Epidermal Nevi
Christina Stefanaki
Andreas Katsambas
Dimitrios Rigopoulos
Alexander Stratigos
BACKGROUND
Epidermal nevi (EN) are benign neoplasms comprised of cell types that reside in the epidermis, including keratinocytes, sebaceous glands, hair follicles, apocrine and eccrine glands, and smooth muscle cells. EN comprised primarily of keratinocytes are termed “keratinocytic,” whereas those composed of adnexal differentiation (sebaceous, follicular, or apocrine) are termed “organoid.” The incidence of EN has been reported to range from 1 to 3 per 1000 live births affecting males and females equally.1,2 The percentage of individuals with EN who have extracutaneous abnormalities is not precisely known. The most common extracutaneous associations involve the central nervous system (CNS), ocular, and skeletal systems.3
Keratinocytic epidermal nevi (KEN) are the most common form and include linear EN and linear verrucous EN.
Nevus sebaceous (NS) is relatively common, accounting for approximately one half of all EN.4
Inflammatory linear verrucous epidermal nevus (ILVEN) is a type of epidermal nevus and represents 6% of EN.3
Porokeratotic adnexal ostial nevus (PAON) was coined in 2009 to encompass porokeratotic eccrine ostial and dermal duct nevus, porokeratotic eccrine nevus, and porokeratotic eccrine and hair follicle nevus.5 PAON is rare entity and since the original description, there have been at least 25 reported cases.5
Papular epidermal nevus with “skyline” basal cell layer (PENS) is a newly recognized type of keratinocytic nevus.6
PRESENTATION
EN present as flesh-colored, pink, or lightly pigmented tan-to-brown papules or plaques.
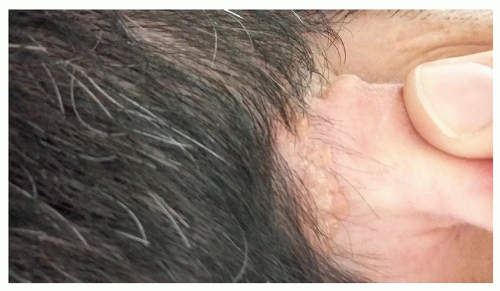
KEN are usually present at birth or during infancy. They are found on trunk and extremities and rarely on the head and neck. They often present as slightly papillated skin-colored to brown growths that follow a linear pattern (Figure 12.3.1).
Nevus sebaceus is always present at birth; however, it may not be noticed until later in childhood or until after puberty, when hormonal influences to sebaceous glands trigger thickening and the development of a papillomatous surface.
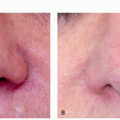
Nevus comedonicus (NC) presents at birth or during childhood with a linear array or clusters of dilated follicles containing keratin, resembling comedones (Figure 12.3.2).
 FIGURE 12.3.1 Keratinocytic epidermal nevus. These lesions may be flat initially, but they tend to become more elevated, verrucous, and darker over time. |
ILVEN usually presents in infancy or early childhood on the lower body as an intensely pruritic, unilateral array of linear erythematous and hyperkeratotic papules that often coalesce into plaques.4,7
PAON is found equally in boys and girls and majority of cases present at birth, occasionally as neonatal erosions, or soon after.5,8,9,10,11 Clinically, it presents as hyperkeratotic papules and plaques with comedo-like punctuate pits, often filled with keratin plugs.8
PENS lesions appear at birth as small, scattered, hyperkeratotic papules; they are rather round, oval, comma-shaped, or polygonal and do not follow the lines of Blaschko.6
Becker nevus (BN) appears between the first and second decade of life usually on the trunk or upper extremities as a solitary lesion that is typically hyperpigmented with hypertrichosis. This is usually categorized as a pigmented neoplasm even though it contains an epidermal hamartomatous component (see chapter 12.1iii).
DIAGNOSIS
Clinical Diagnosis
Keratinocytic Epidermal Nevi
KEN, often referred to as linear EN or linear verrucous EN or simply verrucous EN, are a common form of EN typically located on the trunk and extremities and very uncommonly to the head and neck area.1,4,5 KEN are usually present at birth or occur during infancy as skin-colored or pink-to-hyperpigmented, Blaschko-linear streaks and swirls, which may be unilateral or bilateral, usually stopping abruptly at the dorsal and ventral midline. Lesions can be localized or widespread in distribution, and when they are widespread, symmetric, and bilateral, they have been referred to as systematized EN or ichthyosis hystrix. The lesions initially may be flat and subtle, but they tend to become more elevated, verrucous, and dark over time (Figure 12.3.1).5 Acral lesions often have a more warty appearance and if the nail matrix is affected, the nail may be dystrophic, whereas in the body folds, lesions are softer and less verrucous.1,5 A special term has been used for localized lesions with a more warty appearance named nevus verrucosus.
Nevus Sebaceus
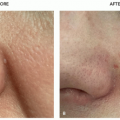
NS is always present at birth; however, it may not be noticed until later in childhood or until after puberty, when hormonal influences to sebaceous glands trigger thickening and the development of a papillomatous surface. Most NS are salmon to yellow colored and have a characteristic smooth waxy surface, which can be complicated by eczematous reactions (Figure 12.3.2).12 Most are located on the scalp or face, although they can be more widespread.5 If they are located on the scalp they are accompanied by alopecia. The size may vary from less than a centimeter to several centimeters in length, and a patient can rarely have multiple lesions.8 There are a few reports of unusually large and exophytic lesions, with histopathological picture consistent with nevus sebaceus.13,14
Nevus Comedonicus
NC is a developmental anomaly of the pilosebaceous unit that typically presents at birth or during childhood. Clinically, it is characterized by a linear array or clusters of dilated follicles containing keratin, resembling comedones (Figure 12.3.3). Usually the face, trunk, and upper extremity are affected, but lesions may rarely be found on the distal extremities, the scalp, or genitalia.15,16 Lesions are usually unilateral and if large they follow Blaschko lines; however, bilateral lesions have been reported, as well as extensive involvement of half the body.15,17,18 NC may be complicated by superinfection with bacteria, chronic inflammation, and scarring.15,19
Inflammatory Linear Verrucous Epidermal Nevus
It usually presents in infancy or early childhood on the lower body as an intensely pruritic, unilateral array of linear erythematous and hyperkeratotic papules that often coalesce into plaques (Figure 12.3.4).4,7 The lesion is characterized by intense pruritus and the prognosis is variable, often waxing and waning over time.8 ILVEN is often mimicking psoriasis; however, it is resistant to standard psoriasis treatments and may be difficult to distinguish from linear (nevoid) psoriasis.5
Porokeratotic Adnexal Ostial Nevus
PAON is found equally in boys and girls and the majority of cases present at birth, occasionally as neonatal erosions, or soon after.5,8,9,10,11 Clinically, it presents as hyperkeratotic papules and plaques with comedo-like punctuate pits, often filled with keratin plugs.8 Lesions
are usually located on the palms or soles in a linear pattern, but several cases have been reported with widespread unilateral or bilateral lesions distributed along Blaschko lines.10,20,21
are usually located on the palms or soles in a linear pattern, but several cases have been reported with widespread unilateral or bilateral lesions distributed along Blaschko lines.10,20,21
Papular Epidermal Nevus With “Skyline” Basal Cell Layer
PENS lesions appear at birth as small, scattered, hyperkeratotic papules; they are rather round, oval, comma shaped, or polygonal and do not follow the lines of Blaschko.6 They are found in many different areas of the body, but the palms and soles are spared.
Becker Nevus
BN mainly appears between the first and second decade of life, sometimes after sun exposure and is rarely described at birth22,23 (see also chapter 12.1.3). Lesions are typically located on the trunk or proximal upper extremities, but other parts of the body may also be involved, including the face24,25 and 12% of the lesions appear on the lower extremities.5,26 Most are solitary and unilateral, although multiple and bilateral BN have been reported.27,28 BN may appear as a single irregular macular hyperpigmentation or as multiple hyperpigmented macules arranged in a checkerboard pattern.29 Hypertrichosis within the lesion is common, but not universal.8 Three varieties of BN have been recognized by Parizzon et al30 according to clinical presentation: melanotic (39%), hypertrichotic (19%), and mixed types (42%). The melanotic type is characterized by only hyperpigmentation, without hair or with only vellus hair and in some cases is difficult to differentiate from a large pale congenital nevus or a giant café au lait macule. The prevalence of BN has been estimated between 0.25% to 2.1%, and males are affected predominately, but the exact male to female ratio is unknown.8,31 When stroked or rubbed, BN become more elevated and appear more infiltrated (pseudo-Darier sign), secondary to piloerection of the hairs within the nevus.5
On dermoscopy features commonly recognized are the presence of a network, hair follicles, and vessels, with focal, skin furrow, and perifollicular hypopigmentation.29
Histopathology
Keratinocytic (Verrucous) Epidermal Nevi
Histologically, keratinocytic, or verrucous EN are characterized by acanthosis, orthohyperkeratosis, papillomatosis, and an expanded papillary dermis, which is sharply demarcated from the surrounding normal skin. Epidermolytic hyperkeratosis, seborrheic keratosis-like features, psoriasiform hyperplasia, verruca-like and porokeratosis-like features, and Darier disease-like and acanthosis nigricans-like changes are seen in a minority of cases.32 The epidermolytic variant may appear clinically as keratotic plaques that are softer and lighter than those of other KEN.5 Epidermolytic KEN are caused by mutations in keratins 1 and 10, which when present in the germline cause epidermolytic ichthyosis, so more appropriately they should be categorized as localized or mosaic forms of ichthyosis.5,33 Patients with cutaneous EN revealing epidermolytic hyperkeratosis histology may transmit this gene to their offspring with widespread cutaneous involvement.33
Nevus Sebaceus
The histopathological features of NS change with age, as do the clinical features. Before puberty, the presence of incompletely differentiated hair structures may suggest the diagnosis, but after puberty, large numbers of
mature sebaceous glands in addition to papillomatous hyperplasia of the overlying epidermis are diagnostic.5,34 Sebaceous glands may be located high in the dermis, unrelated to a hair follicles, sometimes communicating directly with the epidermis.8,35 Hair follicles are decreased, absent, or immature and ectopic apocrine glands may be present in the lower dermis.35,36
mature sebaceous glands in addition to papillomatous hyperplasia of the overlying epidermis are diagnostic.5,34 Sebaceous glands may be located high in the dermis, unrelated to a hair follicles, sometimes communicating directly with the epidermis.8,35 Hair follicles are decreased, absent, or immature and ectopic apocrine glands may be present in the lower dermis.35,36
Nevus Comedonicus
Histopathology of NC reveals cystically dilated hair follicles forming epidermal invaginations filled with lamellar keratin.8
Inflammatory Linear Verrucous Epidermal Nevus
Histologically, ILVEN typically resembles psoriasis.
Porokeratotic Adnexal Ostial Nevus
Histopathology reveals epidermal invagination with a parakeratotic column resembling a cornoid lamella, overlying a dilated eccrine acrosyringium and dermal duct.8,37 Immunohistochemical staining for carcinoembryonic antigen is positive along the cuticle of the eccrine dermal duct and acrosyringium through the channel within the parakeratotic column.37,38
Papular Epidermal Nevus With “Skyline” Basal Cell Layer
Histopathologically, the lesion displays features of a keratinocytic nevus and a striking palisading skyline pattern in the basal layer.6
Becker Nevus
On histopathology subtle findings are usually detected including acanthosis, elongation of rete ridges, variable hyperkeratosis, and basal layer hyperpigmentation, without proliferation of melanocytes. The dermis may or may not contain smooth muscle hyperplasia.8
Subtypes
KEN Subtypes
Numerous forms of KEN have been recognized based on clinical and histological features, the most frequently mentioned are:
Soft epidermal nevus of the common type—In the first stage of the disease the lesions appear as areas of excessive pigmentation, with smooth surface and then become more papillomatous.
Hard epidermal nevus of the common type—The nevus has a dark brown, warty surface and is usually covered with scales. Histologically it may mimic seborrheic keratosis.
Epidermolytic epidermal nevus—Clinically similar to other EN. Microscopic examination reveals the presence of epidermolytic hyperkeratosis.
Linear Cowden nevus—Cutaneous manifestation of Cowden syndrome type 2, associated with PTEN mutation. Lesions resemble epidermal soft nevus.
ILVEN—Linear erythematous exfoliating lesion, often with the presence of hyperkeratotic lumps. It is accompanied by severe itching.
CHILD nevus—Clinically and histopathologically demonstrates features of linear form of psoriasis. NSDHL mutations result in its formation. It mainly affects women, because the gene responsible for the disease is located on the X chromosome. Lesions are erythematous, often covered with waxy, yellow scales. It has an affinity for the skin folds.
Nevus corniculatus—Very uncommon. It has significantly hyperkeratotic surface with filamentous formations and histologically presents foci of acantholysis.
Differential Diagnosis
Basal cell carcinoma (BCC)
Squamous cell carcinoma (SCC)
Sebaceous carcinoma
Verruca vulgaris
Lichen striatus
Linear psoriasis
Linear porokeratosis
Linear Darier disease
Incontinentia pigmenti
PATHOGENESIS
A variety of cell types may form nevi or nests of cells. Cell types that reside in the epidermis, including epidermal cells or keratinocytes, sebaceous glands, hair follicles, apocrine and eccrine glands, and smooth muscle cells, are all candidates for EN formation. In general, EN are the result of cutaneous mosaicism and multiple epidermal structures may be seen
in an individual epidermal nevus, most exhibiting the predominance of one such structure and named accordingly. EN with prominent adnexal (sebaceous, follicular, and/or apocrine) differentiation are referred to as organoid nevi, and those with primarily epidermal differentiation are known as nonorganoid or keratinocytic EN.
in an individual epidermal nevus, most exhibiting the predominance of one such structure and named accordingly. EN with prominent adnexal (sebaceous, follicular, and/or apocrine) differentiation are referred to as organoid nevi, and those with primarily epidermal differentiation are known as nonorganoid or keratinocytic EN.
A postzygotic mutation or another genetic alteration in an embryonic cell destined to populate an area in the epidermis is the pathogenetic basis for EN. Genetic mosaicism of gain-of-function mutations in genes encoding fibroblast growth factor receptor 3 (FGFR3) and oncogenes Ras and PIK3CA has been reported. Given that keratinocyte progenitor cells migrate and proliferate along Blaschko lines, linear EN follow those lines. Mutations that arise very early in embryonic development lead to more extensive EN and may affect organ systems other than the skin. When other extracutaneous abnormalities occur in conjunction with EN, specific syndromes are recognized.5
Keratinocytic Epidermal Nevi
In general, KEN are the result of cutaneous mosaicism as mentioned above. Several mutations have been identified in KEN, including mutations in RAS, fibroblast growth factor receptor 3 (FGFR3), phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA) apart from the keratins39,40,41,42; therefore KEN in terms of genomics are not a single entity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree