Key points
- •
What is photothermolysis?
- •
How does the CO 2 laser remove wrinkles and tighten skin?
- •
What is fractional laser skin resurfacing?
- •
What are the contraindications to laser skin resurfacing and blepharoplasty?
- •
What are the advantages of CO 2 laser blepharoplasty?
- •
What are the crucial steps in post laser skin resurfacing wound care?
CO 2 laser skin resurfacing
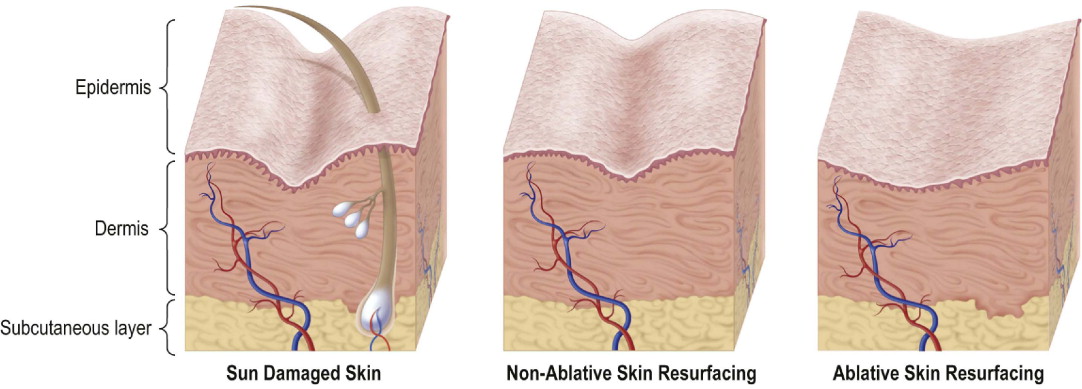
The technique of CO 2 laser skin resurfacing (LSR) for the removal of photo-aging skin pathology, including wrinkles and solar lentigines, and skin tightening is based on the concept of photothermolysis. Utilizing CO 2 laser light (photo) energy which is highly absorbed by water, the skin is irradiated with the laser beam, intracellular water is heated (thermo) to a point where cell rupture (lysis) occurs. With CO 2 and 2940 Er:YAG lasers, the lasers most highly absorbed by water, sufficient cellular injury occurs to actually ablate or remove photo-damaged epidermal cells and damaged superficial dermis. In addition, the cellular injury in the dermis causes residual thermal damage (RTD) which initiates an intense inflammatory cascade. This results in the production of new collagen in the dermis to replace the actinically damaged dermal collagen.
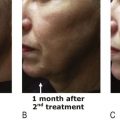
The new dermal collagen and wound healing response result in wrinkle removal and skin tightening ( ). The ablation of photo-damaged skin by CO 2 LSR provides superior wrinkle removal and skin tightening compared to non-ablative LSR which only heats, but does not remove, photo-damaged skin ( Figure 2.1 ). However traditional flat-beam ablative LSR is followed by 2–3 weeks of recovery time and often months of prolonged erythema, and long term hypo-pigmentation is common.
Fractional CO 2 laser skin resurfacing
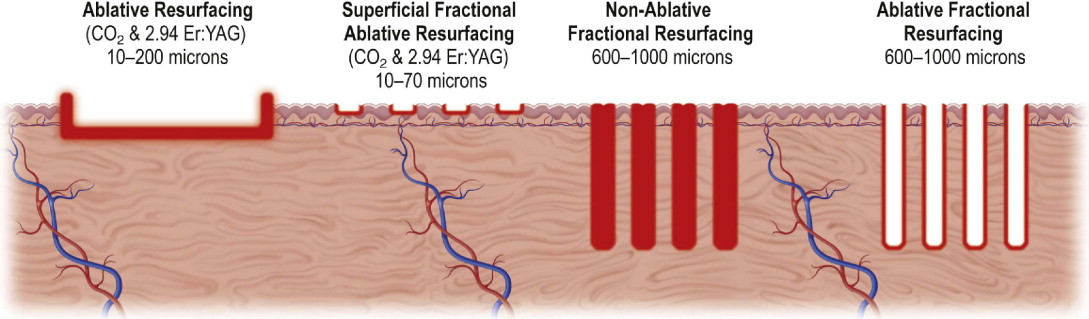
The prolonged recovery and attendant morbidity have dampened enthusiasm for traditional flat-beam CO 2 and erbium laser resurfacing in spite of the ability to achieve significant results with these techniques. Recently, new technology called fractional laser skin resurfacing (LSR) has been developed which has dramatically shortened recovery time and lessened the occurrence of complications.
With fractional laser resurfacing the laser beam is broken up or fractionated, into many small micro-beams. These micro-beams are separated and thus, when they strike the skin surface, small areas of the skin between the beams are not hit by the laser and are left intact. These small areas of untreated skin promote a much more rapid re-epithelialization, recovery and healing with less risk of complications. The small areas treated by the fractional micro-beams, called micro-treatment zones (MTZs), cause sufficient laser injury deep in the dermis to promote new collagen production and resultant facial skin rejuvenation. Early fractional LSR devices were non-ablative. They heated but did not ablate the tissue in the MTZs. Although the non-ablative LSR lasers are effective at plumping the skin and removing pigment, they are less effective for wrinkle removal than traditional flat-beam ablative LSR lasers. During the past year, fractional ablative CO 2 and erbium lasers have been developed which ablate columns of skin as deep as 1600 microns ( Figure 2.2 ). The Reliant Fraxel re:pair® and the Lumenis UltraPulse Encore™ DeepFX are two of the most commonly used ablative fractional CO 2 lasers.
CO 2 laser blepharoplasty
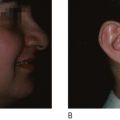
CO 2 laser blepharoplasty using the 0.2 mm incisional hand piece on the Lumenis UltraPulse® CO 2 laser, is a very precise, atraumatic technique for incisional upper and transconjunctival lower blepharoplasty. The CO 2 laser blepharoplasty provides superior hemostasis, accurate control of incisional margins and reduced operating time in a bloodless field ( Box 2.1 ). The safety and efficacy of the CO 2 laser blepharoplasty have been well documented ( ). The benefits of combined periocular CO 2 LSR and transconjunctival orbicularis oculi muscle and septal tightening have dramatically improved cosmetic results in eyelid and periocular skin rejuvenation.
Less bleeding
Less operative time
More precise
Less trauma to tissues
Early recovery of the patient
Less pain
Less swelling
Patient selection
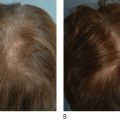
CO 2 LSR is best limited to patients with fair skin because of the risk of post LSR hypo-pigmentation and demarcation lines between treated and untreated skin. Therefore I limit CO 2 LSR to patients with Fitzpatrick Type 1, 2, and 3 skin. Although many physicians have successfully treated darker skin types, I do not because of the risk of hypo-pigmentation.
Contraindications to CO 2 LSR include active infection, prior use of Accutane® within the past 6–12 months, skin atrophy from previous laser resurfacing or chemical peel, significant psychopathology, unrealistic expectations, non-compliant patient, active pustular acne or skin infection, deficient wound healing, and use of anticoagulant medication ( Box 2.2 ).
Active herpes simplex infection
Psychoneurosis – active abuse of drugs and alcohol
History of hypertrophic or keloid scar
History of hyperpigmentation or hypo-pigmentation
Use of Accutane in previous 6 months
Unrealistic expectations
The non-compliant patient
CO 2 laser blepharoplasty can be done on any patient who is an appropriate candidate for incisional upper and transconjunctival lower blepharoplasty. Contraindications to blepharoplasty include uncontrolled hypertension, Graves’ disease, proptosis greater than 3 millimeters, uncontrolled glaucoma, serious retinal disease, dry eye syndrome, acute blepharitis, and blepharochalasis ( Box 2.3 ).
Uncontrolled hypertension
Graves’ disease
Proptosis >3 mm
Uncontrolled glaucoma
Serious retinal disease
Dry-eye syndrome
Acute blepharitis or blepharochalasis
Indications
CO 2 LSR is indicated for the treatment of skin photo-aging pathology including wrinkles, solar lentigines, diffuse superficial hyperpigmentation, multiple widespread actinic keratoses, sebaceous hyperplasia, rhinophyma, and acne scarring. These are accepted indications for traditional flat-beam CO 2 LSR. Fractional CO 2 LSR is indicated primarily for wrinkle and pigment removal and acne scarring. Efficacy for treatment of actinic keratoses and exophytic skin lesions has not yet been established for fractional ablative lasers.
Indications for CO 2 laser blepharoplasty include dermatochalasis, excess upper eyelid skin causing ‘hooding’ of the eyes, herniation of the infraorbital fat causing puffiness or ‘bags’ on the lower eyelids, and skin excess or photo-aging changes on the lower eyelid skin. A new indication for lower eyelid blepharoplasty is the arcus deformity which is also called the ‘dark circle under the eye’. The arcus deformity is caused by the attachment of the arcus marginalis to the underside of the lower lid combined with skin laxity and herniation of lower eyelid fat. The arcus deformity can be corrected with a transconjunctival laser lower blepharoplasty with arcus release and fat repositioning or fat grafting onto the orbital rim.
Operative technique
Pre-operative preparation
Pre-operative preparation for all patients includes a thorough history and physical examination, preferably performed 10 days to 2 weeks before CO 2 laser resurfacing or CO 2 laser blepharoplasty. Screening for contraindications to LSR is essential. If CO 2 LSR or CO 2 blepharoplasty of the lower eyelids is contemplated, lid laxity must be evaluated using the Jelk’s lid snap test. Several predisposing factors, especially laxity of the lower eyelids, can increase the risk of ectropion following LSR or blepharoplasty ( Box 2.4 ).
Hypotonicity of lid
Malar hypoplasia
Shallow orbit
Graves’ ophthalmology
Unilateral high myopia (long eyeball)
Large eye
Secondary blepharoplasty
At the pre-operative visit, patients undergoing CO 2 LSR are given prescriptions for oral antibiotics such as Duracef® (500 milligrams twice a day) or Eryc® (500 milligrams daily) beginning the day of the procedure. I also prescribe the antiviral Valtrex® (500 milligrams twice a day for 10 days) beginning one day before the procedure. For patients who are having the CO 2 LSR under topical anesthesia I prescribe Percocet® (1 tablet) and diazepam (5 milligrams) to be taken 1 hour prior to the procedure. For patients who have, or are at risk for, hyperpigmentation I also prescribe a bleaching regimen to begin 3–6 weeks prior to LSR. This consists of a uniform mixture of 4% hydroquinone, 0.1% Retin A®, and 1% hydrocortisone cream which are to be mixed in the hand and applied to the facial skin one to two times a day and to be discontinued a day before LSR.
Reliant Technologies recommends clobetasol propionate 0.05% cream applied twice daily starting the day before the Fraxel re:pair® fractional CO 2 LSR procedure. Benadryl® 25 milligrams is also prescribed at bedtime starting the night before the procedure and for 2–3 nights after the procedure. I also have patients acquire Aquaphor® ointment, gauze sponges and normal saline solution for post-operative wound care. Patients who are having CO 2 blepharoplasty are given Lacrilube® and erythromycin ophthalmic ointment for use after surgery as well as the prophylactic antibiotics listed above.
Traditional flat-beam CO 2 LSR with the CO 2 UltraPulse laser
Good results and avoidance of complications require knowledge of laser skin interactions, skin micro-anatomy, wound healing response and the depth of laser injury caused by the particular laser in use. These details cannot be covered here and the reader is referred to a detailed coverage of these variables described below for the Coherent Ultrapulse® 5000 CO 2 laser ( ), the most widely available CO 2 laser in use for LSR today. Users of the new Lumenis Ultrapulse Encore™ are referred to the user’s manual for adjustment of the settings for the new ActiveFx® and DeepFX® pattern generator hand piece in order to achieve the energy and coverage listed below. It is essential that laser fire precautions be observed. Eye protection is mandatory for the patient and all personnel. Smoke evacuation of the laser plume is crucial throughout the procedure.
Most full face CO 2 LSR procedures are done under general anesthesia. Prior to starting the procedure the skin is de-greased, rinsed with saline and dried. The depths of wrinkles, rhytides and acne scars are marked with a surgical marker so that progression of ablation can be observed during treatment. The sub-mandibular border is marked symmetrically by observing the mandible from below so that symmetrical demarcation zones are achieved. Protective stainless steel scleral shields (Oculo-Plastik®, Montreal, Quebec) are placed over the eyeball.
The CO 2 Ultrapulse® Laser with the CPG scanning hand piece is set at 300millijoules, 60 watts, packing density 5, pattern 3, and size 6–9. The first pass is done over the entire face avoiding the eyelids, making certain the ablation patterns are adjacent or with a 5 % overlap to avoid skip areas. The gray char is removed with saline soaked gauze sponges revealing a pink de-epithelialized skin surface. A second, and usually, a third pass are done. If the skin develops a yellowish ‘chamois cloth’ appearance it is an indication of injury into reticular dermis and no further pass should be done. In patients with very deep rhytids individual passes with a smaller pattern can be done on the ‘hillock’ or shoulder of the wrinkle as long as the ‘chamois cloth’ appearance has not developed. More than three passes does not achieve improvement in results and can extend the depth of injury to an unsatisfactory level.
The laser is then de-powered to 150 millijoules and 30 watts and a blending pass is done at the demarcation line on the mandible to ‘blend’ the transition between treated and untreated skin. The eyelids are only one-sixth of the thickness of the facial skin and must not be treated as deeply as the remainder of the face. I use one to two passes at 300 millijoules 60 watts with a packing density of 5 on eyelid skin of average thickness. Thinner skin is treated with 150 millijoules and 30 watts. A smaller pattern 3 size 2–3 is used on the eyelids.
Closure
I apply a mask of Xeroform™ gauze on the facial skin and cover this dressing with thick layer of bacitracin ointment for the first post operative night. I cover the lower eyelid with a supportive Flexan® occlusive dressing and simply apply bacitracin to the upper eyelids. Some practitioners prefer other occlusive agents such as Aquaphor® or Vaseline® due to risk of contact allergy with topical antibiotic ointment. Percocet® tablets are used for pain management.
Operative steps
- •
Place intra-ocular shields
- •
De-grease skin
- •
Three passes facial skin–one to two passes eyelid skin
- •
Cleanse between passes
- •
Apply Xeroform ® dressing with bacitracin or other occlusive agent
- •
Flexan ® supportive lower eyelid dressing
- •
Remove intra-ocular shields.
Fractional CO 2 LSR with the Reliant Fraxel re:pair ® procedure
The Fraxel re:pair® LSR procedure is done under topical or local nerve block anesthesia. Pre-operative preparation has been covered above. I use a topical anesthetic consisting of benzocaine 12%, tetracaine 8%, and lidocaine 4%, compounded by University Pharmacy in Salt Lake City, Utah, which is applied 1 hour prior to the procedure. This compound should not be used on large areas like the leg or body because of potential toxicity; however, use on the face is safe for individuals who do not have sensitivity to these agents. The topical anesthetic is removed only from the treatment area currently being treated leaving the anesthetic on the areas which will be treated later. Other topical anaesthetics such as Pliaglis® (Galderma Labarotories, Ft. Worth, TX) have been introduced that provide excellent topical anesthesia. The face is prepped with sterile solution and then the skin cleansed and de-greased. As in the traditional flat-beam CO 2 LSR procedure above, laser fire precautions, eye protection for patient and staff, and constant smoke evacuation of the laser plume are mandatory laser safety procedures.
I use stainless steel intra-ocular shields when doing ablative CO 2 LSR, although if the eyelids are not to be treated, external shields may be used. The Fraxel re:pair® laser settings below are recommended in the Reliant® user manual and are customized according to skin type and anticipated depth of treatment required. Depth of penetration is determined by pulse energy which can be set from 20 millijoules to 70 millijoules. The second parameter to consider is the percentage of skin surface area coverage of the fractional laser beam which, for the face, is usually set from a low of 25% to a high of 60%. The neck should not be treated with over 35% coverage. Eyelids are thinner than facial skin. Thus the eyelid skin should be treated with lower settings, a maximum of 20 millijoules and no more than 40% surface area coverage. While higher settings of depth and surface area coverage will provide more effective wrinkle removal, higher settings will also increase post LSR erythema and delay recovery.
The Fraxel re:pair® is new technology, and you will experience a definite learning curve. For mild to moderate rhytides and/or pigmentation, I use a 25% surface area coverage and 40 millijoules and four passes, two horizontal and two vertical over the same area at 90 degrees to the prior pass. For acne scarring and deeper rhytids a 40% surface area setting and 50 to 60 millijoules will produce better results, but also prolong erythema time. The Fraxel re:pair® hand piece is a marvellous technological achievement. The two rollers glide easily over the skin, delivering the fractional CO 2 beam in a uniform fashion. Appropriate hand speed is monitored by an automatic audible monitor. Four passes are always done–two horizontal and two vertical in alternating fashion.
Visual feedback is not as important with Fraxel as it is in flat-beam CO 2 laser resurfacing. You have to trust the machine to uniformly deliver the pre-determined energy of your dialled-in settings. Once four passes are completed, you are done–no checking for ‘chamois cloth’ appearance. I do not wipe debris between passes, as there is little debris to visualize and the attached vacuum removes most debris that is created. Note: be sure to remove the intra-ocular shields after the procedure.
Closure
Once the treatment is completed, apply iced or cold saline soaks to the skin. After the patient feels comfortable, apply Aquaphor® ointment. I have the patient continue saline soaks every 2–3 hours the first night, gently removing any debris. The patient then applies Aquaphor® ointment. Percocet® tablets are used for pain management.
Operative steps
- •
Laser safety precautions.
- •
Intra-ocular shields.
- •
Remove topical only from area to be treated.
- •
De-grease skin.
- •
Laser settings – 20–60 millijoules and 25–40% surface area.
- •
Eyelids maximum 20–millijoules 40% surface area.
- •
Four passes – two horizontal, two vertical.
- •
Cold saline soaks.
- •
Aquaphor ® ointment.
- •
Remove scleral shields.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree