Disorders Mostly Limited to the Epidermis and Stratum Corneum
 |
The stratum corneum is usually arranged in a delicate mesh-like or “basket-weave” pattern. It may be shed (exfoliated), or thickened (hyperkeratosis) with or without retention of nuclei (parakeratosis or orthokeratosis respectively). The granular layer may be normal, increased (hypergranulosis), or reduced (hypogranulosis). Usually, alterations in the stratum corneum result from inflammatory or neoplastic changes that affect the whole epidermis and, more often than not, the superficial dermis. Only a few conditions, mentioned in this section, show pathology mostly or entirely limited to the stratum corneum.
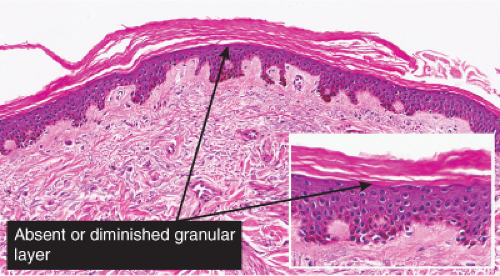
IA Hyperkeratosis with Hypogranulosis
The stratum corneum is thickened, and the granular cell layer is absent or thinned.
IA1 No Inflammation
The dermis contains only the normal scattered perivascular lymphocytes, and there is no epidermal spongiosis or exocytosis. Ichthyosis vulgaris is the prototype.
Ichthyosis Vulgaris
Clinical Summary
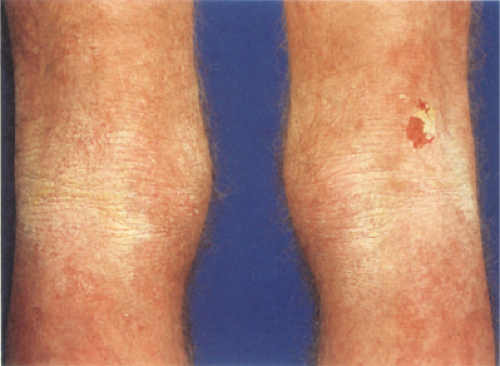
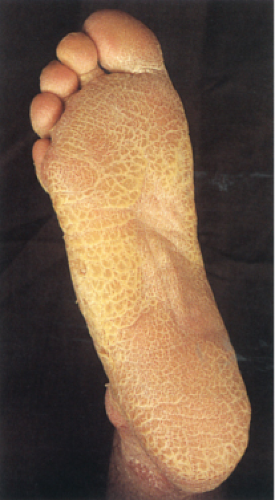
Ichthyosis includes a number of subtypes from congenital severe forms, such as harlequin ichthyosis, to mild non-congenital forms, such as ichthyosis vulgaris (IV), which is a common disorder that is usually first manifest in childhood and is inherited in an autosomal dominant fashion. Filaggrin gene mutations in IV cause keratohyalin granule deficiency, leading to hyperkeratosis and also to loss of barrier function, and increased susceptibility to atopic dermatitis (1). The skin shows scales that on the extensor surfaces of the extremities are large and adherent, resembling fish scales, and elsewhere are small. The flexural creases are spared.
Histopathology
The characteristic finding is the association of moderate compact hyperkeratosis with loss of the normal “basket-weave” pattern of the keratin and a thin or absent granular layer. The hyperkeratosis often extends into the hair follicles, resulting in large keratotic follicular plugs. The dermis is normal.
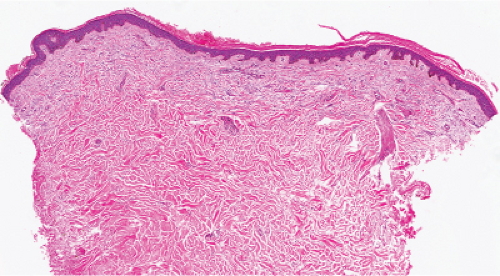 Fig. IA1.a. Ichthyosis vulgaris, low power. At this power, the epidermis appears normal, except for thickening of the stratum corneum. The dermis is normal. |
IB Hyperkeratosis with Normal or Hypergranulosis
The stratum corneum is thickened, the granular cell layer is normal or thickened, and the dermis shows only sparse perivascular lymphocytes. There is no epidermal spongiosis or exocytosis.
No Inflammation
Scant Inflammation
IB1 No Inflammation
There is hyperkeratosis and the upper dermis contains only sparse perivascular lymphocytes.
X-linked Ichthyosis
Clinical Summary
X-linked ichthyosis is recessively inherited, about 90% caused by gene deletion leading to steroid sulfatase deficiency which results in impaired hydrolysis of cholesterol sulfate leading to accumulation of cholesterol-3 sulfate in the epidermis (1,2). It is only rarely present at birth. Although female heterozygotes are frequently affected, males have a more severe form of the disorder. The thickness of the adherent scales increases during childhood. In contrast to ichthyosis vulgaris, the flexural creases may be involved.
Histopathology
There is hyperkeratosis. The granular layer is normal or slightly thickened but not thinned as in dominant ichthyosis vulgaris. The epidermis may be slightly thickened.
Table I.1. Three Prototypes of Ichthyosis (1) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
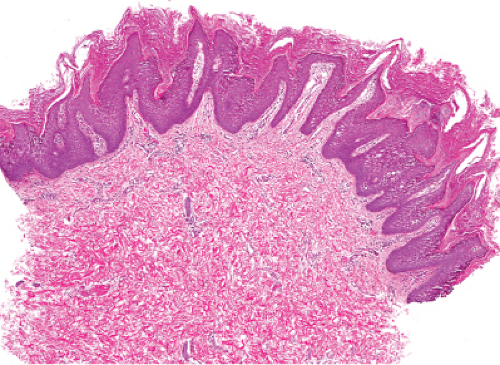
Epidermolytic Hyperkeratosis
Clinical Summary
This rather striking histologic reaction pattern is also known as granular degeneration of the epidermis. It is seen in some linear epidermal nevi and in bullous congenital ichthyosiform erythroderma. The disease results from mutations in the K1 and K10 keratin genes (chromosomes 12 and 17, respectively), which encode the keratins in the suprabasal epidermis. These mutations cause faulty assembly of keratin tonofilaments and impair their insertion into desmosomes. These flaws prevent normal development of the cytoskeleton, resulting in epidermal “lysis” and a tendency to form vesicles (3). Similar changes are also seen as one of the reaction patterns in Grover’s disease, and the same pattern is commonly observed as an incidental finding, when it may be referred to as “focal acantholytic dyskeratosis” (4).
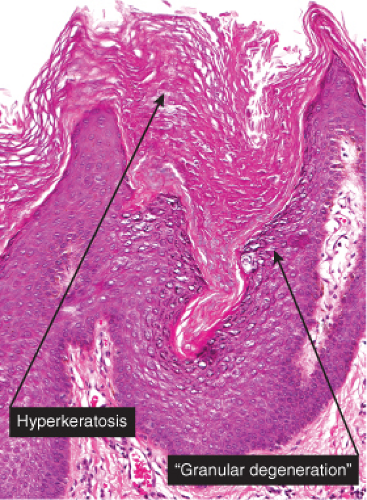
Histopathology
The salient histologic features are (1) perinuclear vacuolization of the cells in the stratum spinosum and in the stratum granulosum; (2) peripheral to the vacuolization, irregular cellular boundaries; (3) an increased number of irregularly shaped, large keratohyalin granules; and (4) compact hyperkeratosis in the stratum corneum.
Epidermodysplasia Verruciformis
Clinical Summary
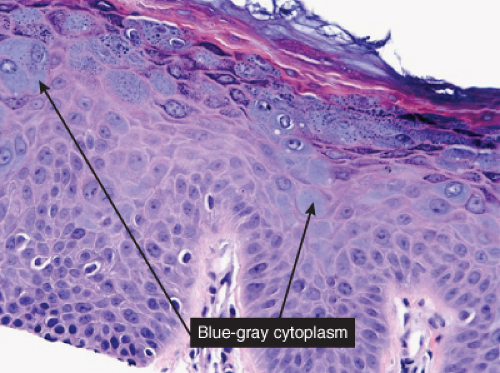
Epidermodysplasia verruciformis (EV) is a genetic disease characterized by HPV infection with types not seen in otherwise healthy individuals
(5). It usually begins in childhood and is characterized by a generalized infection by certain subtypes of HPV (referred to as “EV HPVs”), frequent association with cutaneous carcinomas, and abnormalities of cell-mediated immunity. Two forms of EV are recognized. One is induced by HPV-3 and HPV-10 and characterized by a persistent widespread eruption resembling verrucae planae with a tendency toward confluence into plaques. Some of the cases are familial. There is no tendency to malignant transformation in this form. The second form is primarily related to HPV-5. There is often a familial history with an autosomal recessive or X-linked recessive inheritance. In addition to the plane warts, irregularly outlined, slightly scaling macules of various shades of brown, red, and white, tinea versicolor-like lesions, and seborrheic keratosis like lesions have been noted. Development of Bowen’s disease (squamous cell carcinoma in situ) within lesions in exposed areas is a common occurrence, and invasive lesions of squamous cell carcinoma are occasionally found. The oncogenic potential is highest for HPV-5 and HPV-8. EV-like lesions can develop in renal transplant patients and in HIV-infected persons. Two known EV susceptibility loci, EV1 and EV2, which belong to the transmembrane channel–like (TMC) gene family, may serve as restriction factors for EV HPVs. In EV individuals, these genes are mutated and malfunctioning, causing a defective cell-mediated immune mechanism against certain types of viruses (6).
(5). It usually begins in childhood and is characterized by a generalized infection by certain subtypes of HPV (referred to as “EV HPVs”), frequent association with cutaneous carcinomas, and abnormalities of cell-mediated immunity. Two forms of EV are recognized. One is induced by HPV-3 and HPV-10 and characterized by a persistent widespread eruption resembling verrucae planae with a tendency toward confluence into plaques. Some of the cases are familial. There is no tendency to malignant transformation in this form. The second form is primarily related to HPV-5. There is often a familial history with an autosomal recessive or X-linked recessive inheritance. In addition to the plane warts, irregularly outlined, slightly scaling macules of various shades of brown, red, and white, tinea versicolor-like lesions, and seborrheic keratosis like lesions have been noted. Development of Bowen’s disease (squamous cell carcinoma in situ) within lesions in exposed areas is a common occurrence, and invasive lesions of squamous cell carcinoma are occasionally found. The oncogenic potential is highest for HPV-5 and HPV-8. EV-like lesions can develop in renal transplant patients and in HIV-infected persons. Two known EV susceptibility loci, EV1 and EV2, which belong to the transmembrane channel–like (TMC) gene family, may serve as restriction factors for EV HPVs. In EV individuals, these genes are mutated and malfunctioning, causing a defective cell-mediated immune mechanism against certain types of viruses (6).
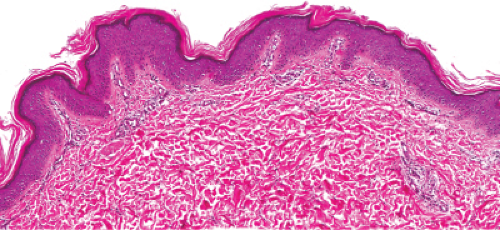 Fig. IB1.a. X-linked ichthyosis. At scanning power, the epidermis appears normal, except for uniform thickening of the stratum corneum. |
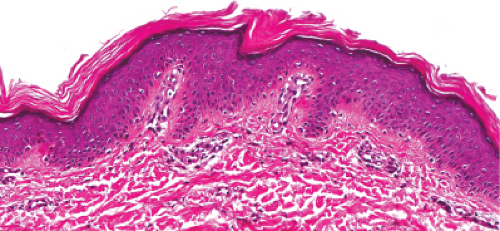 Fig. IB1.b. X-linked ichthyosis, medium power. The thickened stratum corneum (arrow) contains no parakeratotic nuclei, constituting orthokeratosis. |
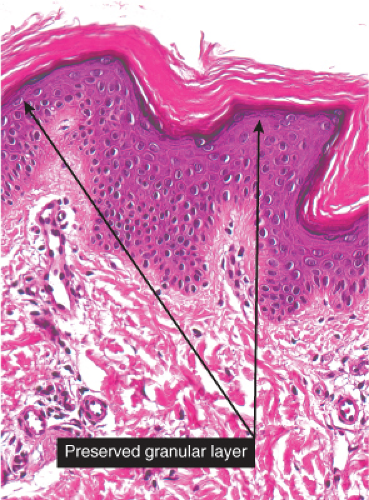 Fig. IB1.c. X-linked ichthyosis, high power. A granular layer is present, visible as a thin blue line in the upper epidermis (arrow). |
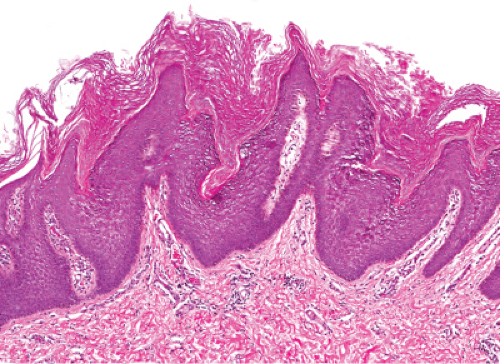 Fig. IB1.e. Epidermolytic hyperkeratosis, medium power. The epidermis shows vacuolated keratinocytes with large keratohyalin granules. There is compact hyperkeratosis in the stratum corneum. |
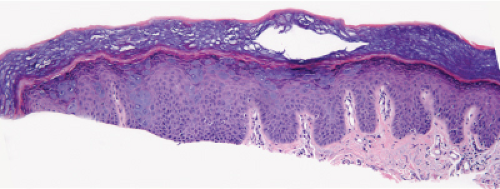 Fig. IB1.g. Epidermodysplasia verruciformis, low power. Sections show hyperkeratosis, cytoplasmic “blue-gray” change of superficial keratinocytes, and hypergranulosis. |
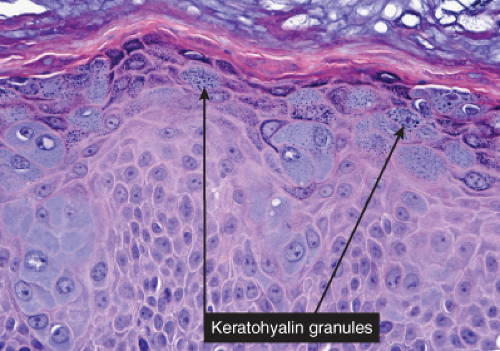 Fig. IB1.h. Epidermodysplasia verruciformis, medium power. The superficially located affected keratinocytes are swollen and irregularly shaped. There are a few lymphocytes in the upper dermis. |