement flaps, the defect reconfiguration flaps, the tissue reorientation flaps, and the tissue importation flaps. Each group offers a unique solution to tissue defects when simple side-to-side closures are not feasible. A cookbook approach to choosing flaps based on anatomic locations or other characteristics of defects is suboptimal. Each defect should be individually considered from all aspects and then selection of the most suitable flap is made with a conscious effort to address all reconstructive challenges. These include the size and depth of the defect, the functional considerations of the wound site, the aesthetic features, the nearby anatomic borders, and the patients’ age and their expectations. Foremost of these considerations is the functional aesthetics of the closure. Not all aesthetic closures are functional, but functional reconstructions are often aesthetic.
Keywords
flaps, reconstruction, tissue dynamics, Burow’s triangle displacement flaps, defect reconfiguration flaps, tissue reorientation flaps, tissue importation flaps
- ▪
A cookbook approach to flap reconstruction is not realistic
- ▪
The mnemonic STARTS lists basic reconstruction options: simple side-to-side closures, transposition flaps, advancement flaps, rotation flaps, tissue importation flaps, and skin grafts
- ▪
Understanding the dynamics of a flap optimizes its execution
- ▪
For reconstruction, the simplest approach that achieves the desired result is often best
- ▪
Extensive undermining, everted wound edges, meticulous hemostasis without excessive electrocoagulation, and technical precision are important in achieving an outstanding result
Introduction
Cutaneous reconstruction has played an important role in the establishment of dermatologic surgery as a vital discipline within dermatology. An in-depth understanding of reconstructive techniques, combined with a dermatologist’s intimate familiarity with skin, enables optimal aesthetic and functional results. Equally important is an in-depth understanding of the tissue dynamics of flaps, why they work, what problems each flap type can address, and their limitations. A cookbook approach to flap reconstruction is not realistic because of the many variables relating to the characteristics of the defect, the donor skin, the patient, and the surgeon. It is better to develop a foundation of basic concepts from which the individual can build his or her skills and unique style for reconstruction.
Background
At the patient’s side, it is always helpful to have an on-demand recall of flap options. With experience, this is automatic, but those with less experience may find the mnemonic STARTS helpful ( Table 147.1 ). It is incumbent upon the surgeon to synthesize the many factors that may affect the choice of the most appropriate flap for a defect. The characteristics of the wound, qualities of the adjacent skin, the functional aspects of the affected anatomic site, the pertinent aesthetic considerations, the anatomic borders in proximity to the defect, and the age and expectations of the patient all contribute to deciding the most appropriate reconstruction.
| STARTS MNEMONIC |
|
The most important goal in reconstruction is functional aesthetics. This means that the reconstruction should first and foremost maintain all vital functions and accomplish this aesthetically. Not all aesthetic reconstructions are functional, but all functional reconstructions can be aesthetic.
Fundamentals of Flap Design and Suturing Technique
Technical precision, including suturing technique, may be the most important variable in achieving an outstanding result. The first important step is to prepare the wound edges of both the defect and the flap. All incisions should be made at a 90° angle to the skin surface such that the wall of the defect and the edge of the flap are square. Secondly, the wound base should be made a uniform depth. Whether reconstructing with an elliptical side-to-side closure or with any of the more intricate flaps, the contour of the wound base will persist and may affect the long-term appearance of the wound. Likewise, the thickness of the flap should be uniform. Although the optimal plane of flap dissection is somewhere between the upper mid subcutaneous and deep subcutaneous tissue, the ideal thickness of a flap varies and must be determined on a case-by-case basis. Flaps constructed too thinly can develop vascular compromise or may lead to an unnatural appearance. Conversely, a very thick flap may be bulky, have decreased mobility, or be more difficult to manipulate while suturing, and it may unintentionally damage underlying neurovascular structures or muscles. Hair-bearing skin mandates attention to the level of the follicle.
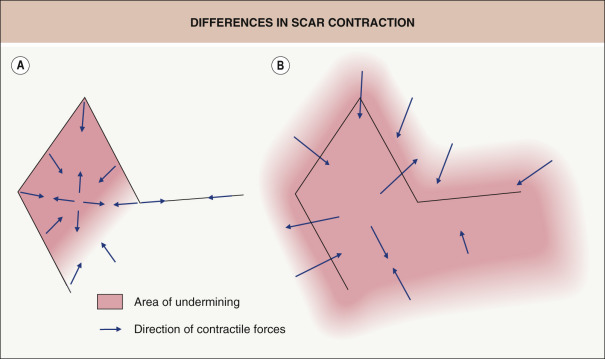
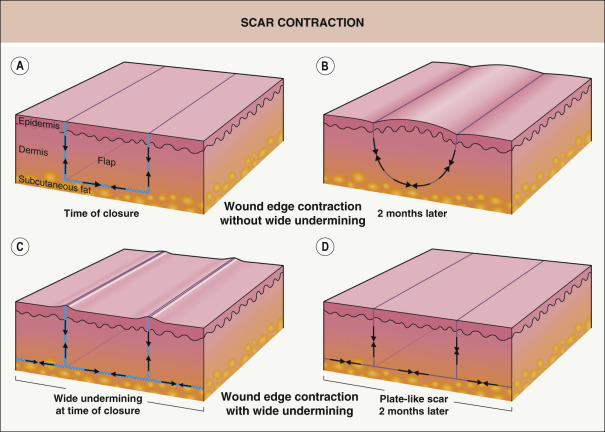
Widespread undermining of the subcutaneous tissue adjacent to both the defect and the donor site defect is important for creating a broad “plate-like scar”. This results in an even distribution of scar contraction over a greater area and diffuses the effects of contraction such that it is not focused on the flap itself or the incision lines of the flap ( Fig. 147.1 ). Undermining should be uniform and complete, including the areas of low tissue tension such as the tips of an ellipse or the pivot points of flaps .
Next, meticulous pinpoint hemostasis with complete visualization of all undermined skin with the help of an assistant is critical. Excessive postoperative bleeding within a sutured wound often results in an inferior outcome. It should be emphasized, however, that extensive tissue injury caused by electrosurgical hemostasis should be avoided as fervently as postoperative bleeding, since this can contribute equally to unwanted results. With a well-prepared wound and flap that are characterized by uniformity in thickness, sharply squared edges, well-loosened tissue margins and excellent hemostasis, the wound is ready for suturing.
An adequately undermined flap may still lead to distortion of delicate structures if the flap is large, heavy, or moves under considerable tension. A flap suspension suture may be necessary in order to avoid distortion or displacement of delicate tissue. These sutures are placed in fixed or rigid structures underlying the flap. Periosteal sutures represent a common anchoring technique and they are placed from the periosteum through the undersurface of the flap into the deep dermis . When this suture is placed in the undersurface of the flap, it should correspond topographically to its desired location relative to the periosteal suture. More than one suspension suture may be needed and should be placed in a direction parallel to the flap blood supply to avoid vascular compromise of the flap.
Whether it is a side-to-side closure or a flap, eversion of the skin edges (along with undermining) is also essential ( Fig. 147.2 ). Given their longer period of effectiveness, as compared to epidermal sutures, the author prefers the use of subcutaneous (“buried”) vertical mattress sutures to achieve eversion (see Ch. 146 ) .
Flap Movement Characteristics
It is helpful to broadly characterize flap types according to their mechanism of skin movement and rearrangement. By understanding the dynamics of each flap, it is easier to select one that will provide functionally aesthetic results. Upon consideration of the unique characteristics of the defect, the donor skin, and the functional and aesthetic issues of reconstruction in the context of the mechanics of flap tissue movement, a rational decision regarding the method of closure can be made. The components that flaps share include the flap body, the pedicle or vascular base, primary and secondary defects, and, as an integral part of flap dynamics, the primary and secondary movements ( Table 147.2 , Fig. 147.3 ) .
| DEFINITIONS OF FLAP COMPONENTS | |
|---|---|
| Body | The skin being advanced, transposed, rotated, interpolated or imported into the primary defect |
| Pedicle | Also known as the vascular base of the flap, it is the conduit of the vascular supply that will remain intact and maintain the vascularization of the body of the flap intraoperatively and for the early postoperative period |
| Primary defect | The area deficient in skin that will be reconstructed by the movement of the body of the flap |
| Secondary defect (donor site defect) | The area devoid of skin created by the movement of the body of the flap |
| Primary flap movement | The movement of the flap body into the defect |
| Secondary flap movement | The tissue movement necessary to close the void or donor site defect created by the movement of the body of the flap |
| Primary tension vector | The direction of the force tending to counteract the movement of the body of the flap |
| Secondary tension vector | The direction of the force created by the closure of the donor site defect |

Most tissue movement results in some degree of tension. This tension creates vectors of force that tend to return moving skin back to its original position. Therefore, the primary movement of a flap creates a primary tension vector, while the secondary movement (during closure of the donor site defect) creates a secondary tension vector. Consideration of these forces and the effects of these forces on adjacent tissue and even the blood supply of the flap is the primary factor in selecting one flap over another . The most perfectly executed flap that, via tension vectors, results in the distortion of a free margin (e.g. a lip or eyelid) is of little value to the patient or the goal of aesthetic restoration. Therefore, the initial and most important skill required for the proper execution of flaps is the ability to anticipate the direction and amount of tension created by particular flaps and to predict what effects this tension will have on adjacent structures. Secondarily, judicious use of tension sutures is helpful.
There are four broad categories of flaps based upon how the tissue is rearranged in order to achieve closure ( Table 147.3 ). In the first category, one or both Burow’s triangles that would be removed if the wound were closed by a simple side-to-side closure are displaced. The second includes the flaps that reconfigure defects, while the third includes flaps that reorient tissue from adjacent pools of laxity into the defect. Finally, there is a category of flaps that enables defect closure by tissue importation.
| CLASSIFICATION OF FLAPS BASED ON DESIGN CHARACTERISTICS | |||||
|---|---|---|---|---|---|
| Flap category | Flap variations | Synonyms | Mechanism of tissue movement | Advantages | Disadvantages |
| Burow’s triangle displacement flaps | Single tangent adv flap | Burow’s flap |
|
|
|
| Bilateral single tangent adv flap | A-to-T flap, O-to-T flap | ||||
| Double tangent adv flap | U-flap | ||||
| Bilateral double tangent adv flap | H-flap | ||||
| Curvilinear tangent adv flap | Rotation flap, Karapandzic flap, Mustarde flap | ||||
| Defect reconfiguration flaps | Island pedicle flap | Kite flap, myocutaneous pedicle flap |
|
|
|
| Tissue reorientation flaps | Rhombic transposition flap | Limberg flap, Dufourmentel flap, Webster’s 30° flap |
|
|
|
| Bilobed transposition flap | |||||
| Nasolabial transposition flap | Melolabial fold flap | ||||
| Nasolabial flap with a twist (Spear’s flap) | |||||
| Tissue importation flaps | Forehead flap | Indian flap |
|
|
|
| Nasolabial interpolation flap | Melolabial interpolation flap | ||||
| Retroauricular pedicled flap | Pin back flap | ||||
| Modified Hughes flap Abbe cross-lip flap | |||||
Burow’s triangle displacement flaps
Flaps that displace Burow’s triangles to a “convenient” location distant from the defect include the single tangent advancement flap (Burow’s flap), the bilateral single tangent advancement flap (A-to-T flap), the double tangent advancement flap (U-flap), the bilateral double tangent advancement flap (H-flap), and rotation flaps (e.g. the dorsal nasal or Rigor flap, Mustarde flap, helical advancement flap) ( Fig. 147.4 ). These flaps displace Burow’s triangles along straight or curved incision(s) tangential to the wound .
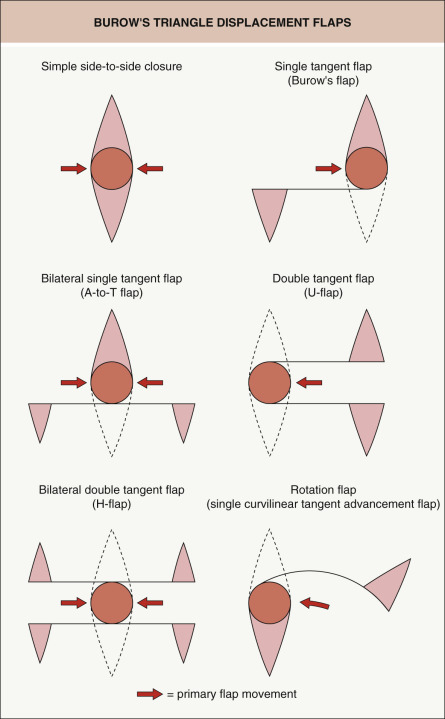
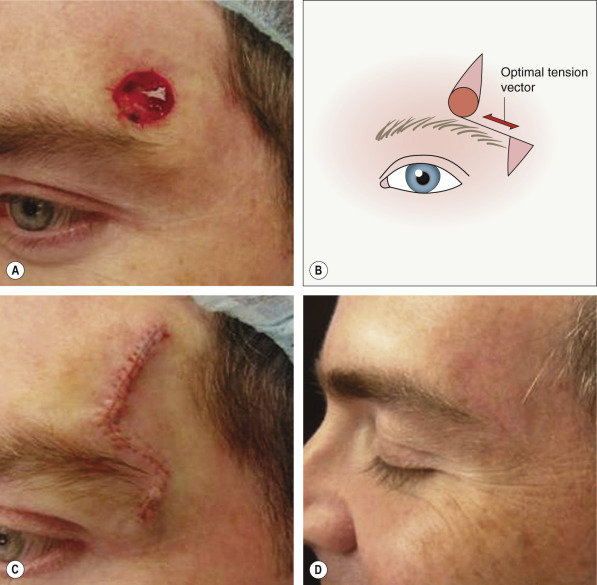
The key features of these flaps are: (1) they displace Burow’s triangles to a distant site; (2) there is limited reorientation of tissue; and (3) their movement is dependent upon the intrinsic elasticity of the skin. Just as a simple side-to-side closure performed in stiff, inelastic skin would result in a tense closure, so would a Burow’s triangle displacement-type flap. When the surrounding skin is elastic and “loose”, the wound edges can be closed under minimal tension in both a side-to-side closure and with these flaps. Thus, the only advantage that these flaps confer over a side-to-side closure in tight skin is that a larger area of skin is typically undermined, which releases the flap from the tethering effect of the subcutaneous tissue. This allows for a modest decrease in wound closure tension. The primary utility of these flaps is in defects where, for functional or aesthetic reasons, it is inconvenient to remove a Burow’s triangle immediately adjacent to the defect. An example of this is a defect above or below the eye in which displacement of the Burow’s triangle is useful in order to avoid removing a triangle from the eyebrow or eyelid ( Fig. 147.5 ).
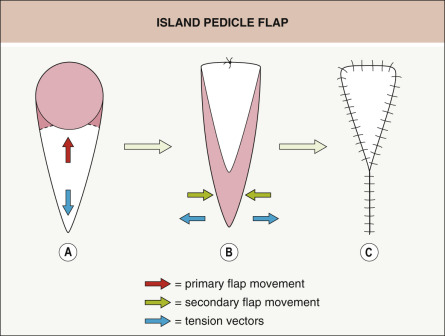
Defect reconfiguration flaps
The island pedicle advancement flap is unique in that it is an advancement of tissue oriented in a plane perpendicular to the skin and at 90° to the more traditional advancement or rotation flaps. In this case, the tissue redundancy created at the pivot point of the flap is buried in the subcutaneous plane at the advancing edge of the flap (see below). Fundamentally, an island pedicle flap reconfigures the typical roundish shape of the wound to a sharp, angled, geometric shape that is easily closed without standing cones or distortion of surrounding structures ( Fig. 147.6 ). Movement of this flap is entirely dependent on the elasticity of the tissue that comprises the flap.
Tissue reorientation flaps
Tissue reorientation flaps are characterized by the lifting of skin from an adjacent donor site and reorienting it through the transposition of the flap over a peninsula of skin between the donor site and the defect. There is a pivot point at the base of this flap (see Fig. 147.3 ). The tissue movement depends on the presence of laxity in adjacent tissue . Although intrinsic elasticity of the flap skin may facilitate the ease of execution, without ample laxity in the donor site, the transposition cannot be performed. Some of the flaps that fall into this category include the rhombic transposition flap, the bilobed transposition flap, and the nasolabial transposition flap (see Table 147.3 ).
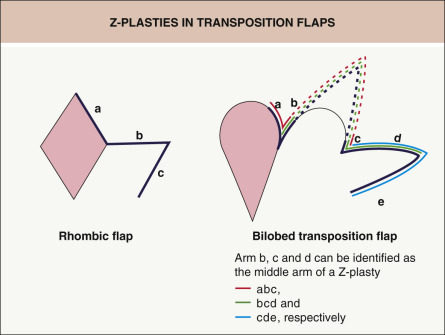
To better understand the reorientation of tissue that occurs in these flaps, a review of the most basic tissue reorientation flap, the Z-plasty, is helpful. Z-plasties transpose two angular flaps, placing them in a complementary fashion into the defects of the other flap ( Fig. 147.7 ). This reorientation of tissue ultimately results in the lengthening of the skin in the direction of the middle arm of the Z-plasty ( Fig. 147.8 ). There is a complementary decrease in the length of skin perpendicular to this same arm. The amount of lengthening is proportional to the angles of the flap(s). Put another way, tissue gain in the direction of the middle arm is proportional to the width of the base of the flaps. This is effectively the mechanism of tissue reorientation in transposition flaps. Upon careful examination, Z-plasties can be found within the design of transposition flaps ( Fig. 147.9 ). Therefore, just as with Z-plasties, transposition flaps work because the reorientation of the tissue results in lengthening of tissue in the direction of the skin deficit at the expense of the laxity in the donor site.
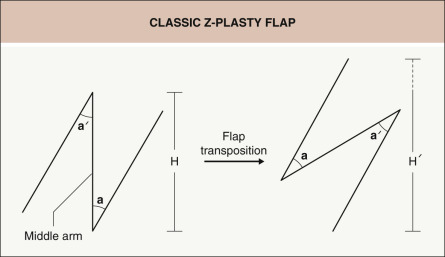

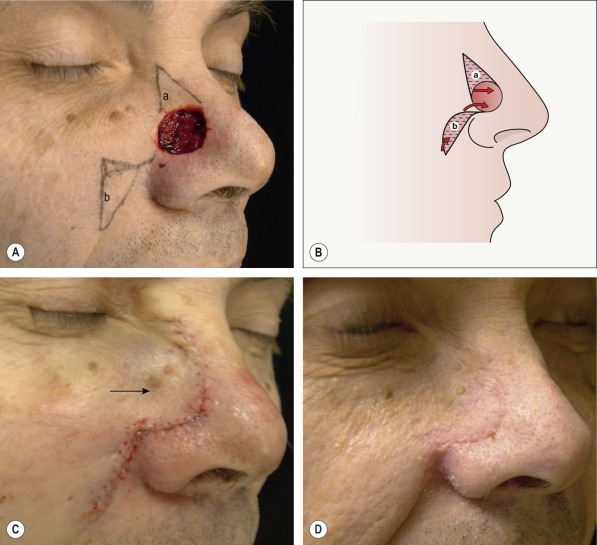
It is helpful to understand the utility of these principles of reorientation – an example of this would be a defect on the nasal tip ( Fig. 147.10 ). The skin is typically very tight in this area, making simple side-to-side closure in the vertical direction difficult. Side-to-side closure in the horizontal direction is impractical because of the distortion that would occur to the free margin of the ala. When one looks for donor sites, there is typically a substantial amount of laxity on the mid nasal dorsum and nasal sidewall. A bilobed flap allows utilization of this laxity through tissue reorientation using two lobes . The underlying mechanism of tissue reorientation is a series of Z-plasties inherent in this flap. Since tissue gain in Z-plasties is in the direction of the middle arm of the Z-plasty, a substantial reorientation and lengthening of tissue in the desirable direction for repair of the defect occurs without distortion . In contrast to the Burow’s triangle displacement flap, this flap does not rely upon intrinsic elasticity of the flap skin. This is key to avoiding distortion of the alar rim.

Tissue importation flaps
Large defects, or defects in areas where tissue laxity is lacking, may be reconstructed by importing vascularized skin from a site that is not adjacent to the defect (see Table 147.3 ) . Tissue importation flaps are typically derived from a distant donor site with ample tissue laxity and, most importantly, an excellent blood supply. This blood supply may be based on a particular artery (e.g. paramedian forehead flap based on the supratrochlear artery) or by a rich, random-patterned blood supply (e.g. the retroauricular pedicled flap).
These flaps are typically two-staged flaps requiring a period of vascular ingrowth from the wound bed of the defect. This time period ranges from 2 to 6 weeks, with 3 weeks being the most commonly reported time point for transection of the pedicle. In the head and neck region, defect sites where tissue importation flaps are commonly employed include the nose, ear, eyelid, and lip.
There are also single-staged tissue importation flaps. These are tunneling flaps in which skin from a non-adjacent site with a subcutaneous and muscular pedicle is passed through a “tunnel” to the defect site. The pedicle lies within the tunnel providing blood supply to the flap.
The appropriate selection and execution of these four broad flap categories are discussed in more detail below.
Description of Technique
Burow’s Triangle Displacement Flaps
Single tangent advancement flaps (STAFs) and rotation flaps
There are several variants of Burow’s triangle displacement flaps that are differentiated by the number of Burow’s triangle displacements, or the configuration of the tangential line extending to the displaced triangle (see Fig. 147.4 ). Ideally, the design of these flaps should, when possible, place surgical scars at cosmetic subunit borders and within relaxed skin tension lines. Therefore, when a defect is located near an arcing junction of a cosmetic subunit or if the relaxed skin tension lines are curved such as on the cheek ( Fig. 147.11 ), then the Burow’s triangle displacement flap, classically known as the rotation flap, may be an excellent option . On the other hand, when the cosmetic subunit junctions or relaxed skin tension lines are relatively straight, the STAF, or “Burow’s advancement flap”, may be optimal. A variation, the crescentic advancement flap, can be employed when the anatomic structures are naturally curved ( Fig. 147.12 ).

Once the need to displace a Burow’s triangle in order to avoid a vital structure is established, the incision lines should be planned in the optimal location. The incision, whether straight or arced, should extend to the point of preferred triangle displacement. The triangle should then be excised, commensurate in depth to the thickness of the flap. After undermining and hemostasis, the first point of suturing is the closure of the displaced Burow’s triangle. The second point of suturing is then the closure of the other Burow’s triangle. The remainder of the flap can then be completely sutured into the defect with even distribution of the remaining edges of the flap to the defect’s wound edges.
Double tangent advancement flaps (DTAFs)
DTAFs displace both Burow’s triangles along parallel tangents (see Fig. 147.4 ). Therefore, these flaps are typically peninsular in configuration with an isolated vascular base at the distal ends of the tangents. The execution of this flap is very similar to that of an STAF, except that one must be mindful of the more limited vascular supply ( Fig. 147.13 ). This isolated vascular supply necessitates limiting the length of the flap to three to four times its width. As with other advancement flaps, the first closure points are at the site of the displaced Burow’s triangles. Suturing the advancing flap with even distribution of the flap along the recipient tissue margins completes the execution of this flap .

Site-Specific Variations of Burow’s Triangle Displacement Flaps
Helical advancement flaps
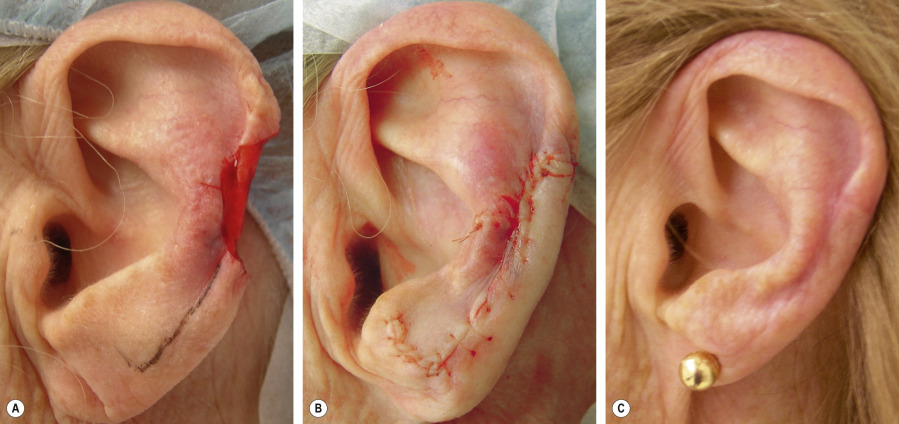
Helical advancement flaps are often discussed as a unique entity, but they are merely variants of Burow’s triangle displacement flaps. The characteristics of the helix are unique owing to its highly distortable free margin that is curved in nearly every dimension and its limited pool of adjacent tissue laxity . The common variant of the helical advancement flap is directly analogous to the DTAF in that parallel tangents are incised from the helical defect along the anterior rim of the helix and the posterior helix. Another variant is an STAF in which a single incision is made along the anterior helical rim while a non-displaced Burow’s triangle is excised directly posterior to the defect onto the posterior ear. Both the DTAF variant and this STAF variant can be either a single flap (derived superior or inferior to the defect) or two flaps (derived both above and below the defect). As with all Burow’s triangle displacement flaps, the helical advancement flap displaces the Burow’s triangle to a more convenient location. The majority of these flaps derive donor skin inferiorly. The donor pool from the superior helix is typically less abundant but can be very beneficial, both in large mid-helical defects when two flaps are used and in defects of the superior helix .
A common use of the helical advancement flap is for a small- to medium-sized defect on the mid helix not involving the cartilage ( Fig. 147.14 ). While a wedge closure of the ear could be considered, displacing the anterior triangle by utilizing the lax skin of the lower helix and earlobe obviates the need to do a wedge resection of the auricular cartilage and avoids disruption of its delicate architecture. Burow’s triangles can easily be displaced to the earlobe, which facilitates the advancement of the helical skin into the defect. Despite the resultant decrease in the size of the earlobe, the aesthetic impact tends to be minimal as long as the anterior profile of the ear is maintained. Since the earlobe is most visible on the lateral view and because the opposite earlobe is not simultaneously visible, subtle changes in size often go unnoticed.