Surgical dislocation of the hip can be done safely to treat a number of conditions, including femoroacetabular impingement (FAI), labral tears, chondral injuries, reduction of femoral neck fractures, femoral head, acetabular fractures, excision of tumors, reduction of acute severe slipped capital femoral epiphysis (SCFE), or any condition that requires wide complete access to the hip joint.14,15
 There is little morbidity associated with this procedure, and avascular necrosis of the femoral head is a rare complication.5
There is little morbidity associated with this procedure, and avascular necrosis of the femoral head is a rare complication.5
 This technique allows functional assessment of motion intraoperatively which is the most critical step in the treatment of FAI. Majority of reoperations after FAI treatment is due to under- or overcorrection.4
This technique allows functional assessment of motion intraoperatively which is the most critical step in the treatment of FAI. Majority of reoperations after FAI treatment is due to under- or overcorrection.4
 Also, surgical hip dislocation approach is comprehensive enough to assess and treat extra-articular impingement at the same time.16
Also, surgical hip dislocation approach is comprehensive enough to assess and treat extra-articular impingement at the same time.16
ANATOMY
 The blood supply to the femoral head is mainly from the medial femoral circumflex artery (MFCA) (FIG 1A).17
The blood supply to the femoral head is mainly from the medial femoral circumflex artery (MFCA) (FIG 1A).17
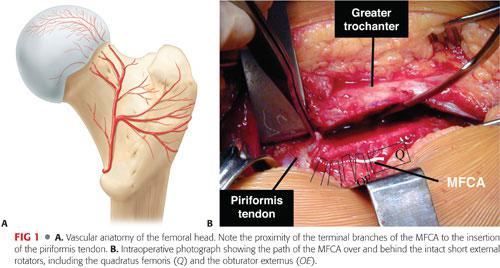
 The intact external rotator muscles, most notably the obturator externus muscle, protect the MFCA during the dislocation (FIG 1B).7
The intact external rotator muscles, most notably the obturator externus muscle, protect the MFCA during the dislocation (FIG 1B).7
PATHOGENESIS
 In FAI, anatomic deformity leads to abnormal contact between the proximal femur and the acetabular rim at the terminal extent of motion. This repetitive collision damages the soft tissue structures within the joint.3
In FAI, anatomic deformity leads to abnormal contact between the proximal femur and the acetabular rim at the terminal extent of motion. This repetitive collision damages the soft tissue structures within the joint.3
 In cam impingement, an abnormal prominence on the femoral neck passes into the hip beneath the labrum and mechanically damages the labrum and cartilage of the acetabulum.
In cam impingement, an abnormal prominence on the femoral neck passes into the hip beneath the labrum and mechanically damages the labrum and cartilage of the acetabulum.
 Pincer impingement occurs with overcoverage of the acetabular rim impinging on the anterior femoral neck or head–neck junction with terminal flexion.
Pincer impingement occurs with overcoverage of the acetabular rim impinging on the anterior femoral neck or head–neck junction with terminal flexion.
Both cam and pincer impingement can, and frequently do, coexist.
 The early chondral and labral lesions that occur in physically active adolescents and young adults can progress and result in degenerative joint disease of the hip.
The early chondral and labral lesions that occur in physically active adolescents and young adults can progress and result in degenerative joint disease of the hip.
 Causes of FAI can be idiopathic, secondary to an SCFE, anterior overcoverage of the hip with a retroverted acetabulum, residual deformity from Perthes disease, or posttraumatic changes.
Causes of FAI can be idiopathic, secondary to an SCFE, anterior overcoverage of the hip with a retroverted acetabulum, residual deformity from Perthes disease, or posttraumatic changes.
NATURAL HISTORY
 A pistol grip deformity of the femoral head has been associated with early arthrosis of the hip.9
A pistol grip deformity of the femoral head has been associated with early arthrosis of the hip.9
 End-stage osteoarthrosis of the hip, once thought to be mainly idiopathic, is now believed to be a result of mild deformities similar to those caused by childhood diseases of the hip such as developmental hip dysplasia, SCFE, and Legg-Calvé-Perthes.1
End-stage osteoarthrosis of the hip, once thought to be mainly idiopathic, is now believed to be a result of mild deformities similar to those caused by childhood diseases of the hip such as developmental hip dysplasia, SCFE, and Legg-Calvé-Perthes.1
PATIENT HISTORY AND PHYSICAL FINDINGS
 FAI usually presents in active adolescents or young adults with slow onset groin pain, which may be exacerbated by athletic activities.
FAI usually presents in active adolescents or young adults with slow onset groin pain, which may be exacerbated by athletic activities.
 Many patients have difficulty sitting for long periods and adjust their seating posture to decrease lumbar lordosis to allow less flexion at the hips. Frequently, they complain of difficulty getting into or out of a car.
Many patients have difficulty sitting for long periods and adjust their seating posture to decrease lumbar lordosis to allow less flexion at the hips. Frequently, they complain of difficulty getting into or out of a car.
 There can be a family history of hip pain, early arthrosis, or hip arthroplasty.
There can be a family history of hip pain, early arthrosis, or hip arthroplasty.
 Patients may walk with an antalgic gait, favoring the side of impingement. A foot progression angle externally rotated may indicate a chronic SCFE or femoral retroversion.
Patients may walk with an antalgic gait, favoring the side of impingement. A foot progression angle externally rotated may indicate a chronic SCFE or femoral retroversion.
 The impingement test, if positive, shows reproducible groin pain with internal rotation, which is relieved with external rotation.
The impingement test, if positive, shows reproducible groin pain with internal rotation, which is relieved with external rotation.
 The physical examination should include both flexion and internal rotation range-of-motion tests.
The physical examination should include both flexion and internal rotation range-of-motion tests.
Patients with impingement will have less than 90 degrees of true hip flexion.
Patients with impingement will have less internal rotation in flexion than extension and may have a compensatory external rotation of the hip as it is flexed.
 Radiographic findings of FAI are common in the normal, healthy population; therefore, it is paramount that good clinical–radiographic correlation be done. Additionally, other causes of hip pain such as osteoid osteoma, stress fracture, osteonecrosis are ruled out.
Radiographic findings of FAI are common in the normal, healthy population; therefore, it is paramount that good clinical–radiographic correlation be done. Additionally, other causes of hip pain such as osteoid osteoma, stress fracture, osteonecrosis are ruled out.
IMAGING AND OTHER DIAGNOSTIC STUDIES
 Plain radiographs should include an anteroposterior (AP) view of the pelvis and a lateral view of the hip (FIG 2A,B). The maximal deformity of the head–neck junction in FAI could be localized best by the 45-degree Dunn view.10
Plain radiographs should include an anteroposterior (AP) view of the pelvis and a lateral view of the hip (FIG 2A,B). The maximal deformity of the head–neck junction in FAI could be localized best by the 45-degree Dunn view.10
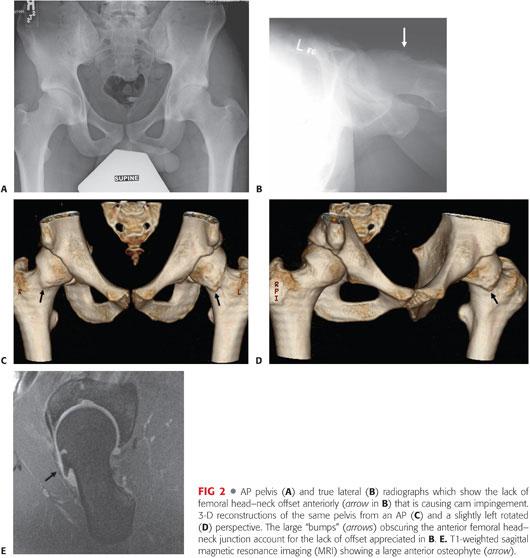
 Computed tomography (CT) scans with two- and three-dimensional (3-D) reconstructions are helpful for preoperative planning and detecting subtle femoral head–neck junction prominence (FIG 2C,D).
Computed tomography (CT) scans with two- and three-dimensional (3-D) reconstructions are helpful for preoperative planning and detecting subtle femoral head–neck junction prominence (FIG 2C,D).
 Magnetic resonance imaging can further delineate the labral and cartilage pathology (FIG 2E). If the study is performed with gadolinium and high-resolution sagittal oblique or radial sequences, labral pathology can be detected.
Magnetic resonance imaging can further delineate the labral and cartilage pathology (FIG 2E). If the study is performed with gadolinium and high-resolution sagittal oblique or radial sequences, labral pathology can be detected.
DIFFERENTIAL DIAGNOSIS
 FAI
FAI
 Labral tear
Labral tear
 Hip dysplasia
Hip dysplasia
 SCFE
SCFE
 Acetabular retroversion
Acetabular retroversion
NONOPERATIVE MANAGEMENT
 Nonoperative management includes cessation of aggravating activities and symptomatic treatment using nonsteroidal anti-inflammatories.
Nonoperative management includes cessation of aggravating activities and symptomatic treatment using nonsteroidal anti-inflammatories.
 Physical therapy to strengthen the hip musculature does not address the mechanical impingement of FAI but may have a role in affecting pelvic inclination.
Physical therapy to strengthen the hip musculature does not address the mechanical impingement of FAI but may have a role in affecting pelvic inclination.
SURGICAL MANAGEMENT
 Hip pathology may be addressed through hip arthroscopy. However, it may be difficult to dynamically assess hip mechanics before and after débridement.
Hip pathology may be addressed through hip arthroscopy. However, it may be difficult to dynamically assess hip mechanics before and after débridement.
 Femoral head–neck osteoplasty may be performed through an anterior approach to the hip without a surgical dislocation. However, the articular cartilage of the acetabulum and most of the femoral head cannot be evaluated with this limited approach.
Femoral head–neck osteoplasty may be performed through an anterior approach to the hip without a surgical dislocation. However, the articular cartilage of the acetabulum and most of the femoral head cannot be evaluated with this limited approach.
Preoperative Planning
 All imaging studies are reviewed.
All imaging studies are reviewed.
 The lack of femoral head–neck offset is best appreciated on the 45-degree Dunn lateral view of the hip (see FIG 2A,B) or on the radial reformats of CT or magnetic resonance (MR) scans around the femoral neck axis or 3-D reconstruction of a CT scan.
The lack of femoral head–neck offset is best appreciated on the 45-degree Dunn lateral view of the hip (see FIG 2A,B) or on the radial reformats of CT or magnetic resonance (MR) scans around the femoral neck axis or 3-D reconstruction of a CT scan.
 A CT scan that includes cuts through the distal femoral condyles may be used to accurately measure the amount of femoral version.11
A CT scan that includes cuts through the distal femoral condyles may be used to accurately measure the amount of femoral version.11
 After general anesthesia is administered, the patient’s hips are examined. The amount of true hip flexion and internal and external rotation with the hip extended and hip flexed are noted and compared to the preoperative assessment.
After general anesthesia is administered, the patient’s hips are examined. The amount of true hip flexion and internal and external rotation with the hip extended and hip flexed are noted and compared to the preoperative assessment.
Positioning
 The patient is placed in the full lateral position, secured on a pegboard. A flat-top cushion (with a half-moon–shaped cutout for the down leg) placed beneath the operative side helps to stabilize the leg during the approach (FIG 3A–C).
The patient is placed in the full lateral position, secured on a pegboard. A flat-top cushion (with a half-moon–shaped cutout for the down leg) placed beneath the operative side helps to stabilize the leg during the approach (FIG 3A–C).
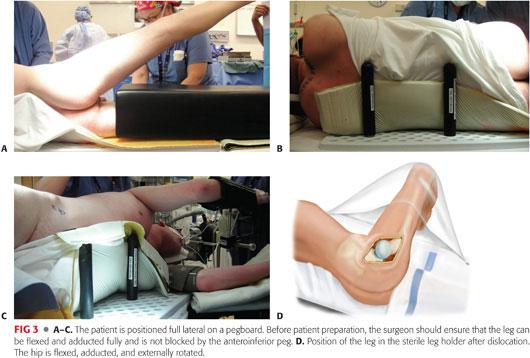
 A hip drape with a sterile side bag is used, which will capture the leg during the dislocation maneuver (FIG 3D).
A hip drape with a sterile side bag is used, which will capture the leg during the dislocation maneuver (FIG 3D).
Approach
 The approach consists of an anterior dislocation through a Kocher-Langenbeck or a Gibson approach with a trochanteric flip osteotomy (FIG 4A,B).
The approach consists of an anterior dislocation through a Kocher-Langenbeck or a Gibson approach with a trochanteric flip osteotomy (FIG 4A,B).
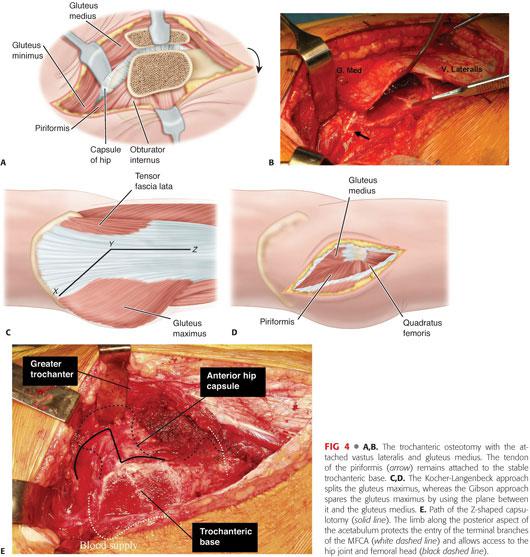
 A Kocher-Langenbeck incision is followed by splitting the gluteus maximus muscle.
A Kocher-Langenbeck incision is followed by splitting the gluteus maximus muscle.
 The abductors and gluteus maximus muscles can be spared by performing a Gibson approach, which proceeds between the gluteus medius and maximus (FIG 4C,D).8
The abductors and gluteus maximus muscles can be spared by performing a Gibson approach, which proceeds between the gluteus medius and maximus (FIG 4C,D).8
The Gibson approach may result in less hip extensor dysfunction but may make anterior exposure more difficult.
 A Z-shaped capsulotomy is made to allow entry to the hip joint while protecting the deep branch of the MFCA (FIG 4E).5
A Z-shaped capsulotomy is made to allow entry to the hip joint while protecting the deep branch of the MFCA (FIG 4E).5
TECHNIQUES
 Surgical Hip Dislocation by a Transtrochanteric Approach
Surgical Hip Dislocation by a Transtrochanteric Approach
Approach to Hip Capsule
A longitudinal lateral incision is made, centered over the junction between the anterior and middle thirds of the greater trochanter (TECH FIG 1A).
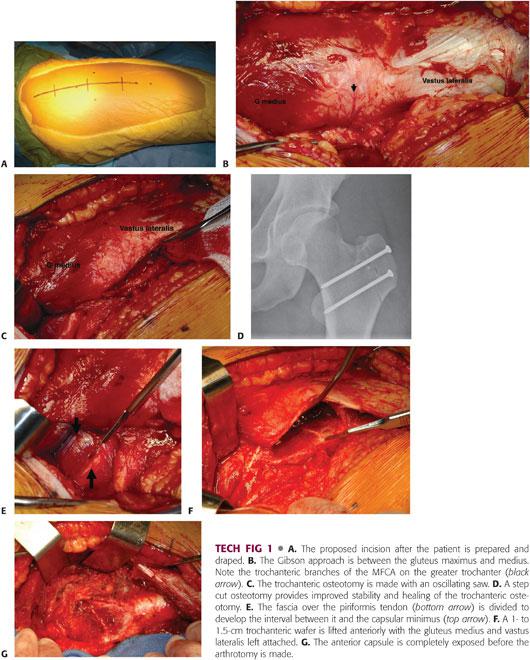
The fascia lata is split distally in line with the incision. The proximal dissection progresses through the interval between the anterior edge of the gluteus maximus and the tensor (TECH FIG 1B).
The proximal 4 to 5 cm of fascia of the vastus lateralis is incised, and the vastus muscle fibers are reflected anteriorly.
The gluteus maximus, along with the fascia of the gluteus medius, which is left on the undersurface of the gluteus maximus for protection, is reflected posteriorly to expose the gluteus medius and insertion.
A 1- to 1.5-cm thick trochanteric osteotomy is made with an oscillating saw, leaving the piriformis tendon and short external rotators intact on the remaining base of the greater trochanter (TECH FIG 1C).
A trochanteric step cut can be performed using two saw blades 6 mm apart if a relative neck lengthening is not planned. This provides excellent stability of the trochanteric osteotomy with lower rates of trochanteric delayed union (TECH FIG 1D).
The fascia overlying the piriformis tendon is incised to identify the tendon and the interval between the piriformis and capsular minimus muscles (TECH FIG 1E).
The trochanteric wafer is next reflected and flipped anteriorly with its attached sleeve of vastus lateralis and the gluteus medius (TECH FIG 1F).
The capsular minimus is elevated in an anterior direction off the hip capsule by carefully dissecting in the interval between the posterior edge of the capsular minimus and the piriformis tendon (TECH FIG 1G).
An assistant may use a right angled retractor to assist with the exposure of the capsule.
Progressive hip flexion, external rotation, and adduction further aid the exposure.
The hip capsule is exposed up to the rim of the acetabulum.
Hip Arthrotomy and Dislocation
A Z-shaped capsulotomy is then performed, with the longitudinal arm of the Z in line with the anterior neck of the femur (TECH FIG 2).
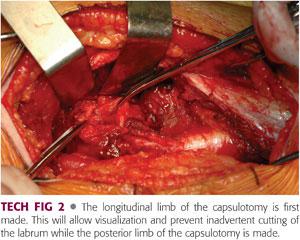
The distal arm of the capsulotomy extends anteriorly well proximal to the lesser trochanter.
The proximal arm is extended posteriorly along the acetabular rim, just distal to the labrum and well proximal to the retinacular branches of the MFCA entering the capsule posteriorly to supply the femoral head.
Depending on the pathology, the hip is brought through a range of motion to determine areas of impingement in a dynamic fashion.
The leg is then placed in the sterile side bag, flexed, externally rotated, and adducted while the hip is subluxated anteriorly through the arthrotomy.
A bone hook placed around the anterior femoral neck may be needed to subluxate the hip.
The ligamentum teres is then divided using curved meniscus scissors to allow full dislocation of the hip.
Dynamic Assessment and Osteoplasty
The entire femoral head and acetabulum can now be assessed for chondral flaps or labral tears, which can be repaired using suture anchors spaced about 7 to 10 mm apart or débrided.
The aspherical segment of the femoral head at the head–neck junction can be resected using a quarter-inch osteotome and rongeur (TECH FIG 3A,B).
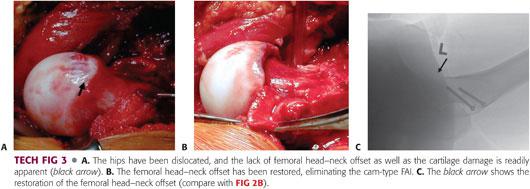
After reestablishing sphericity of the femoral head, the hip is reduced and the results of the débridement are assessed by bringing the hip through a range of motion and confirming the relief of impingement and improvement in range of motion.
Intraoperative fluoroscopy showing a lateral of the hip in 90 degrees of flexion will determine if the femoral head–neck offset has been reestablished (TECH FIG 3C).
Osteotomy Fixation
The trochanteric wafer is reduced and held in position with a towel clip.
Three 3.5-mm small fragment screws are placed to secure the trochanter. Fluoroscopy confirms reduction and fixation of the osteotomy (TECH FIG 4).

Alternatively, 4.0-mm cannulated screws or 4.5-mm cortical screws may be used for trochanteric fixation.
Closure
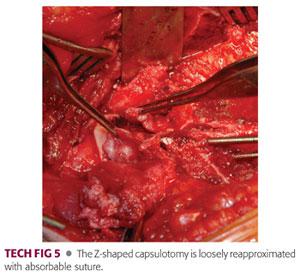
The Z-shaped capsulotomy is loosely repaired using absorbable 2-0 suture (TECH FIG 5).
The fascia of the vastus lateralis is closed with a running absorbable suture. The fascia lata and the fascia between the tensor and gluteus maximus are reapproximated.
Skin is closed in routine fashion.
PEARLS AND PITFALLS | |
Indications |
|
| |
Approach |
|
Trochanteric osteotomy |
|
| |
Heterotopic ossification |
|
Femoral neck fracture |
|
POSTOPERATIVE CARE
 The hip is held flexed and in neutral rotation by placing two pillows under the leg and one under the greater trochanter.
The hip is held flexed and in neutral rotation by placing two pillows under the leg and one under the greater trochanter.
 The patient is placed in a continuous passive motion machine for 6 hours a day, set from 30 to 80 degrees of flexion.
The patient is placed in a continuous passive motion machine for 6 hours a day, set from 30 to 80 degrees of flexion.
 Prophylaxis for deep venous thrombosis is individualized; however, all patients should be started on mechanical compression devices immediately.
Prophylaxis for deep venous thrombosis is individualized; however, all patients should be started on mechanical compression devices immediately.
 After the epidural is removed (if used), out-of-bed ambulation is permitted with one-sixth body weight partial weight bearing.
After the epidural is removed (if used), out-of-bed ambulation is permitted with one-sixth body weight partial weight bearing.
 Range-of-motion exercises are started, but care is taken to protect the greater trochanter osteotomy by limiting adduction to midline and avoiding resisted abduction exercises for 6 weeks.
Range-of-motion exercises are started, but care is taken to protect the greater trochanter osteotomy by limiting adduction to midline and avoiding resisted abduction exercises for 6 weeks.
 Some patients may benefit from heterotopic ossification prophylaxis using indomethacin.
Some patients may benefit from heterotopic ossification prophylaxis using indomethacin.
 AP view of the pelvis or hip and true lateral hip radiographs are obtained 6 weeks postoperatively. Weight bearing is increased to full, and hip strengthening exercises are prescribed.
AP view of the pelvis or hip and true lateral hip radiographs are obtained 6 weeks postoperatively. Weight bearing is increased to full, and hip strengthening exercises are prescribed.
OUTCOMES
 Ganz et al6 has performed over 1200 surgical hip dislocations with no cases of osteonecrosis reported.
Ganz et al6 has performed over 1200 surgical hip dislocations with no cases of osteonecrosis reported.
 Generally, outcomes are excellent if the correct pathology is addressed in a joint without significant preexisting arthrosis.
Generally, outcomes are excellent if the correct pathology is addressed in a joint without significant preexisting arthrosis.
 In a clinical assessment in adults by Murphy et al12 using the Merle d’Aubigné scale, hip scores improved significantly.
In a clinical assessment in adults by Murphy et al12 using the Merle d’Aubigné scale, hip scores improved significantly.
 Almost 80% of patients were satisfied with results of surgical dislocation approach treatment for FAI at midterm.13
Almost 80% of patients were satisfied with results of surgical dislocation approach treatment for FAI at midterm.13
COMPLICATIONS
 Avascular necrosis of the femoral head can occur if care is not taken to follow the technique and to preserve the retinacular vessels.
Avascular necrosis of the femoral head can occur if care is not taken to follow the technique and to preserve the retinacular vessels.
 Femoral neck fracture if the femoral head–neck junction is aggressively débrided.
Femoral neck fracture if the femoral head–neck junction is aggressively débrided.
 Sciatic or femoral nerve neurapraxia
Sciatic or femoral nerve neurapraxia
 Greater trochanteric nonunion
Greater trochanteric nonunion
 Heterotopic ossification
Heterotopic ossification
 Repeat labral tear
Repeat labral tear
 Continued arthrosis of the joint
Continued arthrosis of the joint
 Painful postoperative joint adhesions2
Painful postoperative joint adhesions2
REFERENCES
1. Aronson J. Osteoarthritis of the young adult hip: etiology and treatment. Instruct Course Lect 1986;35:119–128.
2. Beck M. Groin pain after open FAI surgery: the role of intraarticular adhesions. Clin Orthop Relat Res 2009;467:769–774.
3. Clohisy JC, Kim YJ. Femoroacetabular impingement research symposium. J Am Acad Orthop Surg 2013;21(suppl 1):vi–viii.
4. Clohisy JC, Nepple JJ, Larson CM, et al. Persistent structural disease is the most common cause of repeat hip preservation surgery. Clin Orthop Relat Res 2013;471(12):3788–3794.
5. Ganz R, Gill T, Gautier E, et al. Surgical dislocation of the adult hip. J Bone Joint Surg Br 2001;83(8):1119–1124.
6. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;(417):112–120.
7. Gautier E, Ganz K, Krügel N, et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br 2000;82(5):679–683.
8. Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg Br 1950;32-B(2):183–186.
9. Goodman DA, Feighan JE, Smith AD, et al. Subclinical slipped capital femoral epiphysis. Relationship to osteoarthrosis of the hip. J Bone Joint Surg Am 1997;79(10):1489–1497.
10. Meyer DC, Beck M, Ellis T, et al. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res 2006;445:181–185.
11. Murphy SB, Simon SR, Kijewski PK, et al. Femoral anteversion. J Bone Joint Surg Am 1987;69(8):1169–1176.
12. Murphy S, Tannast M, Kim YJ, et al. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res 2004;(429):178–181.
13. Naal FD, Miozzari HH, Schär M, et al. Midterm results of surgical hip dislocation for the treatment of femoroacetabular impingement. Am J Sports Med 2012;40:1501–1510.
14. Spencer S, Millis M, Kim YJ. Early results of treatment for hip impingement syndrome in slipped capital femoral epiphysis and pistol grip deformity of the femoral head–neck junction using the surgical dislocation technique. J Pediatr Orthop 2006;26:281–285.
15. Tannast M, Krüger A, Mack PW, et al. Surgical dislocation of the hip for the fixation of acetabular fractures. J Bone Joint Surg Br 2010;92(6):842–852.
16. Tibor LM, Sink EL. Pros and cons of surgical hip dislocation for the treatment of femoroacetabular impingement. J Pediatr Orthop 2013;33(suppl 1):S131–S136.
17. Trueta J, Harrison MH. The normal vascular anatomy of the femoral head in adult man. J Bone Joint Surg Br 1953;35-B(3):442–461.
< div class='tao-gold-member'>










