Developmental Dysplasia of the Hip, Infant, Toddler, Child
Travis Matheney
Closed Reduction
Operative Indications
Unilateral or bilateral infant hip dysplasia or dislocation in those younger than 18 months having failed conservative/bracing treatment
Anesthesia
Request neuromotor relaxation
Local anesthetic available if an adductor tenotomy is performed
Equipment
Radiolucent OR table
Fluoroscopy
Arthrography setup
Injectable sterile saline
Contrast agent mixed 50:50 with sterile injectable saline
Short leash of IV tubing connected to syringes of saline and contrast mix
Allows injection and position checks on fluoroscopy while keeping your hands out of the image beam
Spica casting table
20-gauge spinal needle
Extra personnel to help hold during casting
Access to intraoperative ultrasound
Examination Under Anesthesia
Complete muscle relaxation
Examine for Ortolani and Barlow signs
Assess for presence/size of “stable zone”; want at least 25 (ideally more) degree zone of adduction/abduction of the hip(s) where hip is felt to be reduced
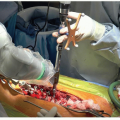
Arthrography
Utilized to confirm examination under anesthesia (EUA) findings
Limited sterile prep of groin(s) with prep solution and wide area of sterile towels to facilitate a sterile working space
A 20-gauge spinal needle inserted under adductor longus aiming roughly at the ipsilateral axilla
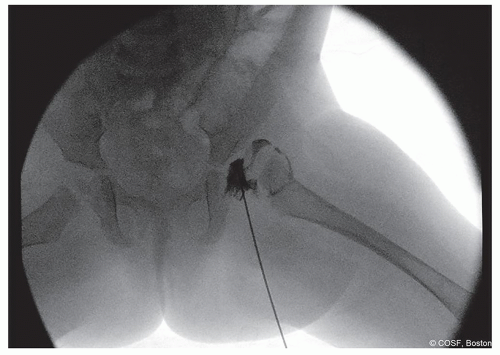
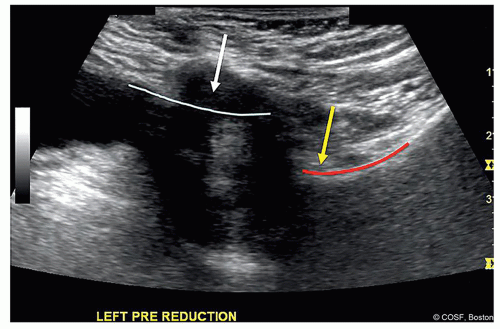
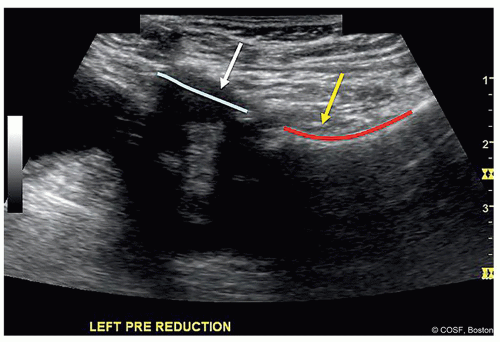
Figure 20-1 ▪ Arthrogram of subluxated left hip. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
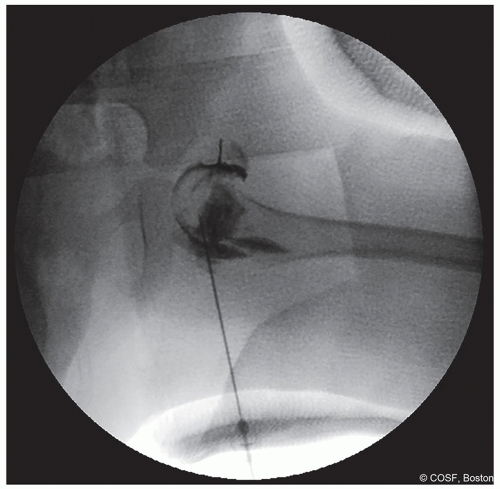
Figure 20-2 ▪ Arthrogram is performed through the groin opening of the cast to confirm hip position after casting. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
In dislocated hip, try to insert into the vacant acetabulum in the inferior side (Figure 20.1)
If you happen to not be in the joint, when you inject contrast material, it will decrease the chances that you create an aberrant “dust cloud” over your areas of interest
In subluxated/dysplastic hips, flex hip and aim for the proximal portion of the inferior femoral neck
Once in cast, if position of the hip is in question, after sterile swab of the exposed groin, you can repeat the arthrogram in cast (Figure 20.2)
Intraoperative Contrast-Enhanced Ultrasound*
Ultrasound can be utilized intraoperatively to assess both hip reduction and hip perfusion
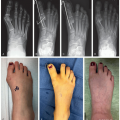
Hip reduction is assessed both prior to casting and in spica cast via an anterior/transinguinal approach (Figures 20.3,20.4,20.5)
This imaging has been validated against cross-sectional imaging1
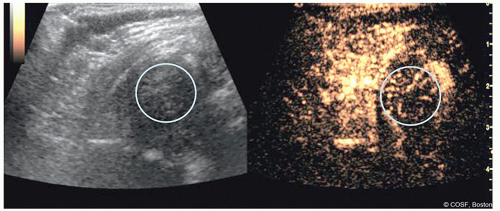
Proximal femoral perfusion can be assessed using intravenous contrast
Perfusion can be graded as “good,” “partial decrease,” or “global decrease” in perfusion
Assessment is performed before attempted reduction and after casting as part of the reduction assessment (Figures 20.6 and 20.7)

Figure 20-5 ▪ In cast ultrasound from anterior view. Cast is modified to allow access to hip. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
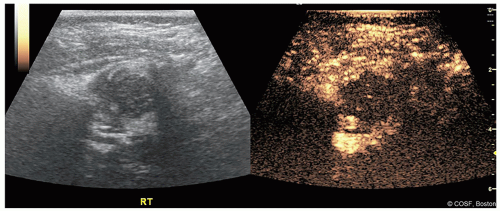
Figure 20-7 ▪ Contrast-enhanced ultrasound after attempted closed reduction and decreased perfusion. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
Preliminary data points to a strong correlation between decreases in perfusion and eventual development of proximal femoral growth disturbance (PFGD)
Technique requires prior agreement with your radiology department and access to appropriate ultrasound machine and intravenous contrast agent
Positioning
Supine on radiolucent operating table
Fluoroscopy is positioned on the opposite side of operative hip if unilateral
If a radiolucent casting table is available, you can consider positioning on this for reduction to facilitate immediate transition to casting once you affect a reduction
Technique in Steps
Apply cast liner (stockinette or water-resistant liner)
Affected hip is flexed and abducted with pressure behind greater trochanter to position deemed most stable on arthrography
Assess “safe zone” of the reduction—the range of adduction to abduction where hip is stable, ideally more than 25° arc
If the safe zone is small and the adductor longus feels tight, consider lengthening of the adductor longus to improve the safe zone
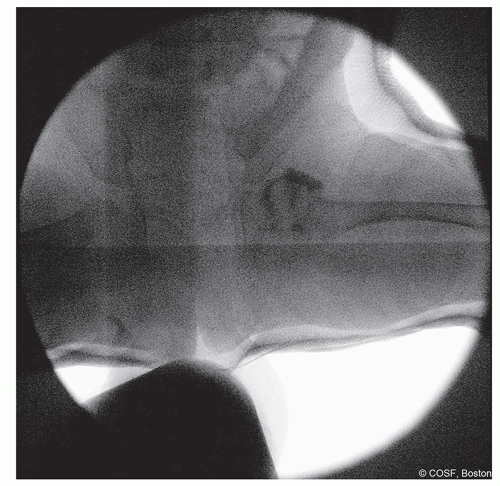
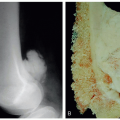
Figure 20-8 ▪ Postreduction anteroposterior (AP) view arthrogram to help confirm reduction. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
This can be accomplished either percutaneously with a #15 or #11 blade or through small 1.5-cm transverse incision directly over the longus tendon following sterile prep of that area
Spica cast is applied with cotton Webril and either fiberglass (our preferred method) or plaster (see Spica casting tips below)
A well-made cast is at least half of this procedure
Cast must have snug contact with
Iliac crests
Greater trochanters—caution not to apply the “SuperMold” as this may lead to pressure-induced femoral head ischemia
Ischial tuberosities
In-cast fluoroscopy or plain radiographs are obtained of the operative hip(s) in both anteroposterior (AP) and iliac oblique Judet views for comparison to in-clinic imaging obtained postoperatively (Figures 20.8 and 20.9)
Postoperative Care
Patient and family are admitted for recovery and spica cast care teaching
Car seat evaluation with current car seat to assure proper fit
Postoperative in cast radiographs can be taken within 10 to 14 days to assure no late displacement in the cast
Total anticipated casting time is typically 3 months
Cast change in the operating room either monthly or at 6 weeks with cast removal in clinic at 3 months
Post cast bracing at the discretion of the surgeon
Where persistent instability or dysplasia is a concern, use of an abduction splint may be beneficial
Postoperative Imaging
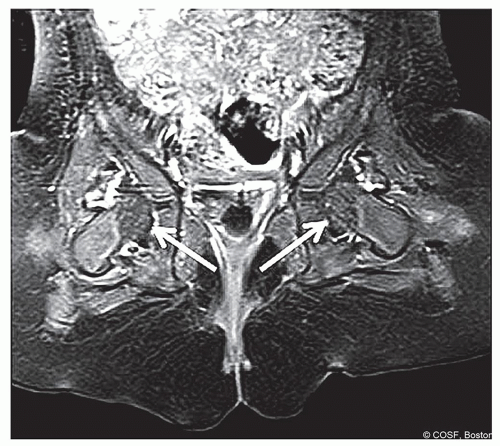
Postoperative multiplanar imaging in spica is commonly used to confirm hip reduction in cast after this child recovers from anesthesia
Both computed tomography (CT) and magnetic resonance imaging (MRI) have been utilized to confirm hip reduction in spica cast
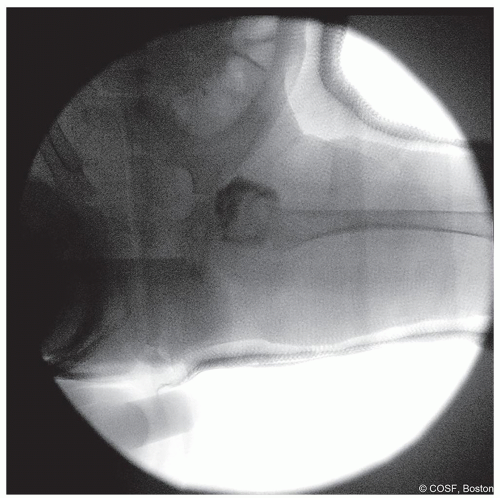
Figure 20-9 ▪ Postreduction iliac oblique Judet view to help confirm reduction. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
Evidence suggests that “global decreased enhancement” of the femoral epiphysis and/or hip abduction in cast greater than 60° correlates with the development of PFGD2 (Figures 20.10 and 20.11)
What if there is globally decreased enhancement? Assess the amount of hip abduction, amount of trochanteric molding, and relative difficulty maintaining the reduction
If any of the above are present, consider remaking the cast and/or conversion to open reduction
Complications
Recurrent dislocation
Emphasizes the precasting assessment of hip stability and size of the “safe zone” for stable reduction
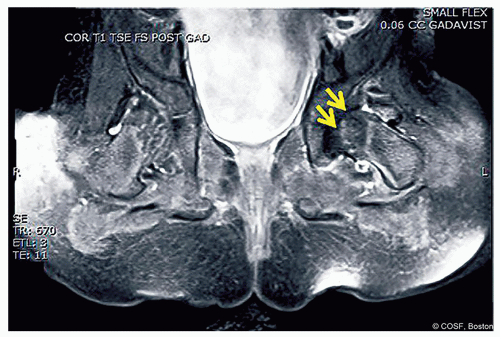
Figure 20-11 ▪ Postoperative contrast-enhanced magnetic resonance image (MRI) demonstrating global decreased enhancement of the left femoral epiphysis as noted by the arrows in agreement with the femoral epiphysis in Figure 20.7. (Courtesy of Children’s Orthopaedic Surgery Foundation.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access