Injectable tissue replacement and regeneration (ITR 2 ) is a standardized fat grafting technique, which anatomically addresses losses of facial volume, laxity, and sun damage of the skin resulting from the natural processes of aging. Based on the structural differences of fat existing in the deeper versus the superficial fat compartments of the face, while accounting for skeletal losses and skin aging, ITR 2 utilizes 3 sizes of fat grafts—millifat (parcel size 2.0–2.5 mm), microfat (1.0 mm), and nanofat (<500 μm)—to replicate characteristics of fat cells lost with facial decay and provide increased blood supply and improvements in aging skin.
Key points
- •
Injectable Tissue Replacement and Regeneration (ITR 2 ) is a standardized fat grafting technique, which anatomically addresses losses of facial volume, laxity, and sun damage of the skin.
- •
Anatomic components of volume loss are diagnosed through evaluation of facial surface topography and used to formulate unique, individualized treatment plans.
- •
Three sizes of fat grafts, millifat, microfat, and nanofat, are used to structurally replace losses in facial fat occurring at different depths and anatomic regions in the face.
- •
Regenerative effects of ITR 2 fat grafts often are augmented with regenerative cells obtained via mechanical fragmentation or through addition of stromal vascular fraction cell enrichment, platelet-rich plasma, and topical nanofat biocrème application.
Video content accompanies this article at http://www.plasticsurgery.theclinics.com .
Introduction
Recent advances in understanding of facial aging have resulted in significant insights into facial soft tissue and bony volume loss. Lambros documented photometric changes that showed that soft tissue of the face deflates with aging. Kahn and Shaw and Mendelson and Wong documented how the facial skeleton loses broad surface areas of bone without corresponding shrinkage of the soft tissue envelope. Rohrich and Pessa clarified the anatomy of the superficial and deep fat compartments and recommended that fat be injected into specific deep fat compartments in the face because fat lies both above and below the facial musculature and ligaments. From the authors’ own cadaver observations, fat is more tightly clustered in the superficial compartments above the muscles and larger and more loosely organized in the deep compartments below the facial musculature.
Advances in genetics have provided a basis for measuring early interventions that have the potential to slow aging of cells, and the finding of stem cells and regenerative cells in fat introduced the possibility of regenerating aging tissues, which was shown by Rigotti et. al and supported by recent work by Cohen and others. There are almost no other therapies in aesthetics other than fat grafting, stromal vascular fraction (SVF)-enriched fat grafting, nanofat grafting, platelet-rich plasma (PRP), and growth factors, that have demonstrated neoangiogenesis and trophic effects to some degree in virtually all subjects.
When patients come in for a facial aging consultation, they are evaluated at that particular moment in time. Yet, aging is an evolution of interdependent processes taking place over a lifetime. Growth dominates human development during the first 2 decades of life followed by a continual and gradual decay of tissues until death. The anatomic and histologic changes due to aging are seen individually in the skin, fat compartments, and underlying bone as well as dynamically in the interdependent relationships between them. Facial aging can be anatomically and visually modeled from analysis of the topography of the face. The concept of injectable tissue replacement and regeneration (ITR 2 ) attempts to answer a fundamental question: Can a dynamic model be used to determine the specific losses in facial fat compartments and bone and replace and/or regenerate these tissues in a way that reduces and to some extent reverses the facial aging process?
The ITR 2 procedure is a new, standardized method of differential fat grafting, which
- 1.
Diagnoses the anatomic components of volume loss by evaluating the surface topography of the face
- 2.
Addresses specific anatomic losses of different tissues, including skin, facial fat in the deep and superficial compartments, and bone
- 3.
Replaces these anatomic losses of fat with 2 to 3 different sizes of autogenous fat grafts optimized in size for structural replacement for areas of bone and deep fat compartment losses, superficial fat compartment replacement, and dermal and epithelial replacement and/or regeneration
Regenerative effects of fat grafts may be augmented with regenerative cells obtained via mechanical fragmentation. For example, ITR 2 nanofat is primarily a matrix-rich product that is processed through microcutting of the aspirated adipose tissue using the Nanocube (Lipocube, London, United Kingdom) and contains matrix, adipocyte-derived stem cells, SVF cells and growth factors, PRP, and/or mechanically dissociated SVF. This combination of anatomic fat replacement is supplemented with a menu of regenerative ingredients can be tailored to patient-specific needs.
Preoperative evaluation and markings
The patient is marked with a white makeup pen while sitting in the upright position ( [CR] ). Scalp hair quality and/or loss are noted to determine if a restorative treatment a regenerative approach might be beneficial. The epidermal, dermal, and subcutaneous tissue thickness and the degree of bone recession in the glabella and along the supraorbital rims are noted in analyzing the upper third of the face. The degree of photodamage is noted. Deeper rhytids are noted for possible sharp-needle intradermal fat grafting (SNIF) technique. Temporal depression is associated with deep fat loss, whereas increased show of the temporal veins is associated with superficial fat loss. Often both are present. The upper and lower eyelids and periorbital region are inspected. Loss of fullness of the lateral brow, loss of convexity of the skin caudal to the eyebrow, and supratarsal fold depth are noted. In the inferior orbit, the rim is evaluated as is the prominence of the intraorbital fat.
The tear trough and lid cheek junction are evaluated. The position of the globe is noted from the vertex view to determine the degree of proptosis. The lid to pupil position is noted and the degree of senile enophthalmos is evaluated. In the middle third, the zygomatic arch and body are outlined in white. The superior arch corresponds with the inferior temporal region. The deep lateral and medial suborbicularis occuli fat (SOOF) are noted as is the deep medial fat compartment of the cheek. The degree of buccal hollowing is evaluated. The nose is assessed for any aesthetic deformity and/or aging and the degree of pyriform recession is noted. The lips are evaluated along with the peri-oral tissues and degree of thinning and rhytids. In the lower third, the marionette basin is evaluated as the chin and labiomental fold. Chin texture may be improved with nanofat microneedling and fractional laser with topical delivery of nanofat biocrème. The prejowl area just lateral to the mandibular retaining ligaments, if scalloped, is addressed as is the inferior border of the mandible and the gonial angle. Chin projection is evaluated, and the neck is inspected for degree of subcutaneous loss, deep and fine rhytids and severity of sun damage.
Surgical procedures
Preoperative Preparation and Anesthesia
Patients are given oral prophylactic antibiotics 1 day before the procedure, if planned under local anesthesia, or intravenously before the procedure. Patients are given their choice of anesthesia, but for ITR 2 , local or intravenous anesthesia and tumescent lipoharvest are used unless the patient is having other facial procedures. Patients are offered the possibility of undergoing a fixed focused ultrasound treatment, a week to a couple days before the procedure, for its potential release of endogenous angiogenic growth factors to prepare the recipient facial tissues.
Adipose Tissue Harvest
If only fat grafting is being performed, the surgery itself takes approximately 45 minutes to an hour (see [CR] ). Fat is harvested from any area of excess subcutaneous fat and/or areas of patient preference if sufficient fat is available. The patient is prepped and draped under sterile conditions. Harvest begins with a 14G needle puncture followed by infiltration of tumescent fluid (500 mL of Ringer lactate with 25 mg lidocaine and 1 vial of epinephrine [1:1000]). A 12-holed cannula, with openings measuring 2.5 mm in diameter (Marina Medical, Davie, Florida), is inserted into a slightly dilated 14G needle hole. Using a 60-mL syringe with a lock, fat is aspirated. Generally, 120 mL of fat is removed. These punctures are often allowed to close by secondary intention or by Dermabond (Ethicon, Bridgewater, New Jersey, US) wound adhesive.
Fat Processing
Once the fat is removed, the tumescent fluid is decanted, and the fat is rinsed with Ringer lactate to reduce blood contamination. Based on new research on fat preparation and degree of engraftment, filtration systems, such as Puregraft (Solana Beach, California), and centrifugation are probably not necessary and add to the cost. Simple washing, gravity separation, and decantation to remove the tumescent solution are necessary to process the fat. When cleaning is complete, a portion of millifat is set to the side to replenish deep fat compartment loss and facial bone recession. The remaining fat is transferred into 20-mL syringes and processed into microfat and nanofat using the Nanocube kit, which has a total of 4 ports whose functions are to resize fat using a special cutting technique (see [CR] ). Other systems that can process the various sizes of fat grafts can be used.
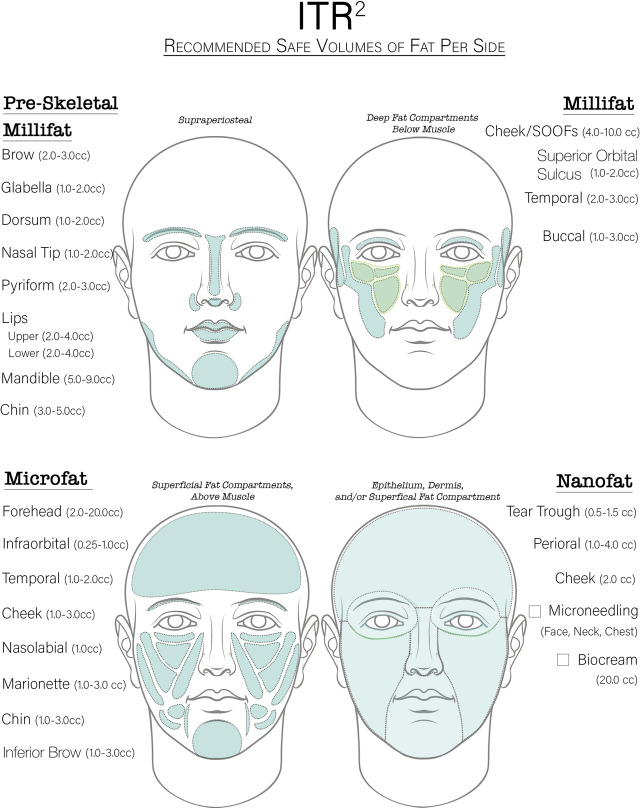
Delivery Techniques
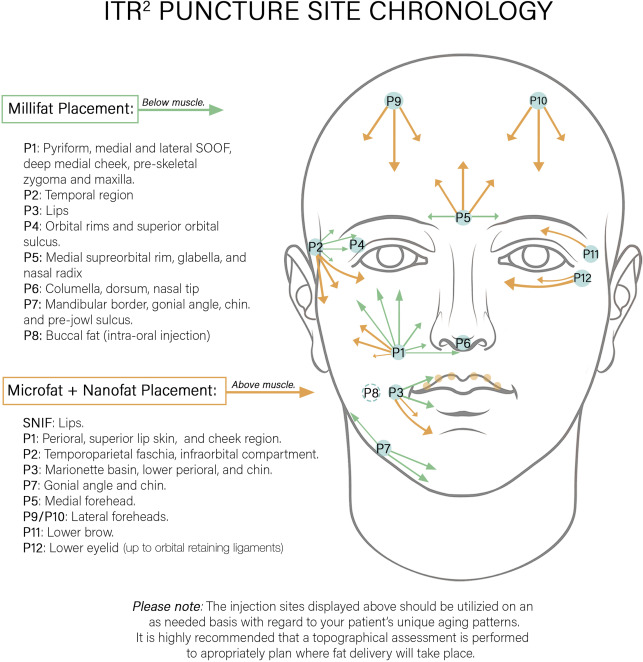
According to the topographic assessment, fat grafts are assigned to anatomic locations in the face according to their parcel sizes of millifat (2–2.5 mm), microfat (1 mm), and nanofat (500 μm and less) (see [CR] ). Placement starts with the deep compartments of the face and progresses superficially, using millifat first, then microfat, and ending with nanofat.
Up to 12 puncture sites are made with an 18G needle and are reused whenever possible in delivering the 3 sizes of fat grafts, shown in Fig. 1 . Safe volume recommendations and sites for fat grafting are shown in Fig. 2 .
Millifat (2–2.5 mm parcels)
Middle Third/Temporal Region
Millifat is first placed through an 18G needle puncture in the nasolabial fold lateral and superior to the oral commissure, into the areas of bone recession in the pyriform region. The cannula is then directed cephalad to graft the deep medial fat compartment and the medial then lateral SOOF. The deep temporal region is grafted along with the preperiosteal lateral supraorbital brow. The upper and lower hemilip are injected with millifat at the commissure.
Upper Third
The glabella, medial supraorbital rims, and nasal radix are injected through a needle puncture in the central glabella, approximately 1.5 cm to 2 cm above the nasofrontal junction. The nasal dorsum, tip, and columella are then grafted through an entry point between the domes of the nasal tip.
Lower Third
Attention is directed to the chin, mandibular border, and gonial angle. Modest retrogenia can be improved with millifat grafting. The area just lateral to the mandibular ligament and along the mandibular border is grafted in the preskeletal level through the same puncture. Millifat is placed along the inferior mandibular border and into the gonial angle to define the jawline, camouflage mild jowls, or lower an obtuse mandibular angle (see Fig. 1 , puncture site “7” [P7]).
If the buccal fat compartment shows volume loss, it is injected using an intraoral approach (see Fig. 1 , puncture site “8” [P8]). The patient is given intravenous clindamycin, and the intra-oral mucosa just below Stensen duct is prepped with betadine and then punctured with an 18G needle. It is important to place only small amounts of fat into the deep buccal compartment and reinspect the area frequently to determine if the proper amount is injected. It is important not to overfill this lowlight area.
Microfat (1-mm parcels)
Middle Third and Temporal Regions
For the perioral skin, microfat is grafted superficially above the muscle from the nasolabial needle incision for the upper lip and the oral commissure incision for the marionette basin and perioral tissue. The SNIF technique is used for the philtral columns (cupid’s bow) and rhytids perpendicular to the white roll of the upper and lower lips.
The superficial temporal fat compartment is grafted with microfat using the same temporal puncture site as the deep temporal compartment (see Fig. 1 , puncture site “2” [P2]).
Upper Third
For the forehead, the glabellar needle puncture site is used to inject superiorly and laterally into the medial brows (see Fig. 1 , puncture site “5” [P5]). Two more needle incisions are then placed at the hairline on either side at the midpupillary line to graft the corresponding central, inferior, and lateral forehead subcutaneous (superficial) fat compartment.
The incision for the upper lid sulcus and lower brow fat pad is located on the lateral superior orbital rim approximately 3 mm inferior to the tail of the eyebrow. For the lower eyelid, 2 access points are used: the tear trough point (see Fig. 1 , puncture site “11” [P11]) and a second point just lateral to the nasojugal groove (see Fig. 1 , puncture site “12” [P12]). Microfat placement is in the supraperiosteal, preseptal space.
Lower Third
The subcutaneous fat of the chin and jawline, including the lateral superior gonial angle as well as the submental crease, are grafted with microfat to restore a uniform silhouette of the lower face (see Fig. 1 , puncture site “7” [P7]).
Nanofat (500-μm parcels)
Nanofat is placed using either the SNIF approach, topically with microneedling or with a topical biocrème. Until 2017, the authors prepared nanofat in the gradual emulsification technique originally described. Since 2018, however, ITR 2 nanofat has been prepared using the Nancube. The advantage of the latter processing method is a matrix-rich product with less-traumatized regenerative cells. When delivered through an SNIF technique for dermal rhytids, this cellularly optimized nanofat is injected intradermally using a 25G cannula attached to a finger-activated grafting device, 3-mL Celbrush (Cytori, San Diego, California), or an automatic grafting device, Lipopen (Juvaplus, Neuchâtel, Switzerland).
Finally, nanofat is delivered with a mechanical microneedling device into the face, neck, and décolletage. A 5-mL to 20-mL aliquot of nanofat is kept to combine with a transdermal liposomal carrier to form a topical nanofat biocrème (neo-U [Aries Biomedical, San Diego]).
Postoperative care
Postoperative care consists of analgesia, nonsteroidal anti-inflammatory medications, and arnica for bruising. Direct application of ice is not permitted. Excessive swelling is treated as needed with a tapering oral steroid regimen. In patients undergoing facelift surgery or laser resurfacing, preoperative skin care is maintained with products containing matrikine (tripeptides and hexapeptides) ingredients exhibiting biologic functions, which modulate extracellular matrix repair and neocollagenases (Alastin Skincare, Carlsbad, California). In patients with a history of herpes simplex, perioperative prophylactic antivirals treatment is prescribed.
Patients can expect some bruising and swelling, with the lips swollen for approximately 5 days to 10 days. Patients can expect facial swelling and mild ecchymosis, which generally dissipate by day 3 to day 5, with 15% of patients taking longer, even a few weeks.
Expected outcome and management of complications
Patients having nanofat microneedling and/or nanofat biocrème (neo-U) in conjunction with fractional lasers of different wavelengths have experienced significant improvement in aesthetic outcomes with faster healing compared with historical controls that were not treated with nanofat. In patients having facelifts with ITR 2 , facial volume improves by approximately 45% at a month, drops to approximately 25% to 30% from 7 months to 12 months, and then improves to 74% at 18 months to 24 months. This finding suggests that there may be a reversal of tissue decay using ITR 2 in conjunction with facelift surgery.
Complications from ITR 2 have been rare and only related to excessive fat grafts in the lower eyelids. Although rare, transconjunctival or transcutaneous lower blepharoplasty with removal of fat has taken care of the problem. The authors no longer use microfat above the orbital retaining ligament, only matrix-rich nanofat. Since adopting ITR 2 , the authors have not experienced any overgrowth with patient weight gain.
Maintenance and subsequent procedures
Additional procedures are recommended based on a patient’s physical findings and individual aging patterns.
Case demonstrations
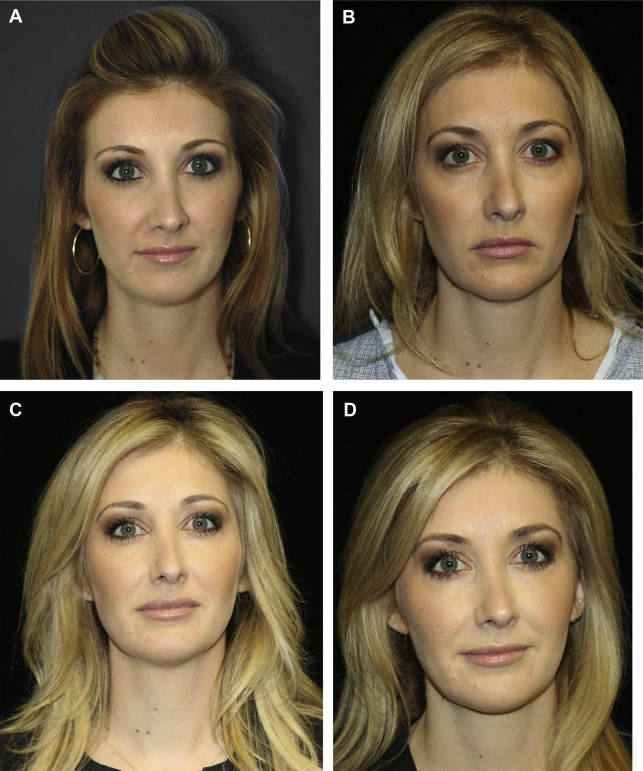
Patient 1
A 39-year-old woman demonstrates 6 years of aging ( Fig. 3 A, B ). In Fig. 3 C, she is shown 6 months post-ITR 2 and 2 years after ITR 2 ( Fig. 3 D). A total of 34 mL of fat was placed to the temporal, brows, cheeks, tear trough, nose, nasolabial folds, lips, and marionette lines. Note the gradual and subtle changes that occur with aging, the replacement of fat losses in the deep and superficial fat compartments, and her appearance after 8 years of aging.